Appendix to report 4: country reports THE NETHERLANDS
| Reports - A Report on Global Illicit Drugs Markets 1998-2007 |
Drug Abuse
THE NETHERLANDS
1 General information
Location:
Western Europe, bordering the North Sea, between Belgium and Germany
Area:
41,526 sq km
Land boundaries/coastline:
1,027 km / 451 km
Border countries:
Belgium 450 km, Germany 577 km
Population:
16,645,313 (July 2008 est.)
Age structure:
0-14 years: 17.6% (male 1,496,348/female 1,427,297)
15-64 years: 67.8% (male 5,705,003/female 5,583,787)
65 years and over: 14.6% (male 1,040,932/female 1,391,946) (2008 est.)
Administrative divisions:
12 provinces
GDP (purchasing power parity):
$645.5 billion (2007 est.)
GDP (official exchange rate):
$768.7 billion (2007 est.)
GDP- per capita (PPP):
$39,000 (2007 est.) (CIA The World Factbook)
Drug research
Drug research in the Netherlands is extensive and covers many domains. Funding of drug-related research is to a large extent delegated to intermediary agencies, although ministries and municipalities may also directly fund research. Many academic institutions are involved in drug research, such as the universities of Nijmegen, Maastricht, Utrecht, Leiden and Rotterdam). Other research institutes include IVO (Institute for Addiction Research), AIAR (Amsterdam Institute for Addiction Research), Trimbos Institute and CVO (Centre for Addiction Research). Some of them involve cooperation between a university and researchers from institutes for addiction care. Finally, there are also several private institutes involved in drug research, as e.g. Bureau Driessen and Intraval. The national focal point is integrated in the so-called National Drugs Monitor hosted by the Trimbos Institute (Country overview; Van Laar et al., 2008).
Main drug-related problems
The Netherlands is facing a three-fold drugs problem: production (mainly Ecstasy and cannabis herb), trafficking (mainly transhipment of cocaine and cannabis resin and export of cannabis herb) and consumption (cannabis, ATS (mainly ecstasy), cocaine and heroin).
2 Drug problems
2.1 Drug supply
2.1.1 Production
The Netherlands are one of the world’s largest producers of ecstasy, and to a lesser extent amphetamines as can be assumed from data on seizures and dismantling clandestine laboratories. Between 1996 and 2006, 25 countries reported the dismantling of a total of 581 ecstasy laboratories to UNODC. The largest numbers of ecstasy laboratories were reported in the Netherlands (161), followed by the USA (139), Canada (104), Australia (41), Belgium (34), UK (18), and Germany (17). The number of laboratories discovered in the Netherlands and Belgium peaked in 2000 and has since declined (UNODC, 2008).
In 2006, the National Crime Squad carried out 22 investigations into synthetic drugs and 23 production locations were dismantled in 2006, nine of these laboratories were producing amphetamines and five laboratories were producing MDMA. Finally, 52 warehouses of hardware and precursors were dismantled. Most production locations were found in the west and the south of the Netherlands (Country overview).
A proxy indicator of production is the reported origin of amphetamine seizures as identified (“mentioned”) by States Members. Europe as a whole accounts for nine of the top 10 counties of origin. On this basis, the country receiving the most ‘origin’ mentions is the Netherlands (67 or 28% of such mentions), followed by Poland (41 or 17%), Belgium (24 or 10%), and the Baltic region (Lithuania, 7%, and Estonia, 5%). Comparing these results with those of previous years suggests that the importance of the Netherlands, Belgium and Germany as producers of amphetamine has been declining (UNODC, 2008).
Europe remains the main illicit manufacturing region for MDMA globally, with the Netherlands and Belgium the most commonly cited ‘source’ countries. However, as manufacture continues to shift and spread, the importance of these territories as source countries is declining. A shift in ecstasy labs has been identified since 2003, with an increase in North American labs (USA and Canada) and a decrease in European labs (principally the Netherlands and Belgium) (UNODC, 2008).
The largest ecstasy seizures in 2006 were reported by the USA (26%), followed closely by the Netherlands (24%), then Australia (12%), Canada (8%), the UK (7%), Turkey (4%) and France (3%) (UNODC, 2008).
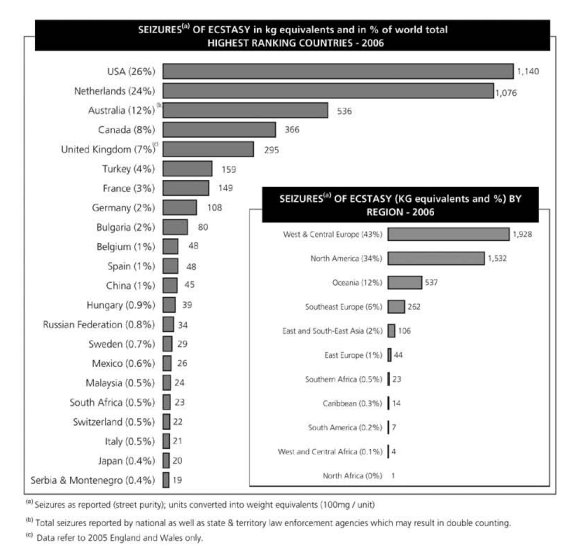
(UNODC, 2008)
The Netherlands and Switzerland are the major producers of cannabis herb in Europe (EMCDDA, 2008). According to UNODC the Netherlands are the largest producers of cannabis herb in West and Central Europe (22% of all European countries saw the Netherlands as their main source of cannabis herb in 2006) (UNODC, 2008).
Yet, it is unclear how much of this production is for the domestic market and how much is exported. There have been for instance some seizures of ‘netherweed’ in the United Kingdom, Scandinavia, Germany, Belgium and France (EMCDDA, 2008; Legget and Pietschmann, 2008). The extent of this export remains unclear (KLPD-IPOL, 2008; Fijnaut and de Ruyver, 2008). Cannabis resin coming from the Netherlands most probably is transhipped from Morocco through the Netherlands to other countries. Cannabis resin is barely produced in The Netherlands (UNODC, 2007; KLPD-IPOL, 2008).
Estimated market value (2007 data)
Ecstasy retail price per tablet: €2.75
Amphetamine: €6 per gram
Cocaine: €45 per gram
Heroin: no report (estimate €35 per gram)
Cannabis: “nederwiet” in coffeeshops €7.30 per gram (Van Dijk, 2008).
2.1.2 Trafficking
The Netherlands has a pivotal position within international trade and thus plays a major role as a drug market and more importantly as a transit country for heroin and cocaine. The supply of heroin to Europe, including the Netherlands, is mainly dependent on the production of opium in Afghanistan. The Netherlands is an endpoint of the Balkan route, and heroin is distributed to other countries from the Netherlands, especially Belgium, France and the UK. Cocaine is supplied from Latin America to Europe. The Caribbean countries, in particular the former Dutch colonies, play a major role in the trafficking of cocaine. In recent years, the role of the maritime trade for cocaine trafficking has decreased while trafficking by air has gained importance (Country overview).
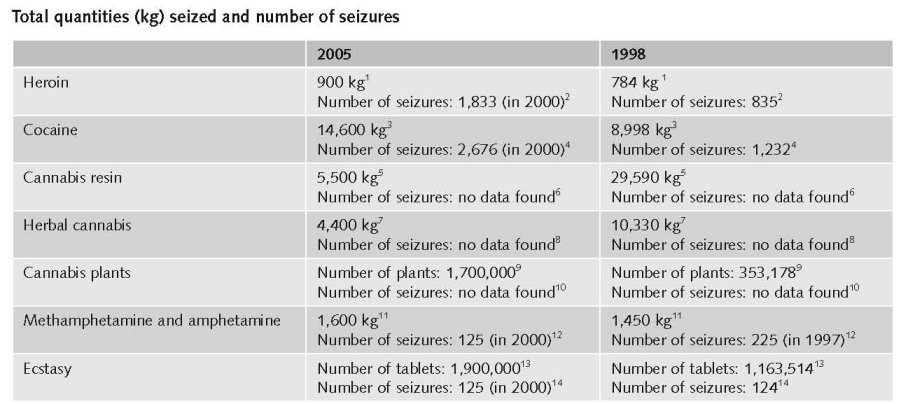
Data on drug seizures in the Netherlands are not registered centrally, but instead the National Police Agency annually collects data from the regional police departments, customs, the Royal Military Police, as well as from the Synthetic Drugs Unit (now part of the National Police Force). Underreporting and the lack of a uniform registration system hamper the quality of the data collected and thus trends may be influenced by collection strategies and investigation efforts. In 2006, 71% of the total quantity of drug seizures related to ecstasy tablets, followed by 28.6% for cannabis seizures (Country overview).
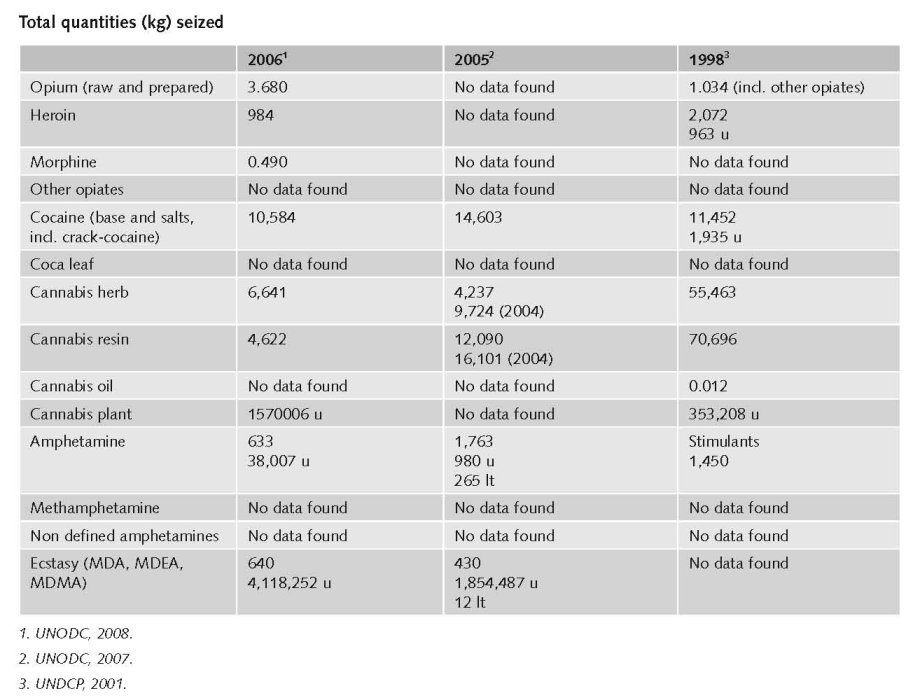
In the Netherlands Drug Situation 2007, the following data can be found (for 2006):
Cannabis (hash and weed) 11,000 kg
Heroin 1,000 kg / methadone 11,600 tablets
Cocaine 10,600 kg
Amphetamines 600 kg + 38,100 tablets + 3 kg paste
XTC/MDMA/MDA/MDEA 700 kg + 4,118,300 tablets +100 litres (Van Laar et al., 2008).
1. Quantities (kg) of heroin seized, 1995 to 2005 - EMCDDA Table SZR-8-SEIZURE-HEROIN-QUANTITY.htm
2. Number of heroin seizures, 1995 to 2005 - EMCDDA Table SZR-7-SEIZURE-HEROIN-NUMBER.htm
3. Quantities (kg) of cocaine seized, 1995 to 2005 - EMCDDA Table SZR-10-SEIZURE-COCAINE-QUANTITY.htm
4. Number of cocaine seizures, 1995 to 2005 - EMCDDA Table SZR-9-SEIZURE-COCAINE-NUMBER.htm
5. Quantities (kg) of cannabis resin seized, 1995 to 2005 - EMCDDA Table SZR-2-CANNABIS-QUANTITY.htm
6. Number of Cannabis resin seizures, 1995 to 2005 - EMCDDA Table SZR-1-SEIZURE-CANNABIS-NUMBER.htm
7. Quantities (kg) of herbal cannabis seized, 1995 to 2005 - EMCDDA Table SZR-4-SEIZURE-HERBAL-CANNABIS-QUANTITY.htm
8. Number of herbal cannabis seizures, 1995 to 2005 - EMCDDA Table SZR-3-SEIZURE-HERBAL-CANNABIS-NUMBER.htm
9. Quantities (number of plants) of cannabis plants seized, 1995 to 2005 - EMCDDA Table SZR-6-SEIZURE-CANNABIS-PLANTS-QUANTITY.htm
10. Number of seizures of cannabis plants, 1995 to 2005 - EMCDDA Table SZR-5-SEIZURE-CANNABIS-PLANTS-NUMBER.htm
11. Quantities (kg) of amphetamine seized, 1995 to 2005 - EMCDDA Table SZR-12-SEIZURE-AMPHETAMINES-QUANTITY.htm
12. Number of amphetamine seizures, 1995 to 2005 - EMCDDA Table SZR-11-SEIZURE-AMPHETAMINE-NUMBER.htm
13. Quantities (tablets) of ecstasy seized, 1995 to 2005 - EMCDDA Table SZR-14-SEIZURE-XTC-QUANTITY.htm
14. Number of ecstasy seizures, 1995 to 2005 - EMCDDA Table SZR-13-SEIZURE-XTC-NUMBER.htm
2.1.3 Retail/Consumption
The retail price of herbal cannabis increased by 18% from 2006 to 2007. Possibly this increase is related to intensified efforts to combat large-scale cannabis cultivation, which may have hampered the supply of herbal cannabis in coffee shops. Retail prices of other drugs have not changed significantly over the past three years. In 2006, the price of an ecstasy tablet varied between €1 and €10 and the price of cocaine between €30/gram and €60/gram. Amphetamine is much cheaper than cocaine, and costs between €3/gram and €10/gram which is sometimes a reason why it is used as a replacement for cocaine (Country overview).
Market retail value
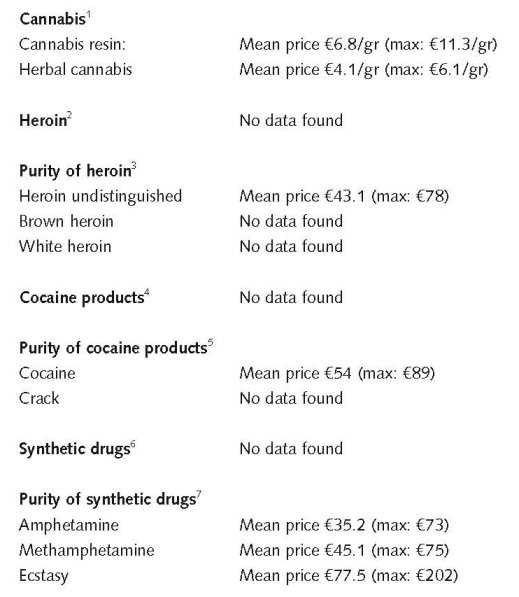
1. Price of cannabis at retail level, 2005 - EMCDDA Table PPP-1 Part (i)-PRICE-CANNABIS.htm
2. Price of heroin at retail level, 2005 - EMCDDA Table PPP-2 Part (i)-PRICE-HEROIN.htm
3. Purity of heroin at retail level, 2005 - EMCDDA Table PPP-6 Part (i)-PURITY-HEROIN.htm
4. Price of cocaine products at retail level, 2005 - EMCDDA Table PPP-3 Part (i)-PRICE-COCAINE.htm
5. Purity of cocaine products at retail level, 2005 - EMCDDA Table PPP-7 Part (i)-PURITY-COCAINE.htm
6. Price of synthetic drugs at retail level, 2005 - EMCDDA Table PPP-4 Part (i)-PRICE-SYNTHETIC.htm
7. Purity of synthetic drugs at retail level, 2005 - EMCDDA Table PPP-8 Part (i)-PURITY-SYNTHETIC.htm
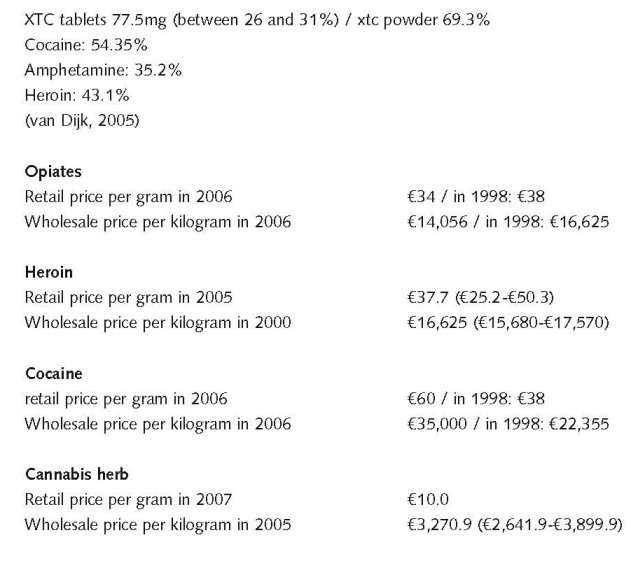
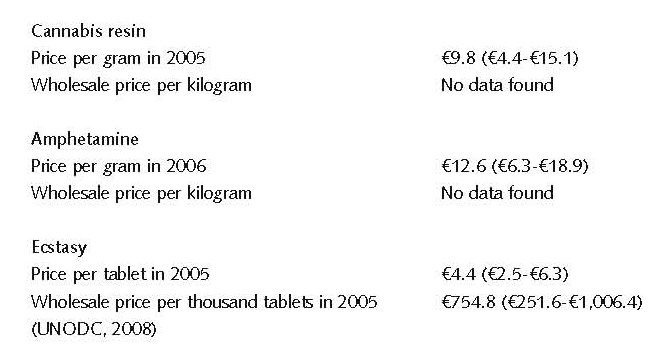
Market data show that the average THC concentration in Dutch home-grown marihuana bought in coffee shops peaked in 2004 (20%), levelled off in 2005 and 2006 (18% in both years) and decreased in 2007 (16%). In 2007 a drop in the percentage of THC in imported hashish was found as well. In 2007 the price of Dutch marihuana increased significantly, which may be related to the intensified actions of police and justice to combat large-scale cannabis cultivation (Van Laar et al., 2008).
2.2 Drug Demand
2.2.1 Experimental/recreational drug users in the general population
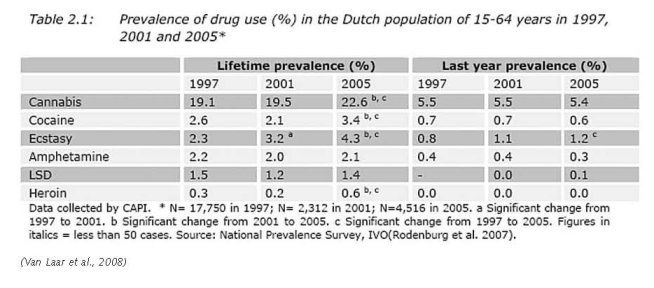
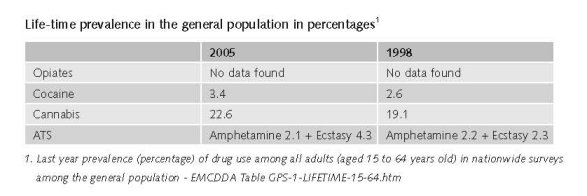
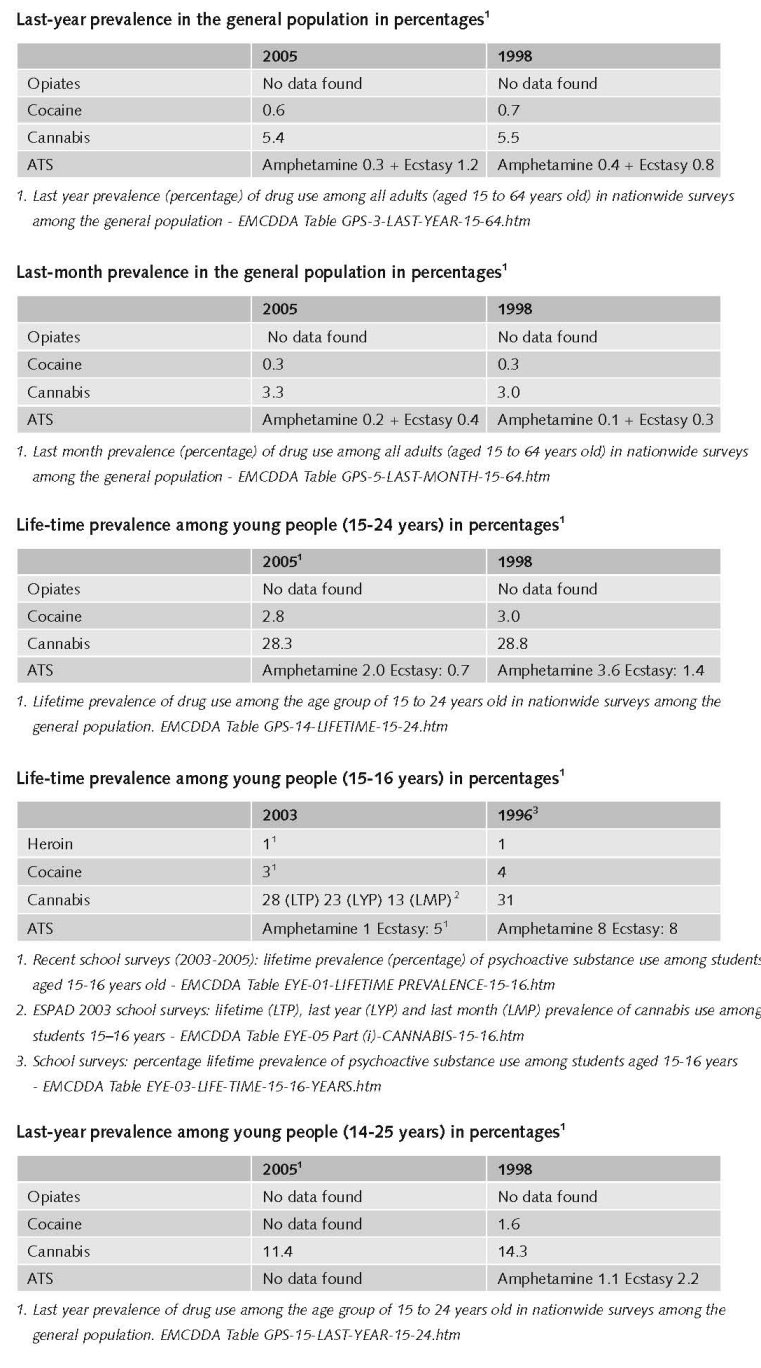
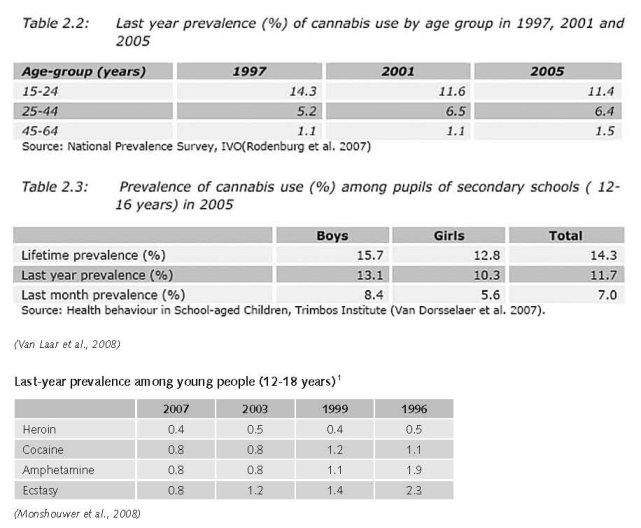
Life-time prevalence in the general population
National prevalence surveys on drug use were carried out in the Netherlands in 1997, 2001 and 2005 among the general population, 15–64 years. In 2005, 22.6% of respondents reported lifetime prevalence of cannabis (compared to 19.5% in 2001 and 15.6% in 1997). Lifetime prevalence of ecstasy use (4.3%) increased significantly compared to previous years, and last year prevalence of ecstasy increased as well. Lifetime prevalence of cocaine and heroin increased significantly compared to 1997 (Country overview).
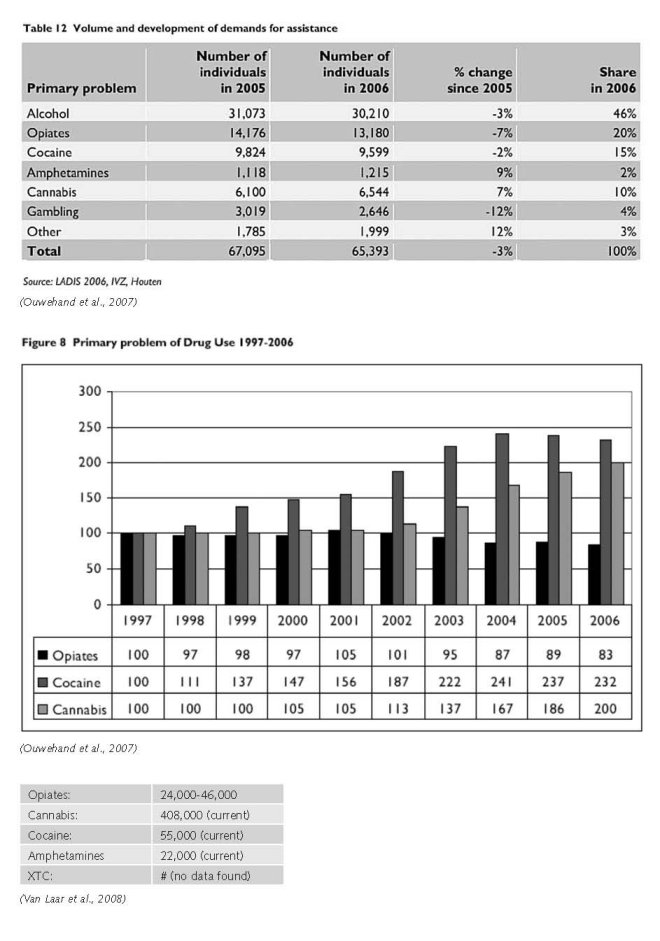
(Ouwehand et al., 2007)
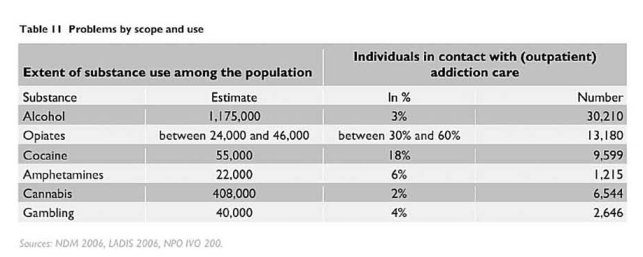
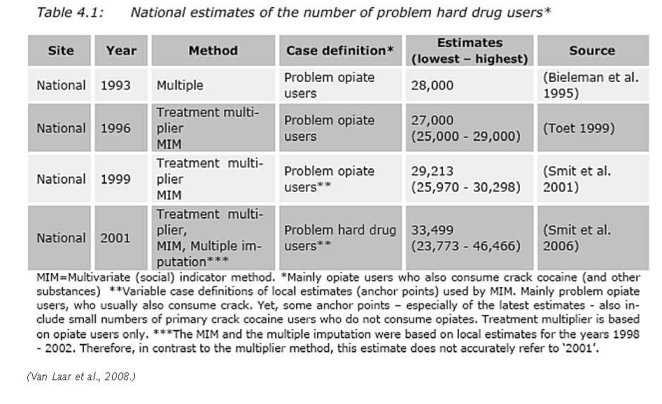
The latest figures from the National Drugs Monitor show that the average estimate of hard drug users comes to around 33,500 with a range of 24,000 to 46,000 (2001 estimate). The line between recreational and problematic use cannot be derived from these figures.
For alcohol and cannabis, the number of demands for assistance in relation to use is strikingly low, while estimates show that 10% of the Dutch population between 16 and 69 years of age are problem drinkers. Demands for assistance in relation to estimated use are also relatively low for cannabis. Demands for assistance have been increasing in numbers, however, and there is a lot of poly drug use among problematic cannabis users (Ouwehand et al., 2007).
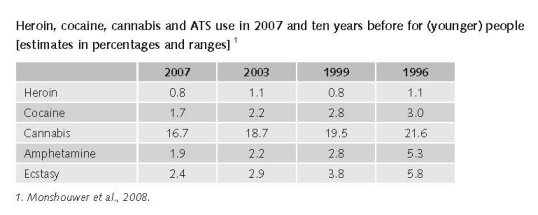
The Youth Health Survey, a school survey among students aged 15–16, was carried out in 1988, 1992, 1996, 1999 and 2003. The results concerning illegal drug use show an increasing trend for cannabis use since 1988, which stabilised between 1996 and 2003. In 2003, the lifetime prevalence rate of cannabis use was 28%. The percentage of pupils using other drugs such as ecstasy, amphetamines, cocaine or heroin is much lower. Inhalants were the most popular, with lifetime prevalence reported at 6%, followed by ecstasy (5%), cocaine (3%), LSD (2%) and heroin (1%). Lifetime prevalence for the consumption of hallucinogenic mushrooms was reported at 2%.There are different hypotheses concerning the stabilisation of drug use in recent years, and some of them focus on the influence of prevention programmes, the changes in demographic characteristics of the school population (increase in non-Dutch ethnic groups), and a possible association with a strong decrease in smoking (Country overview).
The results of the HBSC 2005 among those aged 12–16 years, indicate a lifetime prevalence of cannabis use of 14.3%, last year prevalence 11.7% and the last month prevalence of 7%. Differences between boys and girls were not significant. The trend for last year prevalence of cannabis has not changed significantly during recent years (Country overview).
Prior to the release of the new household survey for 2006, Germany had reported stable cocaine use levels. The same applied to most neighbouring countries, including Austria, Switzerland, Belgium, the Netherlands, Denmark, Poland, the Czech Republic and other central European countries (Slovakia and Hungary) (UNODC, 2008).
Treatment data suggest that the number of opiate addicts has remained fairly stable for many years. However, new clients are most common within the group of problematic cannabis and amphetamine use (Ouwehand et al., 2007).
Cannabis use stabilised among pupils of secondary schools between 2003 and 2005. There are no new national data on the use of other drugs among school-goers (Van Laar et al., 2008).
2.2.2 Problematic drug users/chronic and frequent drug users
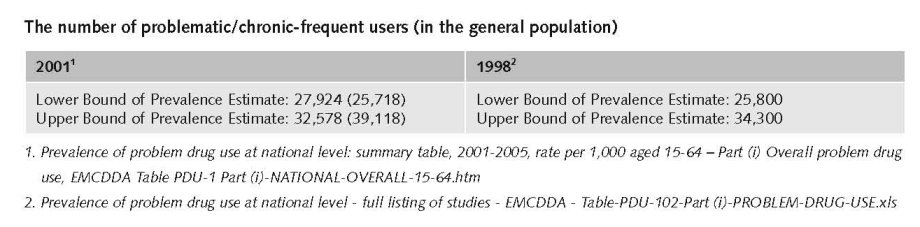
Several national studies have estimated the number of problem opiate users in the Netherlands over the past decade using different methods (treatment multiplier, regression imputation, multiple imputation). For 2001, the number of problem opiate users was estimated at 34,000 problem drug users, or 2.1 users per 1000 inhabitants aged 15–64 using the treatment multiplier method, at 3.1 users per 1000 inhabitants aged 15–64 using regression imputation, and 3.2 users per 1000 inhabitants aged 15–64 using multiple imputation. There is no new estimate available (Country overview; Van Laar et al., 2008).
Most opiate users also use other drugs such as cocaine (including crack cocaine) and other substances. In particular, in recent years the population of crack cocaine users among problem drug users has increased, although the overall estimates of the population of problem drug users remained unchanged. Local and regional studies conducted over the past few years show that the highest concentrations of problem drug users were found in the three largest cities of Amsterdam, Rotterdam, and The Hague (Country overview).
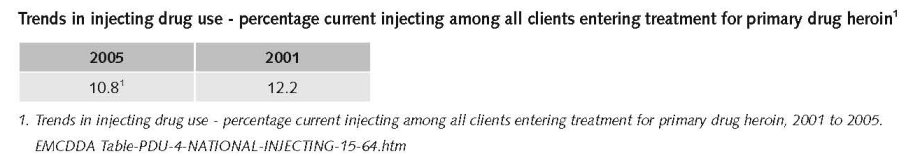
The number of drug users who are currently injecting their drug can be estimated from treatment data given by the National Alcohol and Drugs Information System in combination with the estimated number of problem hard drug users at national level. According to the LADIS, 10% of the opiate clients in 2005 injected their drug. There were 16,199 clients who had a primary or a secondary problem with opiates. This implies that there were about 1,620 currently injecting opiate users in treatment (Van Laar et al., 2008).
All in all, these figures from the opiate and cocaine/crack clients imply that, of the 18,643 problem hard drug clients in treatment, about 1,737 currently inject, which comes down to about 9.3%. Given the estimated number of 33,499 problem hard drug users at national level, it is then assumed that there are about 3,115 currently injecting problem hard drug users in the Netherlands, within a range of 2,211 to 4,321 injectors. Given the total of 11,008,282 inhabitants aged from 15 to 64 years in 2005, it is thus estimated that among the general population, 0.03% are current injectors of hard drugs, within a range of 0.02% to 0.04% (Van Laar et al., 2008).
There is mention of a 2001 estimate of injecting drug users 15-64 in the Netherlands between 0.02% (low) 0.03% (mid) to 0.04% (high). This corresponds with 2,211 (low), 3,115 (mid) to 4,321 (high) people who inject drugs (Mathers et al., 2008).
Data from a cohort study among problem hard drug users as well as national treatment data still show a decreasing prevalence of injection (e.g. 8% in 2006 among opiate clients). This trend is also supported by the continuing decline in the number of exchanged syringes in Rotterdam and Amsterdam (180,100 and 210,000, respectively) (Van Laar et al., 2008).
2.3 Drug related Harm
2.3.1 HIV infections and mortality (drug related deaths)
The number of HIV infected injecting drug users
The Dutch HIV surveillance within the National Institute of Public Health and the Environment uses repeated surveys among drug users in four fixed cities (Amsterdam, Rotterdam, Heerlen-Maastricht, and Arnhem) and two optional cities. Since 2001, one fixed city has been studied per year. In these surveys, hard drug users of heroin, cocaine, methadone and amphetamines are recruited in methadone centres and on the street (Country overview).
In 2006, 833 new HIV diagnoses were reported, which number is likely to increase due to reporting delay. In 94% of cases the most likely route of transmission was known, which in 8 cases was through injecting drug use (1%). By comparison: In 33% of cases heterosexual contact was indicated as the route of transmission, and in 59% homosexual contact. In the total database of the SHM (Stichting HIV Monitoring), the percentage of patients infected through injecting drug use is 5%, indicating that there has been a serious relative reduction of this mode of transmission since the start of the registration (Van Laar et al., 2008).
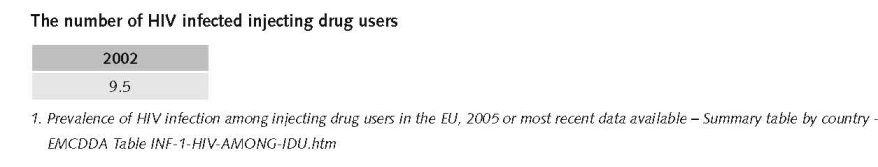
In 2005, 278 new AIDS diagnoses (of which 17 (6%) involved injecting drug use) were made, but this number is subject to change due to reporting delay. In previous years, the number of cases related to injecting drug use peaked in 1995 (74), then dropped to 9, 8, 13 and 6 cases in 2001, 2002, 2003, and 2004 respectively. Until 2005, 659 AIDS patients were registered as being infected through injecting drug use. The annual proportion of injecting drug users varied between 2% and 14% (Van Laar et al., 2008).
The number of drug related deaths by overdose
The main source providing the official Dutch statistics on drug-related deaths is the General Mortality Register or Causes of Deaths Statistics managed by Statistics Netherlands. The register has national coverage and includes only residents of the Netherlands. Cases are classified according to ICD-10 and refer mainly to direct or acute deaths (drug overdoses) (Country overview).
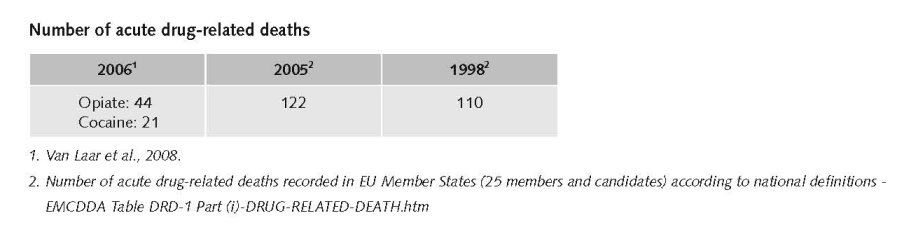
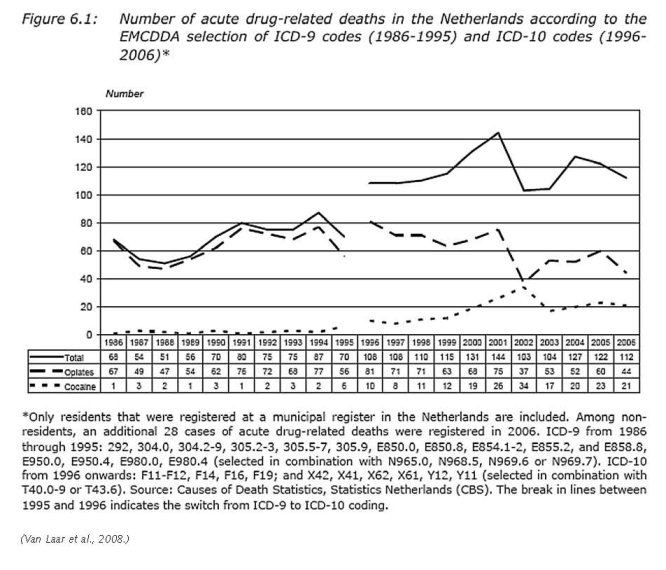
The total number of drug-related deaths increased from 1996 to 2001. This rise may be partly due to the switch from ICD-9 to ICD-10 in 1996, and to the increasing number of cocaine intoxications. Following this increase, DRDs decreased anew to 103–104 cases in 2002–03, followed by a new upward trend observed in 2004 (127 cases), before the consecutive falls in 2005 and 2006 (Country overview).
2.3.2 Drug related crime or (societal) harm
In the Netherlands public nuisance caused by drug dealing and use(rs) on the streets has been a major issue since the eighties of last century. The concept ‘nuisance’ included besides criminal activities (dealing, theft, robbery, etc.), loitering of groups of drug users in the streets, feelings of being threatened by these groups, degradation of neighbourhoods, etc. There are no solid data on the actual extent of these problems (expert’s comments).
3 Drug policy
3.1 General information
3.1.1 Policy expenditures
The total drug policy spending estimate in 2003 was €2,185 million. Allocation to functions amounted to €42 million for prevention, €278 million for treatment, €220 million for harm reduction and €1,646 for enforcement. Drug law enforcement clearly represents the dominant expenditure (Van Laar et al., 2008).
The Netherlands report the highest drug related expenditure in the EU (€139 per capita or 0.66% of GDP) compared to Sweden (€107 per capita or 0.47% of GDP) and to United Kingdom (€68 per capita or 0.35% of GDP). The EU average is 0.15% of GDP (UNODC, 2008).
3.1.2 Other general indicators
The Netherlands’ 1995 white paper ‘Drug policy: continuity and change’ formulated the basic principles of the Dutch drug policy: a distinction between ‘soft’ and ‘hard’ drugs; a balanced and integrated approach; and four major objectives. These are: (i) to prevent drug use and to treat and rehabilitate drug users; (ii) to reduce harm to users; (iii) to diminish public nuisance caused by drug users; and (iii) to combat the production and trafficking of drugs. This white paper, which addresses only illegal drugs, was complemented in subsequent years by several specific strategies in the supply reduction field: dismantling ecstasy production locations (2001); stopping cocaine trafficking by drug couriers using airplanes, especially body-packers (2002); and dismantling large-scale cannabis cultivation (2004) (Country overview).
The ecstasy and cocaine strategies have a strong focus on law enforcement, while the cannabis strategy touches upon all aspects of the issue. In 2006, four developments took place that are relevant with regard to investigation, prosecution and sanctions for offences against the Opium Act. These concern the following three special policy programmes:
• ‘A combined effort to combat ecstasy in and from the Netherlands’ which aims at reducing the production and trafficking of ecstasy (started in 2001);
• The ‘Plan to combat drug trafficking at Schiphol Airport’, which aims to reduce cocaine imports (started in 2002);
• Intensified enforcement of the laws on cannabis cultivation and especially the organised crime behind it (since April 2004). Moreover, in June 2006 the maximum penalty for drug production and dealing and for possession of large quantities of drugs was increased from four to six years of detention or a certain fine (Van Laar et al., 2008).
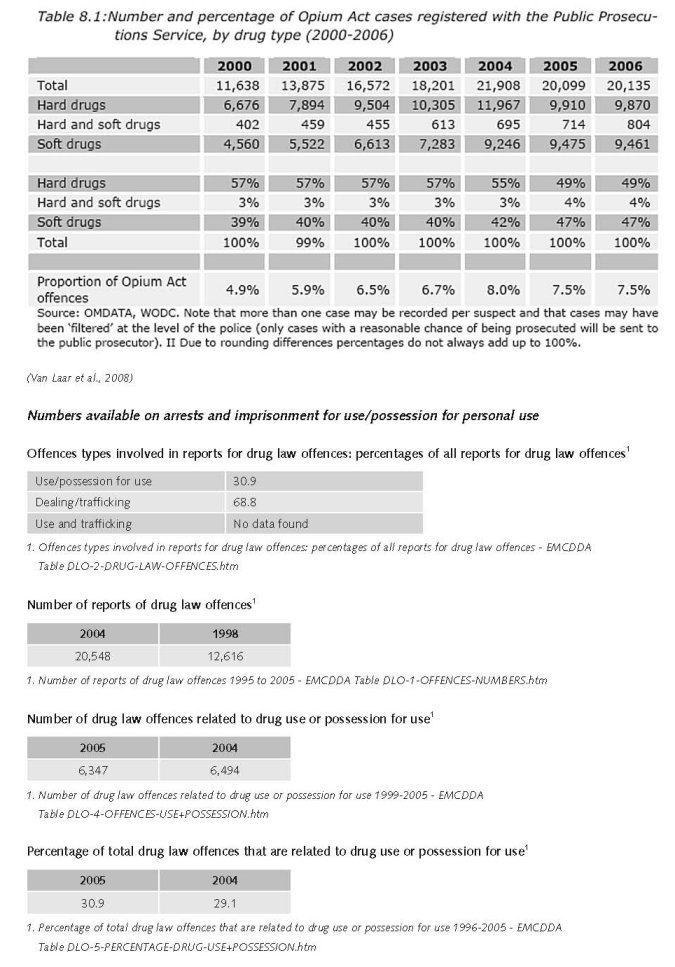
Numbers available on arrests and imprisonment for drug-law related offences
The influx of Opium Act cases in the criminal justice chain did not change significantly in 2005-2006. The police registered 22,000 cases in 2006 (preliminary data) and the Public Prosecutor 20,000. The stabilization in 2006 applies to both hard drug and soft drug cases.
The number of hard and soft drug cases handled by the Court increased (13,000 cases).
The number of community service orders imposed for Opium Act cases decreased in 2006, after a continuous rise in the 2000-2005 period.
Hard drug cases still form the majority of the Opium Act cases, although the difference with the number of soft drug cases is very small in the earlier phases of the criminal justice chain. Hard drug cases account for a clear majority in the later stages, especially in prisons.
The period 2000-2006 shows a rise in the percentage of soft drug cases (of all Opium Act cases) in all parts of the criminal justice chain. This is especially true for 2005-2006. A rise in soft drug cases is also noted in custodial sentences, accompanied by increasing length of these sentences.
75% of the investigations into organised crime involve drug trafficking or production. The majority of these investigations target cases with hard drugs (79%); 60% concern cases with soft drugs; and 39% both hard- and soft drugs (Van Laar et al., 2008).
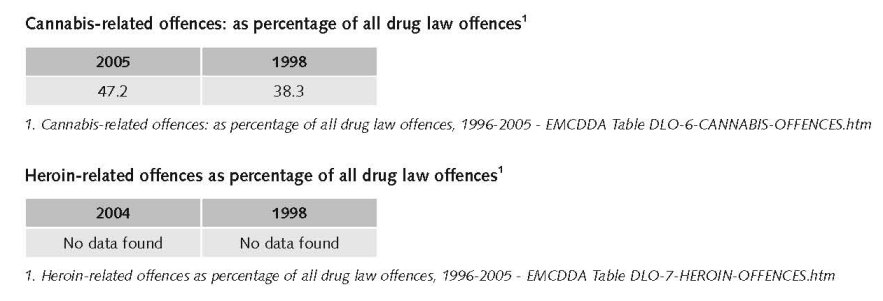
The general term ‘reports for drug law offences’ is used since definitions and study units differ widely between countries. For definitions of the term ‘reports for drug law offences’, refer to Drug law offences – methods and definitions.
3.2 Supply reduction: Production, trafficking and retail
Combating the production and trafficking of drugs are among the major objectives of the Dutch drug policy. There is a trend towards a more punitive approach of production, trafficking and dealing (and keeping at the same time a moderate approach towards use and the possession of small quantities for personal use as already introduced in the seventies. Especially law enforcement efforts aimed at organisational crime involved in heroin, cocaine and synthetic drug offences are priority areas for the justice system. The policy programme of the current Dutch government cabinet aims at intensifying law enforcement efforts on production and trafficking of drugs in the Netherlands (Coalitieakkoord, February 2007) (Van Laar et al., 2008).
Key law is the so-called Opium Act (criminal law,) classifying certain substances as illicit or legally controlled drugs, defining certain acts as criminal offences (like production, trafficking, selling, possession, etc.) and ranking the severity of drug-related crimes, i.e. considering production and trafficking as more serious offences than possession (of small quantities for personal use). Besides this law there are many other laws relevant for supply reduction, e.g. the Temporary Measures for Penitentiary Capacity for Drug Couriers Act, the Closing Drug Premises Act.
Dutch drug legislation is based upon the principle of the separation of the markets for cannabis and other illegal drugs, also known under the non-legal terms of separating the markets for ‘soft’ and ‘hard’ drugs. Thus, illicit substances, according to the Opium Act, are divided into two lists: substances presenting unacceptable risks (list I) and other substances (list II) such as cannabis. This division has a real impact in the prosecution of illegal offences: penalties for offences with regard to list II are lower than those for list I (Country overview).
In the Netherlands, drug use is not a crime. However there are situations where the use of drugs is prohibited (i.e. use in schools). The possession of small quantities of drugs for personal use (less than 0.5 grams of hard drugs (list I) and less than five grams for cannabis (list II) will generally not lead to prosecution. Possession of drugs for commercial purposes will be prosecuted and penalties may range from one month imprisonment and/or a fine to eight years and/or a fine, depending on the quantity and the type of drug. The maximum penalty may be even higher if the crime has been committed more than once (Country overview).
Within the framework of the Opium Act, importing and exporting of any classified drug is considered a serious offence and can be punished by a penalty ranging from four years of imprisonment and/or a fine to up to 16 years of imprisonment depending on whether a ’hard drug’ or a ’soft drug’ was involved. In 2001, a special law was introduced which aims to deliver treatment in prison-like institutions to drug users who are ‘prolific’ offenders. In 2004, a new act for all prolific offenders came into effect (Country overview).
Some recent relevant changes in laws with regards to illicit drugs are:
• Incorporating the European Council Framework Decision of 25 October 2004, laying down minimum provisions on the constituent elements of criminal acts and penalties in the field of illicit drug trafficking into the Dutch Opium Act on 1 July 2006 (Stb 2006/292);
• In June 2006 some changes to the Opium Act were introduced: the maximum penalty for drug production and dealing and for possession of large quantities of drugs was increased from four to six years of detention or a certain fine (Stb 2006/292). This change was made to comply with EU-regulations;
• Law enforcement interventions aimed at the criminal organisations behind the production of Dutch-grown weed will be developed and implemented. Preparations started in 2006 in the south of the country and were under further development in 2007. Police and municipalities are working together already in combating and dismantling cannabis farms, in particular when located at residences, and in preventing criminal activities of grow shops;
• Fresh hallucinogenic mushrooms will be included in the Opium Act, as a soft drug. This was announced by the minister of Health, Welfare and Sport in October 2007, after questions in Parliament and after a report about incidents with these mushrooms in Amsterdam in 2007 (Coördinatiepunt Assessment en Monitoring nieuwe drugs 2007;T.K.30515/12;T.K.30515/15).
(Van Laar et al., 2008)
3.3 Demand reduction: Experimental/recreational drug use + problematic use/chronic-frequent use
Prevention is a priority in current health policy, and one of the five targets is alcohol misuse among young people. In mid-2007 the “Centrum Gezond Leven” (Centre for Healthy Living) started its activities. It informs professionals about available and effective preventive interventions and coordinates the activities of more than ten stake-holding organisations in this field. This centre supports local professionals by presenting the available interventions together with an evaluation of their quality and coherence. The Healthy School and Drugs is still the most widely implemented universal school-based prevention in the Netherlands. Currently pilot studies are running to test electronic strategies. The programme Alcohol and Education targets parents of children at risk of alcohol misuse (Van Laar et al., 2008).
The main feature of the Dutch prevention policy is a strong focus on health promotion in general. Drug prevention focuses on recreational settings, especially regarding party drugs and the implementation of curricular school-based prevention programmes (Country overview).
Universal prevention is mainly carried out within schools, and there are three main school-based drug prevention programmes: ‘Healthy School and Drugs’, ‘Alcohol and Prevention’ and the ‘National Drugs Information Line’. ‘Healthy School and Drugs’ was established more than ten years ago and remains the leading school-based prevention programme in the Netherlands. The programme comprises several lessons in secondary school on alcohol, tobacco and cannabis. ‘Alcohol and Education’ provides advice and supports parents of children under sixteen to prevent alcohol misuse outside school. The ‘National Drugs Information Line’ offers free-of-charge, neutral, objective information, free leaflets and a counselling service (Country overview).
Selective prevention is mostly targeted at youths on the streets and in party settings, and is carried out by NGOs in cooperation with government services. These programmes focus on the implementation of safe clubbing regulations and person-to-person interventions on club premises. Selective prevention is promoted via multi-agency ‘liaisonships’ at a structural level (Country overview).
Risk groups for drug use (e.g. clubbers, children of addicted parents, low SES groups) are targeted in several longer term selective prevention projects, such as the Clubs & Drugs project, Children of Addicted Parents, the Drugs Information and Monitoring System (DIMS) and the family-based programmes Strengthening Families and House Parties (Van Laar et al., 2008).
Special characteristics of the prevention culture in the Netherlands within the European context are: the delivery of universal prevention through one national prevention programme (which is controlled and evaluated); the delivery of selective prevention through several decentralised institutions; a high degree of development and research of prevention in party settings; and, recently, the development of drug prevention via the internet (Country overview).
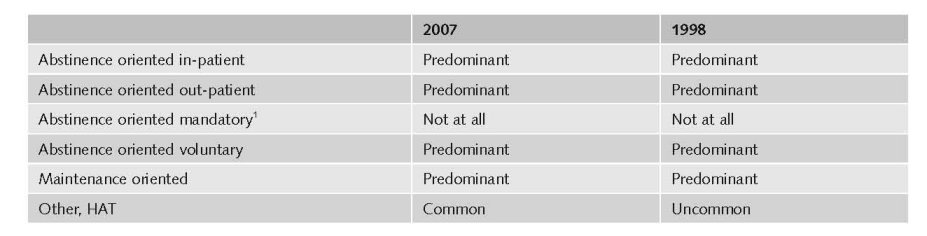
Treatments available
In the Netherlands the responsibility for the organisation, implementation and coordination of addiction care is delegated to regional and local authorities. Drug treatment is mainly delivered by non-governmental organisations on a regional level, followed by private organisations including physicians, hospitals and private clinics. Drug treatment is also provided in regional public hospitals. Funding for drug treatment is mainly provided by the public budget at national and local level. Detoxification and residential treatment is funded by the health insurance (Country overview).
In 2006, several regular addiction care treatment centres decided to found private addiction care facilities and to enter into competition with the, mainly foreign, private clinics. They try to attract the more affluent (and generally socially integrated) patients who want to be treated with discretion in a nice environment (Van Laar et al., 2008).
Drug treatment interventions in the Netherlands are out-patient treatment, in-patient treatment and substitution treatment. Psychosocial interventions are frequently provided to complement substitution treatment in order to attain longer term effectiveness and reduce relapses. Types of frequently-used psychosocial treatments in drug treatment centres are motivational interviewing, relapse prevention techniques, cognitive-behavioural therapies and family therapies (Country overview)
The National Alcohol and Drugs Information System (LADIS) is the most comprehensive information system on treatment demand clients in the Netherlands. LADIS contains data from the regular drug treatment services, including probation services, and provides nationwide coverage (Country overview).
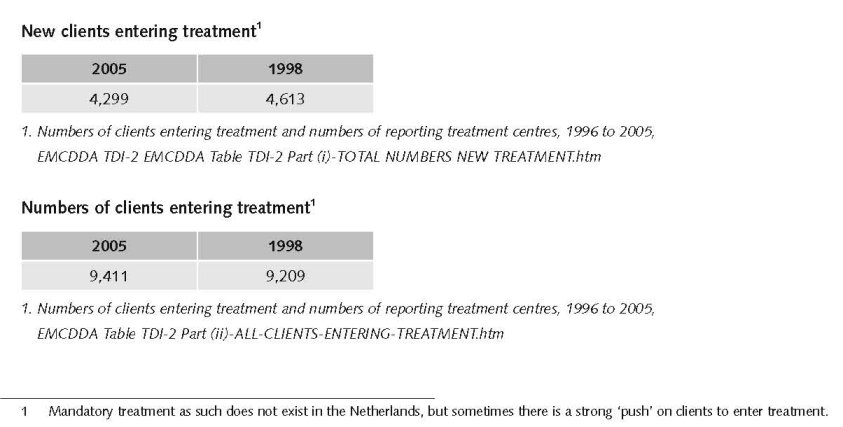
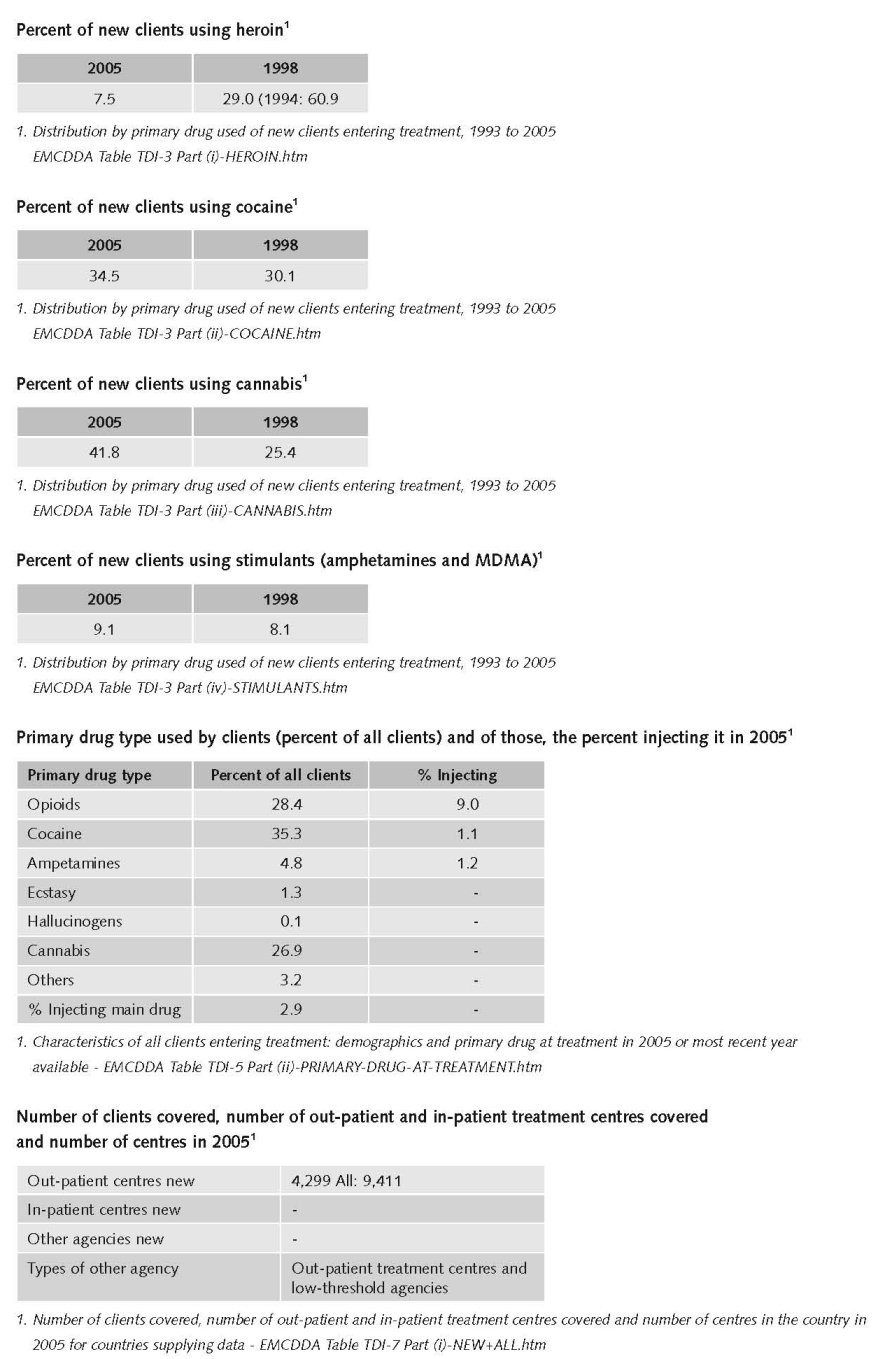
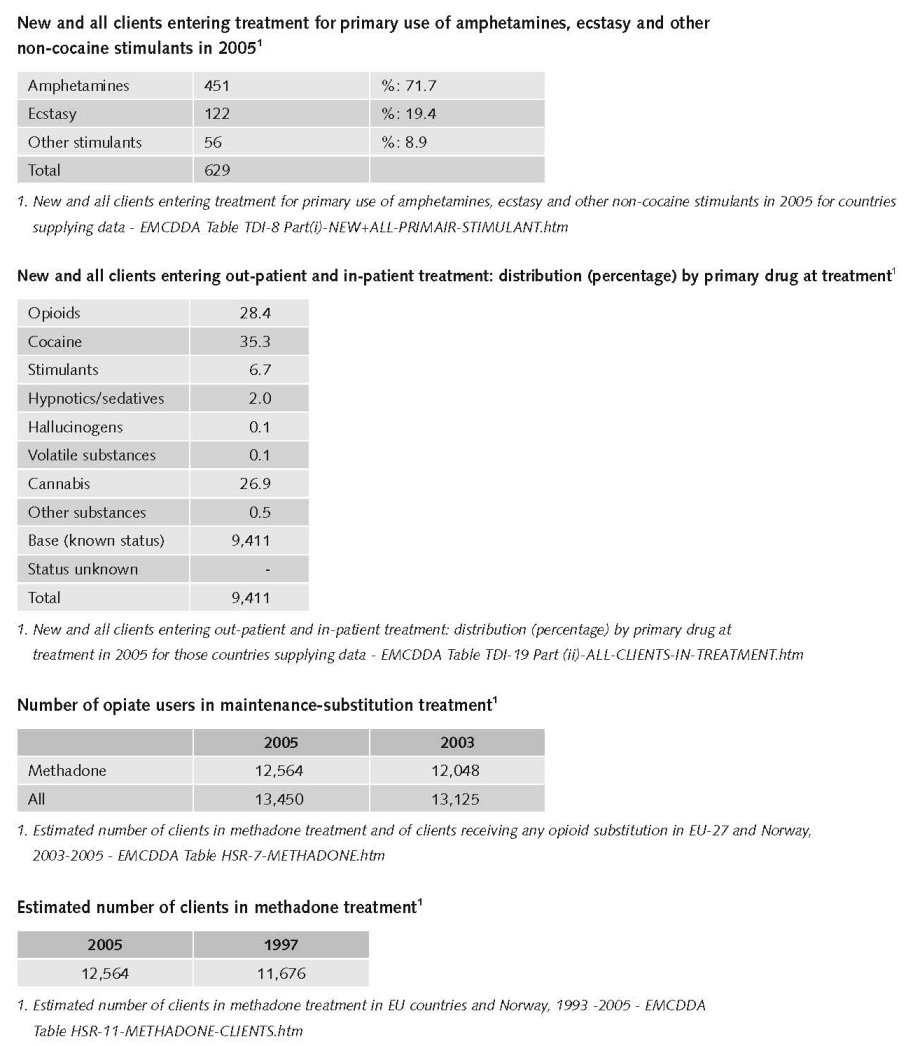
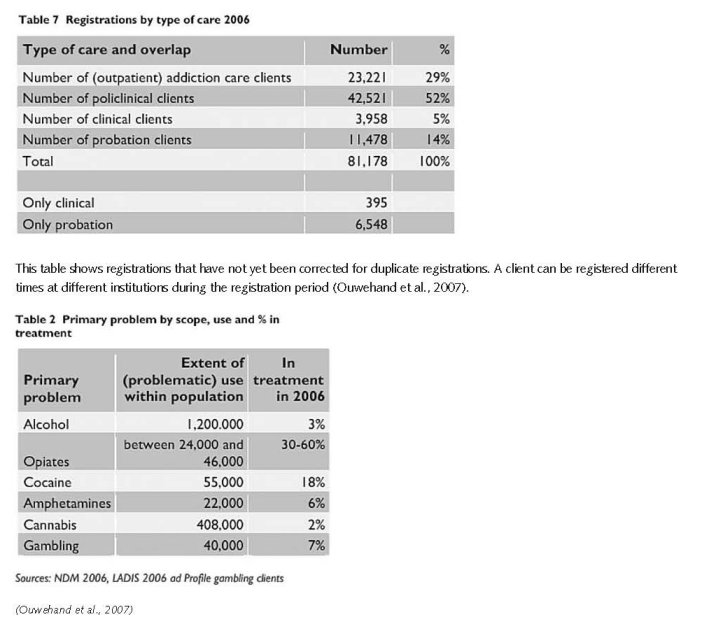
In 2006, a total of 9,623 clients entered treatment, of whom 5,226 clients entered treatment for the first time for a drug problem. Data suggest that 34.7% of all clients entering treatment reported cocaine as their primary drug, followed by 31.8% for cannabis and 22.3% for opioids. Among clients entering treatment for the first time, a slightly different trend was identified with 43.3% requesting treatment for cannabis followed by 31.6% for cocaine and 10.5% for opioids (Country overview).
Recent developments focus on treatment modalities for cocaine and cannabis users, in response to the increased treatment demand of this group of drug users. In the former national report two existing intensive in-patient treatment possibilities for young people with alcohol and drug problems are mentioned. Another example is the experimental treatment for cocaine users, using the Community Reinforcement Approach (CRA) with incentives, i.e. vouchers. The results of this project will be reported in the beginning of 2008 (Van Laar et al., 2008).
With regard to cannabis, the Netherlands is a collaborating partner in the European INCANT study (International Cannabis Need of Treatment), a randomised controlled trial initiated one year ago by five western European countries. The main question is whether Multi Dimensional Family Therapy (MDFT), a treatment developed in the USA, is also effective for Western-European adolescents. INCANT stresses cannabis but does not exclude other issues, e.g. alcohol abuse, psychiatric problems, and psychosocial troubles. Besides the Main Study Protocol and two Newsletters, publications with the first findings are expected within two years (Van Laar et al., 2008).
In recent years coercive approaches have become more popular. Legal options already available are more widely used and improved as e.g. diversion schemes. The ministers promised in a letter to Parliament that by the year 2011 the number of addicts under pressure to have treatment would be doubled (T.K.31110/1). The Judicial Placement of Addicts (Strafrechtelijke Opvang Verslaafden - SOV) – introduced in 2001 – has been adapted. This option allows the courts to place prolific offenders, who are addicted to drugs, commit repeated petty crimes and who were expected not to benefit from other interventions, in a special institution. The aim of this initiative was to reduce public nuisance and to promote behavioural change among offenders. The maximum duration of this measure is two years. New options are implemented as e.g. conditional release at the end of the detention period (Van Laar et al., 2008).
Since 1968, methadone is the most commonly prescribed substitution substance. Heroin-assisted treatment (introduced in 1997) and high dosage buprenorphine treatment (introduced in 1999) are also available. High-dosage buprenorphine treatment is only provided in specialised treatment centres. Methadone on the other hand, is available via various treatment providers, including office-based practitioners and mobile units. In 2006, the number of clients on methadone maintenance treatment was around 12 500 (Country overview). In the autumn of 2006, a total of 815 treatment places for medical prescription of heroin (in 18 municipalities) were approved by the Minister. This policy is continued by the new government (Van Laar et al., 2008).
Priorities of demand reduction covered by policy papers and/or law
The policy programme Scoring Results that was started in 1999 to improve quality in drug prevention and addiction care is in its last phase. Many research publications and protocols have been published to support this target. Its current focus is on developing protocols, implementation of guidelines and professional training and education in addiction. Benchmarking of addiction care is examined, and a new instrument for treatment allocation and evaluation (Measurement of Addiction for Triage and Evaluation (MATE) has been introduced, which may replace the Addiction Severity Index during the coming years. Two addiction care organisations are now certified by the National Expertise Centre on Quality Review in Health Care (Van Laar et al., 2008).
The programme Scoring Results has been prolonged until 2008 with a focus on further developing protocols, on the implementation of guidelines and on starting specialised courses in professional training and education in order to improve the expertise of future professionals. Between 1999 and 2007, this programme received funding of € 2,450,000.
Monitoring the performance of addiction care will be facilitated by a set of outcome indicators (prestatie-indicatoren) for the broad domain of mental health and addiction care. The indicator set encompasses data on several aspects of effectiveness of care, safety, and client-centred data (Van Laar et al., 2008).
3.4 Harm reduction
3.4.1 HIV and mortality
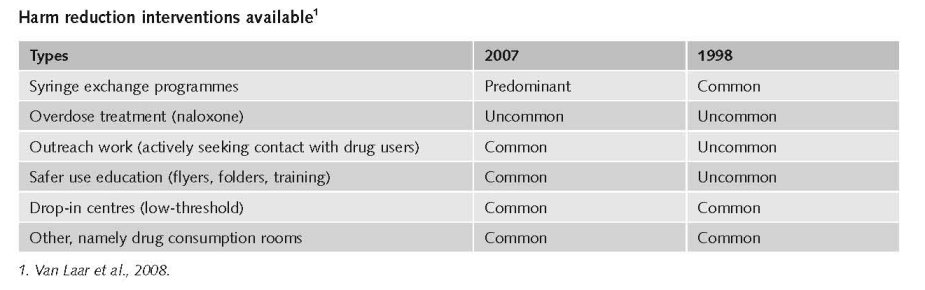
Harm reduction is an important feature of the Dutch drug policy and as a result there are many harm reduction interventions in the country. In the Netherlands there is an explicit supportive reference to harm reduction in national policy documents.2
In practically all cities and towns there are facilities for needle and syringe exchange. This may take place at (low-threshold) drug services and some pharmacies. Health care centres and some places also police stations may have boxes for disposing dirty needles (no exchange). Finally there are also a number of vending machines for clean needles, but their number is limited and restricted to the bigger cities (Van Laar et al., 2008).
2 Global State of Harm Reduction, IHRA, 2008.
In the Netherlands, the difference between outreach work, low-threshold services, harm reduction activities and the term ‘social addiction care’ is hard to define. All four deal with motivating difficult-to-reach drug users (hidden populations) to participate in some kind of treatment to prevent a worsening of their life situation (individual and/or social) (Country overview).
Most outreach work is carried out by low-threshold services in out-patient care facilities. These services are active in ‘street corner work’ offering daytime shelter in drop-in centres for street problem drug users, ‘living room’ projects for drug-using prostitutes and user rooms for chronic hard drug users. Other target groups of these services are injecting drug users, extremely problematic drug users, and drug users from foreign countries. Outreach activities also feature in programmes for reducing drug-related public nuisance, which are often a joint venture between treatment and care facilities, police and civic groups. Outreach work today is often education ‘on the spot’ (i.e. where young people meet) applying peer-support techniques. Another one is targeting at drug users who have been sentenced to prison (Country overview).
Some drop-in centres are combined with drug consumption rooms. Presently there are about 40 drug consumption rooms in the Netherlands (Van der Gouwe et al., 2006).
Facilities for needle exchange or syringe exchange have existed for more than twenty years in the Netherlands and are available in all major Dutch cities. Needle exchange programmes are mainly implemented by street workers, workers of institutes for addiction care, and to a much lesser extent by pharmacists. The total number of needle exchange programmes in the Netherlands is not known, nor are there national registration data on the number of exchanged syringes or needles. However, data from Amsterdam show that from 1990 to 1993, around one million needles were exchanged. Since 1993 there has been a sharp decline to 38,000 syringes in 2006 (Country overview).
Overdose treatment is not a standard procedure in drug services in the Netherlands, but it is the responsibility of the medical staff. Naloxone is in general not available at drug services (Van Laar et al., 2008).
3.4.2 Crime, societal harm, environmental damage
One of the key targets of drug policy in the Netherlands is to reduce drug-related public nuisance in neighbourhoods, i.e. drug users hanging around and using drugs on the streets, dealing on the streets and drug-use related crimes like street robbery, shop-lifting and burglary. Intensive policing, special measures like banning individuals who cause nuisance from certain areas (‘straatverbod’), but also drop-in centres and drug consumption facilities are examples of measures taken.
A specific Dutch problem is public nuisance caused by so-called drug tourism. The larger cities and the cities in the border region attract considerable numbers of young people from neighbouring countries (Belgium, Germany and France) who cross the border to buy cannabis in Dutch coffee shops. People living in the neighbourhood of coffee shops complain about crowds hanging around on the streets till late in the evening, heavy car traffic and parking problems, etc. Consequently, at certain times initiatives have been taken at the local level to address this. There are several laws and policies aimed at reducing drug related nuisance.
References
Consulted experts
G. Cruts, Research fellow, Unit Drugs Monitor, Trimbos Institute, Utrecht.
T. Ketelaars, Research fellow, Unit Drugs Monitor, Trimbos Institute, Utrecht.
M. van Laar, Head Unit Drugs Monitor, Trimbos Institute, Utrecht.
Documents
CIA. The World Factbook: The Netherlands. Available: www.cia.gov/library/publications/the-world-factbook/geos/nl.html, last accessed 10 December 2008.
Cook C, Kanaef N. Global state of harm reduction 2008. Mapping the response to drug-related HIV and hepatitis C epidemics. London, International Harm Reduction Association (IHRA), 2008.
Country overview: The Netherlands. Available: www.emcdda.europa.eu/publications/country-overviews/nl, last accessed
10 December 2008.
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction). A cannabis reader: global issues and local experiences, Monograph series 8, Volume 1. Lisbon, EMCDDA, 2008.
Fijnaut C, de Ruyver B. Voor een gezamenlijke beheersing van de drugsgerelateerde criminaliteit in de Euregio Maas-Rijn. Tilburg – Gent, 2008.
KLPD-IPOL. Het groene goud. Verslag van een onderzoek naar de cannabissector voor het Nationaal dreigingsbeleid criminaliteit met een georganiseerd karakter. Zoetermeer, KLPD, 2008.
Legget T, Pietschmann T, ‘Global cannabis cultivation and trafficking, in: A cannabis reader: global issues and local experiences, Monograph series 8, Volume 1. Lisbon, EMCDDA, 2008.
Mathers B, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee S, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP. (2007 Reference Group to the UN on HIV and Injecting Drug Use). Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Vienna, UNAIDS, 2008.
Monshouwer K, Verdurmen J, van Dorsselaer S, Smit E, Gorter A, Vollebergh W. Jeugd en Riskant gedrag 2007. Kerngegevens uit het Peilstationsonderzoek Scholieren. Utrecht, Trimbos Instituut, 2008.
Ouwehand AW, Kuijpers WGT, Wisselink DJ, van Delden EB. Key figures National Addiction Care 2006; National Alcohol and Drugs Information System. Stichting Informatie Voorziening Zorg. Houten, 2007.
UNDCP (United Nations International Drug Control Programme). Global Illicit Drug Trends 2000. Statistics. Vienna, UNDCP, 2001.
UNODC (United Nations Office on Drugs and Crime). World Drug Report 2007. Vienna, UNODC, 2007.
UNODC. World Drug Report 2008. Vienna, UNODC, 2008.
Van der Gouwe D, Gallà M, Van Gageldonk A, Croes E, Engelhardt J, Van Laar M, Buster M. Prevention and reduction of health-related harm associated with drug dependence: an inventory of policies, evidence and practices in the EU relevant to the implementation of the Council Recommendation of 18 June 2003. Utrecht, Trimbos Institute, 2006.
Van Dijk P. DIMS Jaarbericht 2005. Utrecht, Trimbos Instituut, 2006.
Van Dijk P. DIMS Jaarbericht 2007. Utrecht, Trimbos Instituut, 2008.
Van Laar M, Cruts G, van Gageldonk A, Croes E, van Ooyen-Houben M, Meijer R, Ketelaars T. The Netherlands Drug Situation 2007. Report to the EMDCCA. Utrecht, Trimbos Instituut, 2008.
| < Prev | Next > |
|---|