3 Reducing the Cost of HIV in Asia
| Reports - Redefining AIDS in Asia |
Drug Abuse
AIDS WILL REMAIN A MAJOR CAUSE OF DEATH FOR WORKING AGE ADULTS
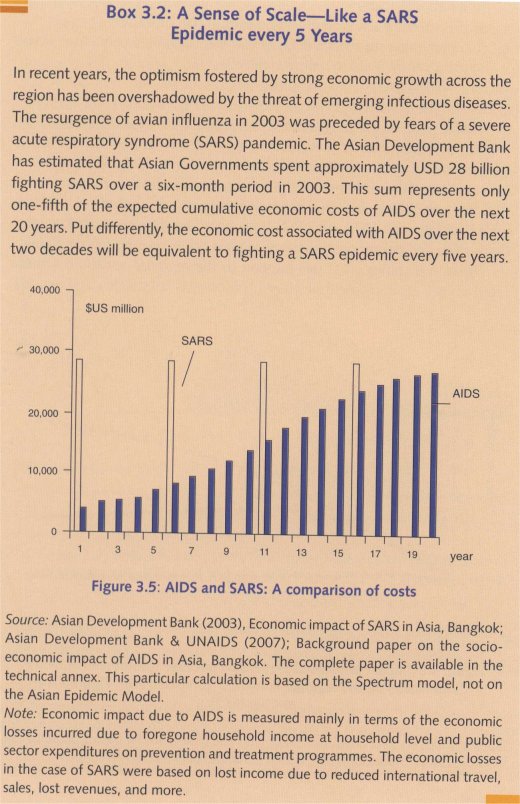
As Asia's economies continue to grow, one of the big unknownsis how infectious disease epidemics will affect the region's economic and social development.1 Avian influenza and Severe Acute Respiratory Syndrome (SARS) have already provoked acute concern in Asia and beyond.
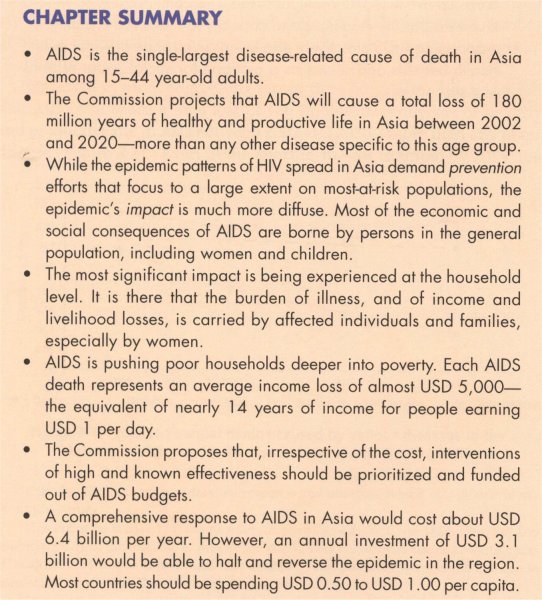
The WHO 2006 study on the burden of disease for Asia shows that between 2015 and 2030, AIDS will be the single-largest disease-related cause of death among adults aged 15-44 years. Adjusting for the recent revision of HIV prevalence estimates for Asia, the Commission found that in the year 2020 alone, almost 0.4 million people in Asia aged 15- 44 years are likely to die of AIDS-related illnesses if current levels and types of HIV interventions continue—more than the projected number of deaths attributable to heart disease in the same year and age group (see Figure 3.1).
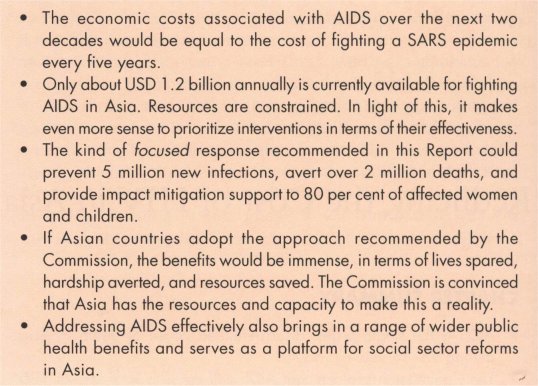
Expressed in more compelling terms, the Commission has projected that AIDS will cause a total loss of 180 million person-years of healthy and productive life in Asia between 2002 and 2020—more than any other disease (Figure 3.2).2 Even in the short term—for example by 2015, the deadline for achieving the Millennium Development Goals—the number of deaths attributable to AIDS will probably match those caused by cancer, as Figure 3.1 shows.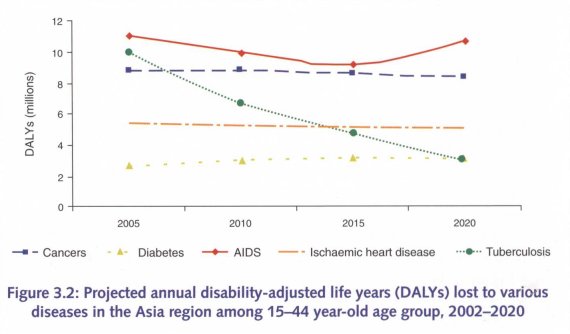
FOCUSED INTERVENTIONS CAN BE PARTICULARLY EFFECTIVE IN ASIA
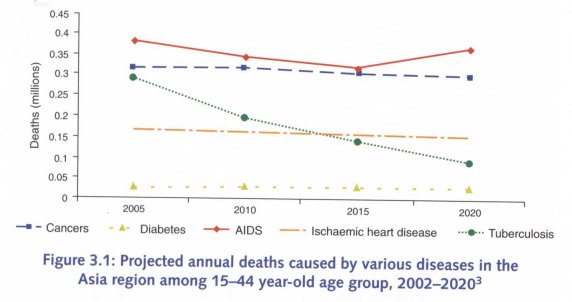
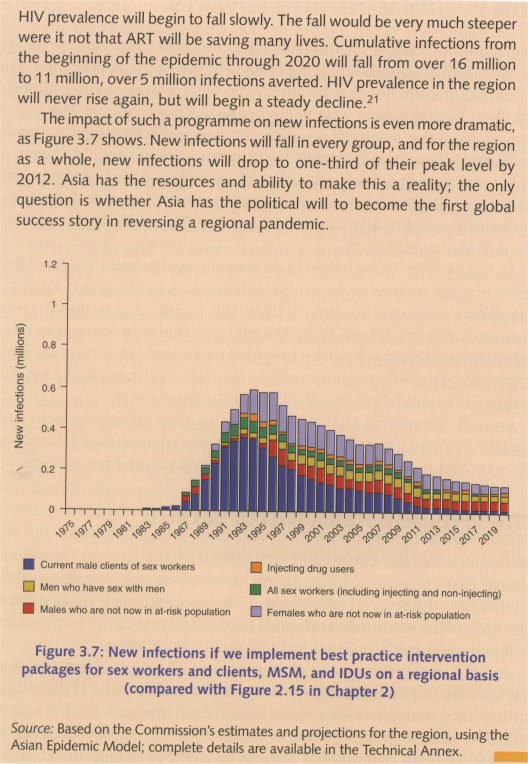
As Figure 3.3 shows, a focused and expanded HIV intervention package could be expected to achieve the following between 2007 and 2020:
• reduce cumulative new infections by 5 million;
• reduce number of people living with HIV in 2020 by 3.1 million; and
• reduce the number of deaths by 40 per cent.
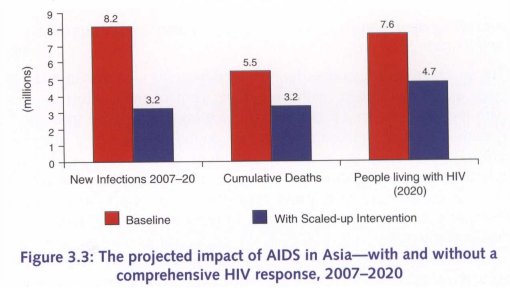
Source: Based on the Commission's projections for the region, using the Asian Epidemic Model.
Note: The 'baseline' scenario in this projection assumes that current HIV programming and effectiveness continue (for example, 30-50 per cent consistent use of condom among sex workers and their clients, while about 25 per cent of people who need antiretroviral treatment receive it). In the 'full intervention' scenario, 80 per cent consistent condom use is achieved among sex workers and clients, there are similarly high levels of risk reduction among men who have sex with men and injecting drug users, and 80 per cent of people in need of antiretroviral treatment receive it.
The argument for investing adequately in the HIV response is compelling.
IMPACT OF AIDS IN ASIA IS LARGELY FELT AT THE HOUSEHOLD LEVEL
The epidemic's impact will register at many levels, most dramatically within affected households and communities. The annual economic cost of AIDS borne by Asian households is estimated to be around USD 2 billion. Introducing a comprehensive intervention package immediately could reduce this cost by 50 per cent over the next decade.17
Although AIDS is the single-largest cause of death from disease among people in their productive prime, the epidemic's impact at the macro-level appears to be negligible. Because national adult HIV prevalence is comparatively low in Asia, AIDS is unlikely to shorten average life expectancy significantly at the national level. Against a backdrop of strong economic growth, the epidemic is unlikely to affect national economic output noticeably or to affect labour productivity in key sectors.18 Even where HIV prevalence is concentrated in certain localities, local economic output probably will not be dramatically affected.
But given the large populations in many Asian countries, even low national infection levels mean that many millions of people will endure the epidemic's impact.
The most significant impact is experienced at the household level. It is there that the burden of illness, and of income and livelihood losses, is borne by affected individuals and families—and especially by their female members. That impact is most harsh in poor households; they lack the income and assets that can help cushion the consequences of AIDS-related illness and death.
A great deal of the damage done by AIDS therefore is concentrated in and around the homes and lives of the poor who, in the absence of formal social protection systems, somehow have to fend for themselves. Such a situation is at variance with the rapid pace of economic growth in Asian countries and the commitments of Asian Governments to ensure a better standard of life for all its citizens.
AIDS has already reduced life expectancy in several Asian countries, albeit by relatively small margins.19 As Figure 3.4 shows, it is estimated that life expectancy in Cambodia in 2005 was three years lower than it would have been in the absence of an AIDS epidemic, while it was 1.7 years lower in Myanmar and 1 year lower in India and 'Thailand.
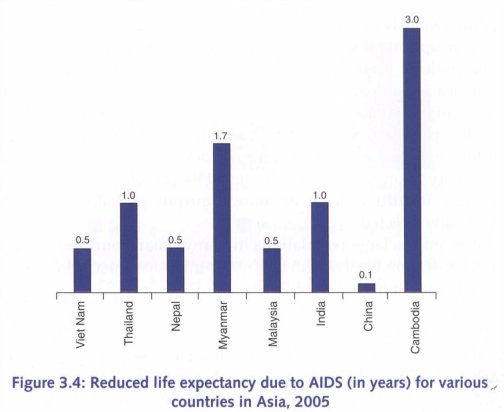
Source: Background study on socioeconomic impact for the Commission, available in the Technical Annex.
THE HUMAN FACE OF AIDS—LOSSES, FOREGONE OPPORTUNITIES, AND SOCIETAL REJECTION
It is difficult to quantify the impact of HIV when children must forego schooling in order to care for parents or kin, when wives caring for HIV-infected husbands are ostracized by their families and communities or when surviving widows are forced to abandon their homes and land.
For example, according to a United Nations Development Programme study in India (2006),2° an estimated 40 per cent of widows leave their in-laws' homes after their husbands' deaths due to AIDS, and 80 per cent of those women are deprived of their property and inheritance rights.
Often, the AIDS stigma cloaks these experiences in silence and secrecy, with families afraid to divulge their plight to neighbours, colleagues, or even relatives. Moreover, because such hardship tends not to be revealed by standard socio-economic and demographic indicators, it often goes unnoticed by policymakers. This will change. Over the course of the next two decades, AIDS is forecast to remain one of the biggest killers of adults in Asia.
AIDS PUSHES MANY INTO POVERTY
The economic effects of AIDS-related illness and death tend to be felt most acutely in households living dose to or below the poverty line. The Commission estimates that, by 2015, AIDS will have caused an additional 6 million households in Asia to fall below the poverty line. The loss of income from the principal wage-earner due to AIDS-related illness or death exacerbates the economic costs endured by households, many of which may already be struggling to make ends meet. It has been estimated that each AIDS death represents an income loss of almost USD 5000 — the equivalent of nearly 14 years of income for people earning USD 1 per day at current prices.
In light of the above, there is a compelling argument for providing antiretroviral treatment for all households as a public good. Thailand has shown this can be done within the ambit of a national social insurance system, where more than 80 per cent of people in need of antiretroviral therapy could be provided treatment. At current levels of antiretroviral need, public provision of HIV treatment and care lies within the financial means of all Asian Governments.
Overall, preventing HIV infections is the most effective way to curb the HIV epidemic, to avoid the burgeoning costs of treating AIDS-related illnesses and to reduce their impact on individuals and households.
THE EPIDEMIC HAS A WIDER IMPACT
While the epidemic patterns of HIV spread in Asia demand prevention efforts that focus to a large extent on most-at-risk populations (as discussed in Chapter 2), the epidemic's impact is much more diffuse. The bulk of the economic and social costs of AIDS is borne by members of the general public, particularly women and children.
As HIV epidemics spread from networks of injecting drug users to sex workers and their clients, the economic characteristics of the people infected also change.22 As already noted, drug injectors tend to belong to lower income groups (often as a consequence of their drug-taking habits), whereas commercial sex clients tend to belong to relatively wealthier segments of society. For example, in Viet Nam, men belonging to the top income quintile were nine times more likely to have paid for sex in the previous 12 months than were men in the lowest quintile. A similar, though less pronounced, correlation was found in India, where HIV prevalence was highest in the second-top income quintile, at 0.5 per cent among adult men.
A similar pattern is evident in Cambodia, where the most recent Demographic and Health Survey (2005) found that 1.3 per cent of men in the lowest household income quintile had paid for sex in the previous year, compared with 12.7 per cent of men in the highest quintile. Simulations done for the Commission indicate that in countries where national adult HIV prevalence is below 0.4 per cent, most people with HIV tend to belong to the lower income groups. As prevalence rises and more clients become infected, the distribution of HIV cases shifts towards wealthier segments of society in the medium-term.
Until now, most people dying of AIDS in Asia have been men, almost all of whom will have acquired HIV when buying sex, having sex with other men, or when sharing contaminated injecting equipment. Only a small percentage of men and women dying from AIDS will have been infected when selling sex. It follows, therefore, that the majority of surviving spouses to date have been female, many of whom will have been unaware of their husbands' HIV status or how their husbands became infected. Their only 'risk' was to have had unprotected sex with their husbands.
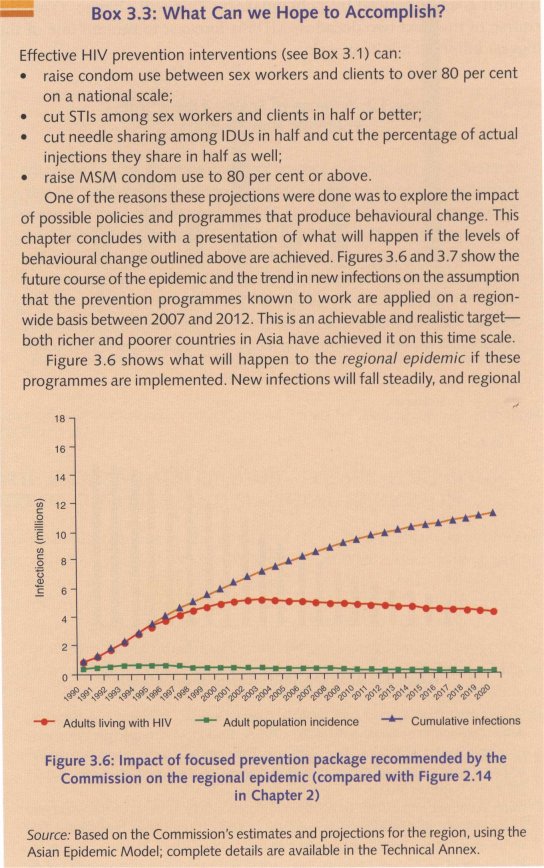
Much of the physical and psychological burden of HIV, the associated loss in household income and other costs associated with AIDS illness and death, is borne by people who do not belong to socially marginalized most-at-risk groups, as shown in Figure 3.6. The majority of people living with HIV are male clients of sex workers. Clients, by definition, are a most-at-risk population. But they are not a marginalized group; for the most part, they are indistinguishable from the 'general' population.
While HIV prevention efforts will be most effective where they focus on such most-at-risk groups, treatment and impact mitigation programmes need to reach all affected men and women. For the same reasons, programmes for preventing the mother-to-child transmission of HIV and voluntary counselling and testing should focus not only on those groups most at risk of infection. This principle has important implications for how services are targeted, financed, and delivered.
Source: The graph is based on the Asian Epidemic Model, and uses standard assumptions regarding the size of most-at-risk groups, HIV transmission dynamics, and the extent of preventive behaviours.
CURBING HIV IN ASIA IS BOTH AFFORDABLE AND ACHIEVABLE
In 2004, UNAIDS estimated that a comprehensive HIV response in Asia would have required an annual investment of USD 5.1 billion in 2007. The package recommended in this Report includes a total of 19 prevention, treatment and impact mitigation interventions, as well as surveillance and programme management activities. The Commission has adapted those estimates on the basis of local costs, while retaining the intervention targets used in the earlier calculations. The Commission's work on the local cost also includes the cost of involvement of community-based organizations an.d of the creation of an enabling environment in delivery of services of prevention, treatment, and impact mitigation.23 Further details of the inputs, assumptions and methodology of these calculations are provided in the tèchnical Annex.
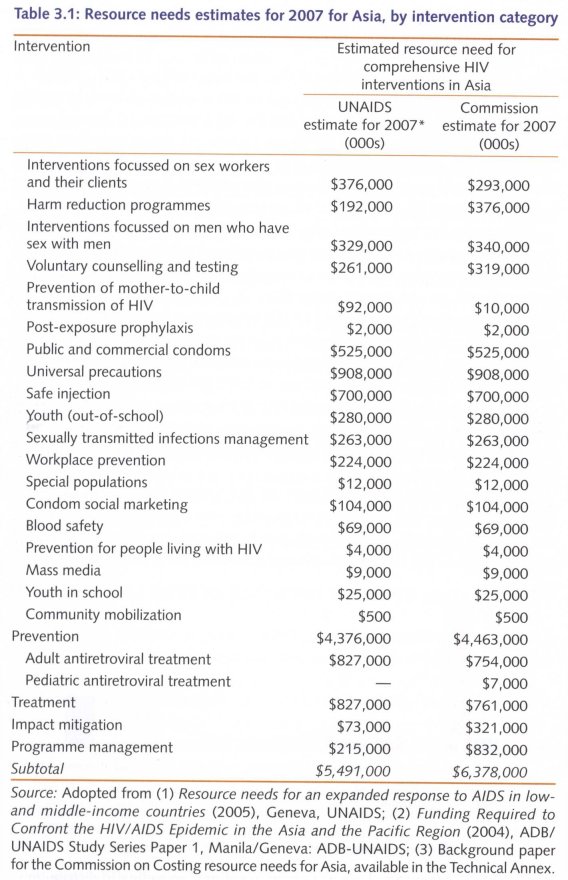
PRIORITIZATION IS ESSENTIAL TO DESIGN A COST-EFFECTIVE PROGRAMME
The Commission then assessed the various components of such a response in terms of their likely impact on the epidemic and in mitigating its effects. This was done by matching the relative costs of interventions against the numbers of HIV infections prevented, the numbers of AIDS deaths averted, and the scale of income losses avoided. The Asian Epidemic Model was used to estimate the outcomes of the proposed interventions based on experiences observed in various best practice cases in Asia.
With regard to prevention, the Commission's analysis indicates that the costlier interventions (such as ensuring blood safety and safe injection) would prevent only about 1 per cent of new HIV infections. But such interventions would absorb more than 25 per cent (USD 1.7 billion of USD 6.4 billion) of the estimated total HIV response budget. On the other hand, the kind of focused response recommended in this Report could prevent 80 per cent of new infections with just 15 per cent of the total HIV response budget (USD 1 billion of USD 6.4 billion).
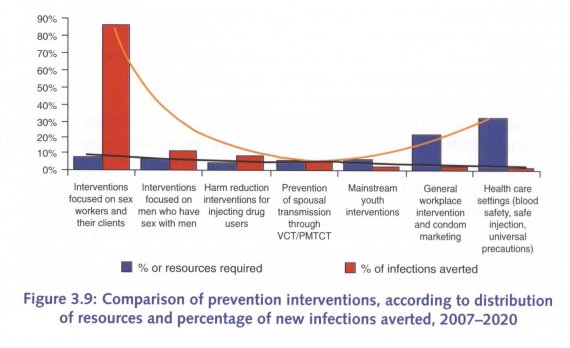
As Figure 3.9 illustrates, several of the interventions currently regarded as integral to a comprehensive prevention strategy under the global framework are best classified as high-cost/low-impact activities, described later in the chapter.
For example, life-skills education for young people tends to be promoted to prevent HIV transmission between young people who do not visit sex workers. Therefore, it would prevent a small percentage of new infections. The Commission's analysis fmds that if such interventions reached a large number of young people, they would cost at least 10 per cent of the total HIV response budget, but would prevent fewer than 1 per cent of new infections.
Nonetheless, the effects on the sexual and reproductive health of young people can be positive and substantial. Therefore, the Commission recommends that AIDS programmes advocate, catalyse, and leverage further resources to cover the cost of programmes such as life-skills education, blood safety, and universal precautions, which should be managed by the relevant administrative ministries in Governments.
Fund-raising efforts should not be relaxed. A projection of current resource availability for Asia shows that only USD 1.2 billion of the USD 6.4 billion needed annually for an effective overall HIV response would be available in 2007.24 Resources are constrained. In light of this, it is wise to assess the various activities included in the response in terms of their effectiveness. It is also sensible to limit the management demands placed on over-burdened AIDS programme managers by focusing resources and energies on interventions that have the largest potential impact.
Bearing that in mind, the Commission then used the Asia Epidemic Model to estimate the cost-effectiveness of various interventions. Its findings highlight the cost-effectiveness of interventions that focus on preventing infections in sex workers and clients. These require as little as USD 3.23 per disability-adjusted life year (DALY); in expanding epidemics, every USD 1 invested in appropriate prevention would save up to USD 8 in averted treatment costs over the next 20 years.
CLASSIFYING INTERVENTIONS BY COST AND IMPACT
Based on the analysis reported above, the Commission has classified HIV interventions into four categories, according to their effectiveness and cost:
• High-cost/High-impact
• Low-cost/High-impact
• Lost-cost/Low-impact
• High-cost/Low-impact
For example, universal precautions and interventions targeting sex workers and their clients tend to be similar in cost but differ considerably with respect to the numbers of HIV infections they prevent. Indeed, when compared with universal precautions, activities focused on sex workers and clients can prevent 7,000 times more new HIV infections for the same amount of money spent. So, not only are interventions targeting sex workers and clients relatively cheap, they are highly cost-effective.
Figure 3.10 shows their cost to be approximately USD 3.23 per disability-adjusted life year saved. In most of Asia's epidemics, these interventions could prevent up to 70 per cent of future HIV infections and save a correspondingly large number of DALYs. They therefore fit in the Low-cost/High-impact category.
Antiretroviral treatment, on the other hand, tends to be quite costly (approximately USD 2,000 or more per DALY saved), but the effectiveness of that intervention is high. Access to a continuum of antiretroviral therapy can save several years of life per person receiving the treatment. This intervention would fit in the High-cost/High-impact category.
The Commission proposes that, irrespective of their cost, interventions of high and known effectiveness should be prioritized and funded out of AIDS budgets. Prevention activities that focus on most-at-risk populations, programmes for preventing mother-to-child transmissiL of HIV, counselling and testing, and antiretroviral programmes fit into this category.'25
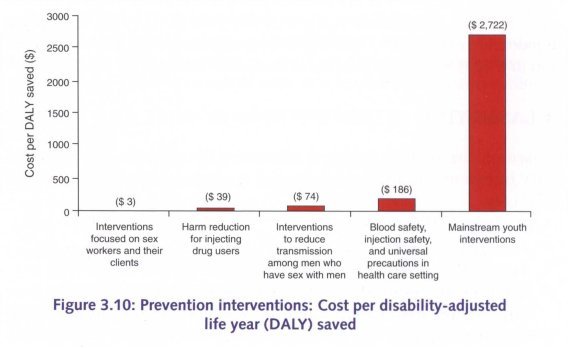
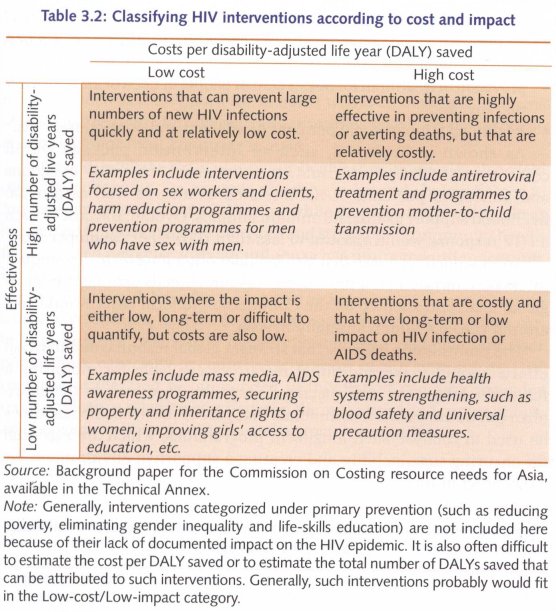
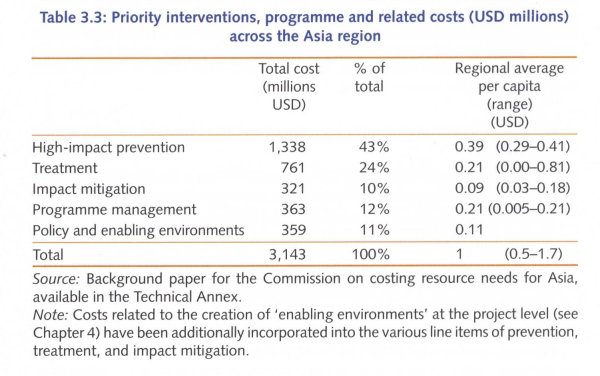
Table 3.3 summarizes a budget for prioritized interventions, which would include:
• High-impact prevention activities: Interventions for sex workers and clients, drug users, and men who have sex with men, as well as focused programmes to prevent mother-to-child transmission and transmission within marriages and relationships;
• Treatment: Comprehensive package of first and second-line antiretroviral therapy, including all laboratory testing and subsidies for transportation;
• Impact mitigation: Livelihood security programmes for AIDS-affected women, and social protection for children orphaned by AIDS;
• Strategic information, surveillance, and monitoring and evaluation;
• Programme management.
Such a priority package would aim to achieve:
• 80 per cent coverage levels for preventing HIV infections in most-at-risk populations and in couples in geographic hot-spots;
• provision of treatment for 80 per cent of people in need of antiretroviral therapy; and
• livelihood support to 80 per cent of affected and poor households.
As shown in Table 3.3, such an intervention package would cost about USD 3 billion, and could avert 60 per cent of new HIV infections and almost 40 per cent of AIDS-related deaths, as well as provide livelihood support to almost 1 million families. Overall, the cost of such a HIV response would amount to less than USD 1 per capita per year.
An expanded response that also includes other long-term, low-impact interventions (along the lines of the resource needs estimates done at global level and adopted by the Commission to local costs) would cost around USD 6.4 billion annually in Asia.
The Commission believes that stronger global resource mobilizatfon efforts should make additional resources available for mounting a full-scale, long-term, and sustained response. However, in the short-term the Commission recommends that part of the available resources be used to catalyse such long-term programmes, which are essential for ensuring sustainability and creating a supportive environment for AIDS programmes.
WITH THE RIGHT CHOICES, HIV EPIDEMICS IN ASIA CAN BE EFFECTIVELY CONTAINED
If the countries of Asia adopt the approaches and programmes recommended in this Report, the benefits would be immense, in terms of lives spared, hardship averted, and resources saved. Such a response is affordable for most countries in Asia.
Efforts to combat a particular public health threat typically also yield other wider benefits. For example, the drive to combat cholera helped to improve sanitation systems in Europe, while the response to tuberculosis has helped improve hygiene practices and strengthen community health facilities, and response to avian influenza has promoted improvements in disease surveillance. Effectively addressing HIV brings a range of wider public health benefits, and serves as a platform for strengthening social development in Asia. Scaling-up national HIV programmes can help to improve health care delivery systems for marginal and poor populations, especially in countries with weak health systems. An HIV response of the kind recommended in this Report can also engender more productive relationships between the authorities and communities, and between various ministries and agencies themselves.
TECHNICAL NOTE
How Much will it Cost to Halt and Reverse the Epidemic?
An Estimation of Priority Resource Needs for AIDS in Asia
The need to estimate the resources required for an effective AIDS response is a vital part of financing as well as mobilizing donor funding that properly addresses and reflects the appropriate national priorities in the region. In the past, global resource needs estimates have been calculated based on a broad spectrum of interventions, without necessarily reflecting the specific components involved or their relative priority and impact in addressing the epidemic.
The typical nature of the AIDS epidemic in Asia and the scenarios presented in Chapter 2 of this Report form a basis for prioritization of the interventions which will have the maximum impact in Asia. Through a review of best practices in HIV prevention and their expected levels of behaviour change, the Commission has suggested a standardization of the elements of intervention packages for important populations in Asia, the necessary coverage needed, the unit costs and the expected behavioral and epidemiological outcomes of these interventions, including their cost effectiveness. The results of this analysis have been presented in this chapter. This note explains the methodology used to generate the Commission's estimated priority resource needs for a high impact and effective AIDS response in the region.
It is important to note that the resource needs estimates presented here are based on regional averages and should be adapted by each country according to their own national and sub-national epidemic situation, local costs, and other local data.
The main steps involved in the estimation of resource needed for this Report are as follows:
• Characterizing the current phase of the epidemic for each country;
• Defining the package of interventions with maximum effectiveness for these countries in terms of population groups to be reached by prevention, treatment, care, and impact mitigation;
• Specifying the activities required for each intervention;
• Assessing the unit cost of such interventions on a regional basis;
• Estimating the resource needs for population-specific services by multiplying the average unit cost of services to one person by the size of the population to be reached;
• Summing the total costs and gains due to these interventions to get a regional average;
• Recommending a resource allocation norm for the region based on the calculation of the per capita resource need arrived above.
Phase of the epidemic
Following the four scenarios described at the end of Chapter 2, each country in this region has been classified as latent, expanding, maturing or declining. Based on the current epidemiological situation, no countries were classified into the maturing phase. The populations of the countries classified into each scenario were then summed to find the total population in each. This gave population sizes of 439 million in the latent phase, 2.87 billion in the expanding phase, and 79 million in the declining phase. Sub-national variations within countries were not taken into account for this rough estimation at regional level.
Most effective intervention package
The package of population-specific interventions that will produce a maximum prevention effect was presented in the technical note for Cha,pter 2 based on an Asian Epidemic Model for each of the four scenarios. In summary, all countries required interventions among IDUs, sex workers, and clients, and the MSM population except that in latent countries the MSM intervention was not factored in because prevalence among these men is assumed to be extremely low. If national MSM prevalence is already growing significantly, then this should be added even in the latent countries. Effective prevention strategies to target and reduce spousal transmission have yet to be developed in Asia despite the urgent need for them, but for the purposes of this estimation, the necessary costs of voluntary counselling and testing, and prevention of mother-to-child transmission services are added to all country scenarios. Voluntary counselling and testing will be an important component of any interventions to prevent transmission within married couples.
Treatment needs are estimated from the Asian Epidemic Model for each scenario. The need for first line and second line ART has been calculated based on an eight year average period between acquiring HIV infection and need for treatment, with an average survival of 3 years after this if no treatment is provided.26 After initiating first line antiretroviral therapy, it is assumed that 15 per cent will fail in the first year and 5 per cent every year thereafter creating a need to move them onto second line ART. Thus, in 2007, fewer than 1,000 people in the latent scenario countries, 955,000 in expanding, and 84,000 in declining scenario countries required first line ART. Second-line therapy was estimated to be required just over 55,000 and 5,000 persons in the expanding and the declining scenario countries, respectively.
A comprehensive impact mitigation programme in addition to ART for positive men and women was targeted at families of positive men with affected women and children being recruited through community organizations and the women being linked with income generating programmes. Cash transfers were assumed to be provided for foster families supporting children who were orphaned by AIDS. A ree'ent estimate using weighted averages from several countries in the region, estimated that approximately 1 million orphans in the region are in need of such familial support.27
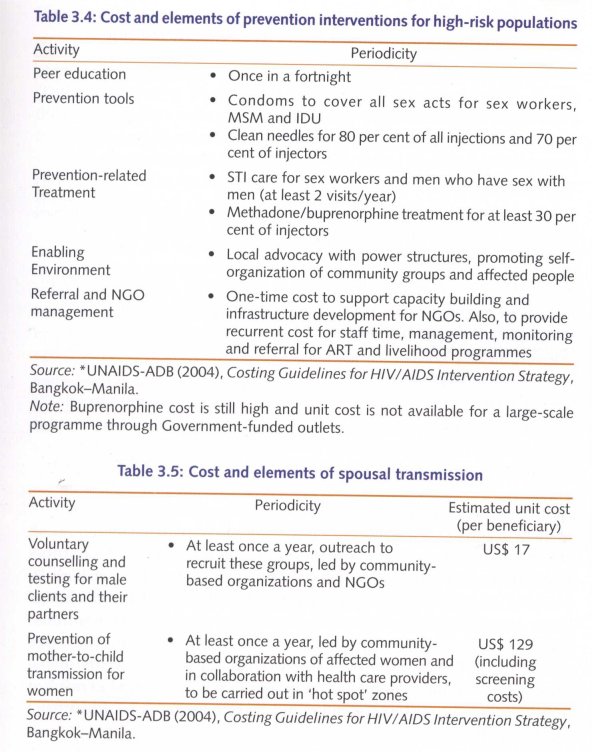
Activities required for each intervention
Based on an analysis of existing best practices in the region, the standard minimum elements of interventions were extracted and their approximate cost was calculated, based on local knowledge and evidence. All three programme areas, that is, prevention, treatment, and impact mitigation, have common elements of peer education, management and capacity building for non-governmental and community-based organizations at project level, and creation of an enabling environment at local level along with commodities and supplies for prevention and treatment. These elements, as they pertain to the most effective intervention packages outlined above, and the costs of each element, are outlined in Tables 3.4 and 3.5 below.
Unit cost: The unit costs for each of the intervention packages were then calculated based on a review of local best practices in these programmes, which include the essential elements of prevention, treatment, and impact mitigation programmes (described further in Chapter 5 and outlined in Tables 3.4-3.6).28
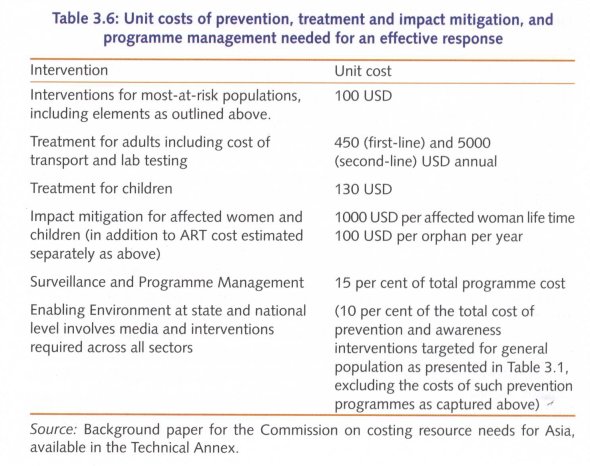
Coverage
Modelling and empirical evidence have demonstrated that if interventions reach at least 80 per cent of the target population of most-at-risk populations, the programme induces behaviour change in at least 60 per cent of the population—leading to the levels of behaviour change documented in a box earlier in this chapter and exceeding the minimum level needed to reverse the epidemic's upward trend. By the same reasoning, then, prevention of mother-to-child transmission, antiretroviral therapy, and impact mitigation programmes are all targeted to reach at least 80 per cent of the targeted population to ensure a lasting impact on the epidemic.29
Total and average cost
Using the steps described, then, the total annual cost of each component of an effective response in Asia was calculated in each of the scenarios (Latent, Expanding, Maturing and Declining) by multiplying the size of the target population for that component by the unit cost of the respective interventions. After the total prevention, care and impact mitigation costs were derived, a per capita cost was calculated for each of the areas (prevention, treatment, impact mitigation) in each of the scenarios by summing across all programme components.
In addition to these essential components for an effective response in Asia, there are several additional prevention interventions targeted at the general population like those for lower-risk young people, blood safety, etc. which may have little direct impact in reducing new infections or deaths, but which are important to the creation of an enabling environment. These components were itemized in the estimation of resource needs according to the global estimation procedures and calculated to cost USD 3.6 billion annually. Ten per cent of the costs of these less effective interventions was included in the priority response to ensure actions are catalysed and to enlist the collaboration and cooperation of relevant ministries and sectors that must deliver these services. The other 90 per cent is assumed to be additionally mobilized as more resources become available.
Programme management, including surveillance and strategic information, monitoring and evaluation, and administrative management was calculated as an additional 15 per cent on the cost of the programme.
Instead of country specific models, a regional AEM for a standard 100 million population was run for each of the four scenarios described, and the per capita costs calculated in that scenario. These per capita costs were then multipled by the size of the total population in the countries classified into that scenario and summed across scenarios to get the total regional response cost.
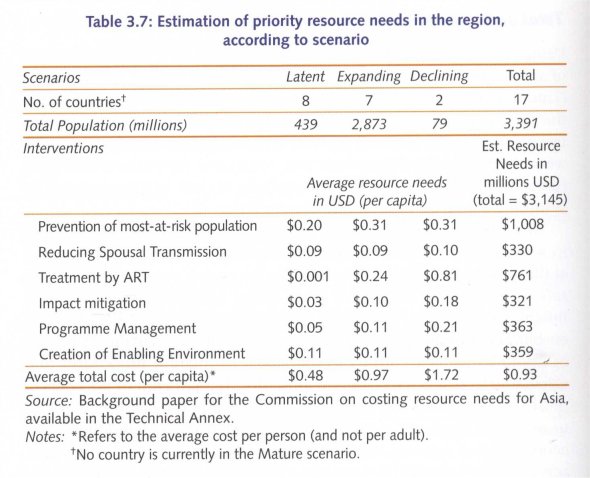
Table 3.7 presents the per capita costs and relevant population sizes in each scenario, providing an overview of the calculation of the overall annual priority resource need of USD 3.1 billion.
The result shows that the average cost of prevention for most-at-risk populations varies between USD 0.2 to USD 0.3 per capita, ART cost USD 0.1 to USD 0.8 per capita and impact mitigation between USD 0.03 and USD 0.2 per capita with overall per capita response cost varying between USD 0.5 in the latent scenario countries to USD 1.7 in the declining epidemic countries with a regional average of USD 1. Although this figure offers a regional estimate, cost for every country, state, province, and district will vary depending on the environment, the nature of the local epidemic, and the understanding of the need for a comprehensive but focused response.
It is estimated that successful implementation of a package funded at this level will reach 80 per cent of the most at-risk populations for prevention, provide ART for 80 per cent of those in need, and mitigate the impacts of HIV on 80 per cent of families, women, and children affected by AIDS. It will achieve a reduction in new infections of 60 per cent and reduce deaths by 40 per cent. This will reverse the regional epidemic as seen earlier in this chapter and will provide the essential ART and impact mitigation programmes needed to keep people living with HIV healthy and productive.
1 This chapter incorporates detailed research and analysis, which is available in the lèchnical Annex.
2 This estimate is based on the number of disability-adjusted life years (DALYs) and potential years of life lost due to premature death. DALYs measure the equivalent years of 'healthy' life lost due to poor health or disability, and potential years of life lost due to premature death. One DALY equals one lost year of 'healthy' life.
3 The estimates presented here are based on the apex study on burden of disease carried out by WHO and published in 2006 (C. Mathers and D. Loncar, Global Mortality and Burden of Disease Projections 2002-2030, PLoS Medicine, 3 [in, pp. 2012-30). That study did not yet take into account the subsequent revisions of HIV figures in Asia, principally in India. Applying a downward adjustment in line with the revisions for India and Cambodia, and using Asian Epidemic Model projections, AIDS remains the largest cause of death and disability-adjusted life years (DALYs) lost due to disease in Asia, in the absence of effective prevention and treatment interventions.
4 S. Jana and B. Banerjee (1997), A dream, a pledge, a fulfillment-Five years stint of STD/ HIV intervention programme at Sonagachi, Calcutta: All India Institute of Hygiene and Public Health.
5 1. Basu, et al. (2004), 'HIV Prevention Among Sex Workers in India', Journal of Acquired Immune Deficiency Syndrome, 36 (3), pp. 845-52.
6 W. Rojanapithayakorn and R. Hanenberg (1996), 'The 100 per cent condom programme in Thailand [editorialr, AIDS, 10 (1), pp. 1-7.
7 UNAIDS-AIDS Division, Ministry of Public Health, Thailand (2000), Evaluation of the 100% Condom Programme in Thailand, Geneva: UNAIDS, available at Publication/IRC-pub01/JC274-100pCondom_en.pdf.
8 W. Sittitrai, et al. (1994), 'A survey of Thai sexual behaviour and risk of HIV infection [lettery, International Journal of STD and AIDS, 5 (5), pp. 377-8.
9 V. Thongthai, and R Guest (1995), 'Thai sexual attitudes and behaviour: results from a recent national survey', Gender and sexuality in modern Thailand, Australia National University, July.
10 UNAIDS (2001), Case Study, Geneva, Joint United Nations Programme on AIDS (UNAIDS) AIDS Division, Thailand: Ministry of Public Health, 1-47.
11 National Centre for HIV/AIDS, Dermatology and STDs (2003), Cambodia Behavioural Surveillance Survey.
12 Z. Wu and Z. Chengzheng (2007), 'Update of Harm Reduction in China', presented at the International Conference on Harm Reduction, Warsaw.
13 C. Hangzo, et al. (1997), 'Reaching out beyond the hills: HIV prevention among injecting drug users in Manipur, India', Addiction, 92 (7), pp. 813-20.
14 A.M. Foss, et al. (2007), 'Could the CARE-SHAKTI intervention for injecting drug users be maintaining the low HIV prevalence in Dhaka, Bangladesh?', Addiction, 102 (1), pp. 114-25.
15 J.H. Herbst, et al. (2005), 'A Meta-Analytic Review of HIV Behavioral Interventions for Reducing Sexual Risk Behaviour of Men Who Have Sex With Men', Journal of Acquired Immune Deficiency Syndrome, 1 June, 39 (2), pp. 228-41.
16 Waria is a Bahasa-Indonesia term, which refers to transgenders.
17 The simulation model used by the Commission shows that foregone income at the household level (due to loss of earnings of both patients and caregivers due to illness, healthcare-related expenses, loss of income due to premature death, funeral costs, etc.) totals about USD 2 billion annually. A full and comprehensive intervention programme starting in 2007, could halve that to about USD 1 billion by 2020. In contrast to earlier studies in the region, loss of income due to premature death has been calculated for only five years, in line with similar assumptions made in recent studies in Africa. The methodology and detailed findings are available in the background study on socio-economic impact for the Commission, in the lèchnical Annex.
18 A comparison of life expectancy, Gross Domestic Product, Gross National Product, and workforce losses, is provided in the Ièchnical Annex.
19 Life expectancy at birth measures the average number of years that a new-born child would live if mortality rates remained constant throughout his or her lifetime.
20 B.K. Pradhan and R. Sundar (2006), Gender impact of HIV and AIDS in India, New Delhi: UNDP.
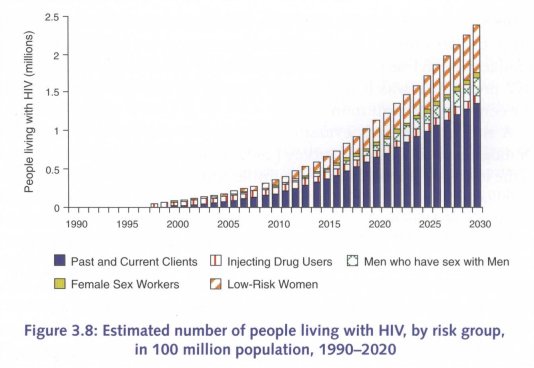
21 These estimate figures differ from the numbers quoted earlier in this chapter, because this estimate is inclusive of several additional countries and has different assumptions about treatment scale-up.
22 About 70 per cent of all people living with HIV in Asia are in countries where the epidemics are driven mainly by sex work.
23 Except for impact mitigation, in which case the Commission has set its own target of 80 per cent coverage for all affected households, as shown in Table 3.1.
24 UNAIDS Global Resource Tracking Consortium (2004), 'Financing the expanded response to AIDS', UNAIDS, Prepublication Draft.
25 Although most of the funds for antiretroviral drugs should be borne by the AIDS budget, other infrastructure and human resource costs should be absorbed by the general health budget. This would serve the larger purpose of integrating these interventions into the general health delivery system.
26 This is consistent with the current recommendation for estimating ART need set by UNAIDS Reference Group.
27 Background paper for the Commission on children vulnerable to and orphaned by AIDS; complete paper is available in the Technical Annex.
28 A review of unit costs and cost-effectiveness analyses in the region s presented in the technical Annex.
29 Coverage for voluntary counselling and testing is targeted for those male clients who can be approached in clusters (for example mobile, migrant worker, sailors) or through existing testing networks like client initiated voluntary counselling and testing programmes or programmes for prevention of mother-to-child transmission. This will mean reaching approximately 1 per cent of adult male population and their female partners. The number of pregnant women who are positive is estimated based on the newly revised number of people living with HIV in the region.
| < Prev | Next > |
|---|












