5 European and non-European evidence of effectiveness of drug treatment
| Reports - Models of Good Practice in Drug Treatment |
Drug Abuse
5 European and non-European evidence of effectiveness of drug treatment
Results related to the effectiveness of drug treatment are based on research from all
available countries (inside and outside of Europe). In order to separate the studies
conducted in European States from those conducted outside of Europe, the country of
origin of all included references was identified. The number of included references was
counted for each chapter and allocated as evidence from a European State or from a
State outside of Europe. Usually it is indicated if the research was conducted in
European State, although the evidence of effectiveness is not influenced by the location
of the study concerned. Generally there are some reviews and systematic reviews on the
effectiveness of drug treatment conducted by researchers in European countries (e.g.
Berglund et al 2003; Rigter et al. 2004; Amato et al. 2007), but these reviews cover
research from all over the world as well. The methodology for the identification of
relevant literature is described in chapter 4.
5.1 Evidence from outside of Europe
Pharmacological treatment agents for opioid-related disorders
Crisis Intervention
Use of naloxone and naltrexone for crisis intervention
Heroin overdose is one of the leading causes of death among heroin addicts (Sporer
2003) and non-fatal overdoses are highly prevalent among opioid addicts (Warner-
Smith et al. 2001). One study showed that 23-33% of injecting heroin users have taken a
non-fatal overdose in the last year, and 43% have witnessed a heroin overdose in
another user within the last year (Sporer 1999).
The short-acting opioid-antagonist naloxone is considered to be an effective substance
in treating respiratory depression and coma in patients with an overdose (Kaplan et al.
1999), This has prompted a discussion on a new strategy to reduce the risks of overdose,
by making naloxone available in addicts´ homes for peer administration in order to
prevent fatal overdose (Baca & Grant 2005; Lagu et al. 2006; Sporer 2003). A recent
study supports this recommendation by showing, that especially drug users with an
overdose history have a great willingness to administer naloxone in the case of a friend's
overdose (Lagu et al. 2006).
There is no evidence to suggest that subcutaneous or intramuscular routes of
administration are inferior to intravenous administration of naloxone (Clarke 2001),
where as another route, the nasal application of naloxone, seems to be comparably
effective to the intravenous application (Barton et al. 2005). Others studies investigated
the preventive effect of sustained release naltrexone implants, where initial findings
support the clinical efficacy in preventing opioid overdose (Hulse et al. 2005).
As a recent period of abstinence may lead to a reduction in tolerance and has been
shown to be a time of particular risk, the best prevention of heroin overdoses is
participation in opioid-assisted maintenance treatment. All opioid dependent persons
who opt for abstinence based treatment need to be made aware of the particular risk of
overdose after a period of abstinence. This is especially true when abstinence was
temporarily obtained through maintenance treatment with the long-acting opioid
antagonist naltrexone. Extended use of naltrexone can result in supersensitivity of the μ-
opioid receptors and an increased risk of overdose (Lesscher et al. 2003). Digiusto et al.
showed eight times higher rates of experienced overdoses in naltrexone treated
participants after leaving treatment, compared to participants who left agonist treatment
(Digiusto et al. 2004). Recently, Gibson et al. found the overdose-related risk of death
related to oral naltrexone appears to be higher than that related to methadone treatment
(Gibson et al. 2007). This results lead to an open discussion about the overdose-related
death risk of oral naltrexone.
In summary, the short-acting opioid-antagonist naloxone is effective in treating in
patients with an overdose. However, an extended use of opiate antagonists can lead to a
reduction of tolerance and therefore to an increased risk of overdose.
Pharmacotherapy of opioid withdrawal/detoxification
Withdrawal or detoxification treatment is a necessary step to enter a following drug-free
treatment and during detoxification various pharmacological substances can be used to
manage withdrawal symptoms, including (partial/full) opioid agonists (e.g. methadone,
buprenorphine), opioid antagonists (e.g. naltrexone) and α2-adrenergic agonists (e.g.
clonidine). The major goal of pharmacotherapy during detoxification is to relieve the
severity of opiate withdrawal symptoms in order to avoid unnecessary human suffering
and medical complications (e.g. epileptic seizures) as well as to enhance motivation to
continue treatment (Gonzalez et al. 2004).
Methadone as a detoxification agent (including methadone reduction treatment)
Detoxification treatment with tapered doses of methadone showed fewer severe
withdrawal symptoms and fewer drop out rates compared to placebo (Kleber et al.,
2007). Nevertheless, various patients relapse to heroin use and in comparison to
methadone maintenance treatment, methadone withdrawal treatment leads to high dropout
rates, even though the effect on the proportion of positive urine samples in both
treatment modalities remains high (Kleber et al. 2006). Because of the poor treatment
outcomes especially in rapid detoxification approaches (e.g. 10% dose reduction per
week) like taper interruptions, illicit drug use and withdrawal symptoms, a gradual
methadone taper (like 3% per week) is recommended (Kleber et al. 2006).
Higher doses of methadone for non-rapid detoxification were found to be more effective
than lower doses with regard to treatment retention and fixed methadone detoxification
programmes may lead to higher retention rates than flexible methadone detoxification
schedules (Kleber et al. 2006). Patients who are informed about the methadone
withdrawal schedule have better outcomes than uninformed patients, although patients
do not have better outcomes, when they control their methadone schedule on their own
(Gowing et al. 2001; Kleber et al. 2006). One Australian effectiveness report found that
detoxification with tapered doses of methadone is more likely to be completed if
withdrawal is scheduled to occur over a short period of time (21 days or less) (Gowing
et al. 2001).
Low doses of methadone were found to be equal to clonidine in the effectiveness to
suppress withdrawal symptoms (Gowing et al. 2001; Kleber et al. 2006). However, in
comparison to methadone treated patients, patients treated with clonidine were more
likely to leave the treatment early, possibly because opioid agonists suppress
withdrawal symptoms early in treatment (Kleber et al. 2006). No differences were
found between clonidine and low doses of methadone with respect to withdrawal
symptoms, but patients treated with clonidine tend to dropout earlier compared to
patients treated with methadone (Gowing et al. 2001; Kleber et al. 2006). Buspirone, an
azipirone used primarily as an anxiolytic agent, administered in addition to methadone,
could lead to a more rapid methadone taper with larger and more frequent methadone
decrements, but more trials will be needed to confirm this hypothesis (Buydens-
Branchey et al. 2005).
There is evidence to show that severity of withdrawal under methadone tapering can be
reduced by different psychosocial measures, such as having patients well-informed
(Green & Gossop 1988), contingency management (Hall et al. 1979) or counselling
(Rawson et al. 1983). Kleber et al. (2006) suggests combining pharmacological
treatment with behavioural and psychosocial approaches to increase efficacy (Kleber
2003). The recent Cochrane review found only one randomised controlled clinical trial
comparing inpatient and outpatient settings for opioid detoxification, suggesting that
opioid detoxification in inpatient settings is slightly more effective, but the underlying
available research remains limited (Day et al. 2007).
In summary, there is evidence that detoxification treatment using tapered doses1 of
methadone is associated with adequate rates of completion of withdrawal, reduction of
withdrawal symptoms to tolerable levels, and minimal adverse effects. Control by the
clinician rather than the patient of the rate of reduction of the methadone dose is
associated with greater reductions in methadone doses. Compared to the effects of
methadone in maintenance treatment, the efficacy of methadone for detoxification
treatment is limited. The attrition rate of methadone detoxification treatment remains
high, particularly in an outpatient setting compared to an inpatient setting. Despite the
findings related to methadone and α2-adrenergic agonists of one recent RCT, the current
systematic Cochrane review shows that methadone had better outcomes than other
opioid agonists in terms of completion rate, and patients have shown less severe
withdrawal symptoms.
Buprenorphine as a detoxification agent
The partial μ-agonist and κ-antagonist buprenorphine is a commonly used agent for the
detoxification treatment of opiate dependents, mainly in Europe and Australia. In the
USA, buprenorphine is commonly combined with the short-acting opioid-antagonist
naloxone. Like methadone, the detoxification treatment with buprenorphine is carried
out in a linear reduction schedule with equal dose decreases.
The efficacy of buprenorphine in the detoxification of opioid dependents is comparable
to methadone with regard to treatment retention, illicit drug use, and suppression of
withdrawal symptoms, though detoxification with buprenorphine can be completed
more quickly, within 3 to 8 days (compared to a normally duration of 14 days in
methadone detoxification (Gowing et al. 2007; Kleber et al. 2006). Also, no significant
differences were found between buprenorphine and methadone in terms of completion
of withdrawal, despite quicker resolution of withdrawal symptoms with buprenorphine
(Gowing et al. 2007). Furthermore, the current Cochrane review found that neither
buprenorphine nor methadone is associated with significant adverse effects when used
to manage opioid withdrawal (Gowing et al. 2007). The recent Cochrane review
suggested that gradual tapering of buprenorphine after buprenorphine maintenance
appears to be more effective than rapid tapering, but further research is needed to
confirm this assumption (Gowing et al. 2007).
Kosten and O’Connor (Kosten & O'Connor 2003) prefer buprenorphine over methadone
as their first choice opioid tapering and detoxification strategy, because withdrawal
symptoms of methadone last longer than those of buprenorphine. Conventional inpatient
detoxification (clonidine and other medications for a mean of 3.5 days) was found to be
more effective in achieving initial abstinence than outpatient detoxification using
buprenorphine (Digiusto et al. 2005). Only 12% of patients treated with buprenorphine
in an outpatient setting achieved initial abstinence compared to 24% of patients in
conventional inpatient treatment (Digiusto et al. 2005), although outpatient
detoxification was found to be more effective with buprenorphine than when
conventional symptomatic medications (e.g. clonidine) were used in an outpatient
setting (4%) (Digiusto et al. 2005).
Assadi et al. (2004) suggest that opioid detoxification using high doses of
buprenorphine (12 mg) in 24 hours is a reasonable approach to reduce the time required
for opioid detoxification (Assadi et al. 2004). One group of twenty patients were treated
with 12 mg buprenorphine in 24 h, the other patients received conventional doses of
buprenorphine tapered down over 5 days. No significant group differences were found
regarding treatment retention, severity of subject-rated opioid withdrawal, and side
effects profile. Patients treated with a high dose of buprenorphine in 24 hours,
developed early the maximal withdrawal symptoms, and patients in the conventional
protocol group were more likely to use more adjuvant medications for symptom
palliation. However, larger studies are needed to confirm these results.
Buprenorphine tapering was found to be more effective than clonidine or clonidine
combined with naltrexone for the management of opioid withdrawal, especially in the
suppression of withdrawal symptoms (Gowing et al. 2007; Kleber et al. 2006).
Buprenorphine probably improves withdrawal symptoms better than clonidine (Gowing
et al. 2001). Furthermore, buprenorphine has fewer cardiac side effects than clonidine
and methadone (Gowing et al. 2001). Compared to clonidine, buprenorphine has also
more positive effects on well-being and psychosocial variables (Ponizovsky et al. 2006).
Collins et al. (2005) found no significant differences, but greater rates of treatment
retention and naltrexone induction in patients detoxified with buprenorphine than in
anesthesia-assisted or clonidine-assisted heroin detoxification, but no differences in
completion rates of inpatient detoxification and opioid free urine samples (Collins et al.
2005).
A recent proposal is to detoxify heroin addicts with a single high dose of buprenorphine
(32 mg), because the combination of a high dose, the relative long plasma half-life and
the slow dissociation kinetics of the drug from the opioid receptors seems to create a
slow and effective tapering process (Kutz & Reznik 2002). Future research should focus
on determinants of withdrawal following cessation of buprenorphine in tapered doses
and the optimum approach to withdrawal following long-term buprenorphine
substitution treatment. Also the effectiveness of buprenorphine for managing
withdrawal from methadone as compared to withdrawal from heroin still remains
unclear, even though some studies indicated that the use of buprenorphine for the
management of withdrawal from methadone is feasible (Gowing et al. 2007). Also more
information is needed about the transition from methadone to buprenorphine, which can
lead to precipitated withdrawal (Johnson et al. 2003).
In summary, buprenorphine seems to have similar efficacy as tapering doses of
methadone for the treatment of opioid detoxification with comparable effectiveness in
improving withdrawal symptoms and in completing detoxification treatment. Compared
to clonidine, buprenorphine provides at least more effectiveness in withdrawal
management and has fewer adverse effects. Therefore, a replacement of heroin by
buprenorphine in tapered doses followed by the prescription of α2-adrenergic agonist
(e.g. clonidine or lofexidine) to reduce withdrawal symptoms proved to be an effective
strategy for detoxification of opioid addicts (Gowing et al. 2004; Gowing et al. 2004a).
However, it should be noted that patients on high doses of heroin are sometimes
difficult to stabilise with the partial agonist buprenorphine, resulting in precipitated
withdrawal symptoms and early drop out.
α2-adrenergic agonists as detoxification agents
The use of α2 adrenergic agonists (clonidine, lofexidine) to manage the acute phase of
opioid withdrawal is common worldwide.
The α2-adrenergic agonists clonidine and lofexidine have been approved for
detoxification treatment. Clonidine reduces opioid related withdrawal symptoms,
although does not completely relieve symptoms like anxiety, restlessness and insomnia
(Kleber et al. 2006). In comparison to morphine, clonidine is more effective in
suppressing objective withdrawal symptoms, but less effective than morphine in
attenuating subjective withdrawal symptoms (Kleber et al. 2006). Low doses of
methadone were found to be equally effective in suppressing withdrawal symptoms as
clonidine, but patients treated with clonidine were more likely to drop out early
(Gowing et al. 2001; Kleber et al. 2006). No differences were found between clonidine
and low doses of methadone in resolving withdrawal symptoms, but patients treated
with clonidine tend to drop out earlier compared to patients treated with methadone
(Gowing et al. 2001; Kleber et al. 2006). Maybe one reason for the high attrition rate in
the early stage of treatment with clonidine is that patients treated with clonidine develop
withdrawal symptoms early in treatment compared to methadone tapering (Gowing et
al. 2001). Another reason for lower retention rates of withdrawal with clonidine could
be higher rates of adverse effects. Despite more evidence supporting the efficacy of
clonidine, it has now been shown that lofexidine is to be preferred over clonidine,
because hypotension is less likely to occur with lofexidine (Gowing et al. 2004).
The comparison of α2-adrenergic agonists with methadone tapering shows some
differences - the longer duration of methadone tapering, no difference in completion
rates, similar or marginally greater withdrawal severity with α2-adrenergic agonists,
earlier resolution of withdrawal under α2-adrenergic agonists, more adverse events for
clonidine - but no overall difference in clinical efficacy (Gowing et al. 2004).
A systematic review, including ten clinical trials, indicates that the clinical effectiveness
of buprenorphine is superior to clonidine regarding suppression of opioid withdrawal
symptoms, treatment retention, side effects and completion of treatment (Gowing et al.
2004). Recent randomised trials confirmed these findings. Oreskovich et al. (2005)
demonstrated in their randomised, prospective pilot study the superiority of high doses
of buprenorphine to clonidine for acute detoxification from heroin in different
measures, like suppression of withdrawal symptoms (Oreskovich et al., 2005).
Ponizovsky et al. (2006) compared detoxification programs using buprenorphine and
clonidine with regard to side effects and effects on well-being and psychosocial
variables in a randomised controlled trial design (Ponizovsky et al. 2006). Patients, who
received clonidine, developed significantly more side-effects. The authors suggested
that buprenorphine is preferable for inpatient detoxification due to these findings. The
application of buprenorphine in combination with behavioural interventions proved to
be more effective than the combination of clonidine and behavioural interventions with
regard to treatment retention in the detoxification of opioid-dependent adolescents
(Marsch et al. 2005). Patients treated with buprenorphine were also more likely to
provide negative urine samples. On the other hand, Digiusto et al. (2005) found higher
retention rates in patients treated in an inpatient detoxification setting with clonidine
plus other symptomatic medications than in patients in outpatient detoxification using
buprenorphine or clonidine plus other symptomatic medications (Digiusto et al. 2005).
Higher completion rates were found for patients in clonidine-naloxone precipitated
withdrawal treatment under sedation (rapid opioid detoxification), than in clonidineassisted
detoxification (Arnold-Reed & Hulse 2005). However, the reasons for these
findings remain unclear: No differences were found in secondary outcomes, like
severity of withdrawal or craving, and also oral naltrexone compliance levels and
abstinence from heroin four weeks following detoxification were similar (Arnold-Reed
& Hulse 2005).
Sinha et al. (2007) found higher opioid abstinence rates and better relapse outcomes in
patients treated with lofexidine-naltrexone compared to those treated with placebonaltrexone
(Sinha et al. 2007). Furthermore, patients treated with the combination of
lofexidine and naltrexone showed lower opioid craving symptoms in laboratory as
patients in the placebo-naltrexone group. The authors concluded that lofexidine has the
potential to decrease stress-induced and cue-induced opioid craving and improves
opioid abstinence in naltrexone-treated opioid-dependent individuals (Sinha et al. 2007).
The combination of opioid antagonists like naltrexone and α2-adrenergic leads to a
more intense (higher peak) but less overall withdrawal severity than withdrawal
managed with clonidine or lofexidine alone (Gowing et al. 2006). The additional
provision of symptomatic medications enhanced the effectiveness of adrenergic
agonists, and especially the combination with opioid antagonists such as naltrexone and
naloxone leads to less severe withdrawal symptoms in detoxification compared to the
treatment with lofexidine alone (Gowing et al. 2006).
In summary, adrenergic agonists (clonidine and lofexidine) could be considered as an
effective detoxification option especially for patients, who prefer non-opioid treatment
for detoxification. Compared to tapering doses of methadone, opioid withdrawal
management with α2-adrenergic agonists like clonidine and lofexidine leads to equal
rates of completion of withdrawal and overall severity of withdrawal, but to more side
effects and therefore to higher drop-out rates especially at an earlier stage of treatment.
Buprenorphine seems to be superior to clonidine, with regard to the better safety profile,
well-being and self-efficacy. Lofexidine showed fewer side effects with similar clinical
effectiveness in comparison to clonidine. The most described adverse effect of the
opioid withdrawal treatment with clonidine is hypotension, which leads to the
recommendation to check patients` blood pressure regularly. Due to the hypotensive
side effects of clonidine, lofexidine should be preferred in outpatient settings.
Buprenorphine-naloxone combination as a detoxification agent
The combination of buprenorphine and naloxone is available for the maintenance and
detoxification treatment of opioid dependence is available several countries worldwide.
The intention of adding naloxone to buprenorphine is to deter intravenous misuse and
reduce the symptoms of opiate dependence.
Recent RCTs show that a direct and rapid detoxification with buprenorphine-naloxone
is safe and well tolerated by patients with good results in terms of treatment retention,
detoxification completion and abstinence rates in treatment (Amass et al. 2004; Ling et
al. 2005). Amass et al. (2004) treated 234 mostly intravenous heroin-dependent
participants in a thirteen-day buprenorphine-naloxone taper regimen for short-term
opioid detoxification. Most patients received an initial dose of 8 mg buprenorphine-2
mg naloxone and reached a target dose of 16 mg buprenorphine-4 mg naloxone in three
days. Treatment compliance and treatment retention were high: Four of five patients
showed compliance with regard to the medication and two of three patients completed
the detoxification treatment. Only one serious adverse event2 was possibly related to
buprenorphine-naloxone (Amass et al., 2004). Ling et al. (2005) used a multi-centre
randomised trial design to investigate the clinical effectiveness of buprenorphinenaloxone
and clonidine for opioid detoxification in inpatient and outpatient settings. 113
inpatients and 231 outpatients were recruited, and short-term treatment seeking opioiddependent
individuals were randomly allocated in a 2:1 ratio to buprenorphine-naloxone
or clonidine detoxification treatment over a period of 13 days. Appreciably more
participants treated with buprenorphine-naloxone completed the detoxification
treatment and provided also opioid-free urine samples on the last day of clinic
attendance (Ling et al. 2005). With respect to dose related effects of
buprenorphine/naloxone, a recent double-blind randomised controlled trial found that
patients did not additionally benefit from buprenorphine/naloxone doses higher than 8
mg/2 mg with regard to opioid blockade and withdrawal symptom suppression (Correia
et al. 2006). However, Hopper et al. (2005) showed that a single high dose of a 32 mg
buprenorphine/naloxone combination tablet is a feasible method for rapid
detoxification. In this pilot study, twenty patients were randomly allocated to one-day
vs. three-day buprenorphine inpatient detoxification protocols for heroin dependence.
No group differences were found with regard to completion rates, retention in treatment,
intensity of withdrawal symptoms, and provision of opiate-free urine samples (Hopper
et al. 2005). In summary, the combination of buprenorphine and naloxone is effective
and safe for the detoxification of opioid dependents and well tolerated by patients.
Pharmacotherapy for opioid maintenance
Given the chronic, relapsing nature of the disease and the generally disappointing longterm
results of detoxification in combination with relapse prevention, stabilisation of
illicit drug use, improvement of well-being and reduction of drug related harm have
become the most important treatment modality in many countries. Opioid-assisted
maintenance programmes are among the most important strategies in this respect, as
they are associated with reductions of heroin use and HIV risk behaviour (Kerr et al.
2005). Considering the high rate of relapse after detoxification of opioid dependence,
maintenance therapy is currently considered to be the first-line treatment for such
patients (O'Connor 2005). Opioid-assisted maintenance programs have been introduced
in most countries of the world, yet the medication of choice differs from one country to
the next. Methadone is the most extensively studied and most widely used opioid in
maintenance treatment. Other μ-opiate agonists that are used include levoacethylmethadol
(LAAM), codeine, slow-release oral morphine and diacetylmorphine,
as well as the partial μ-opioid agonist buprenorphine.
Methadone as a maintenance agent
Methadone maintenance treatment constitutes an effective treatment modality in
reducing illicit opiate use, although not all patients benefit from methadone substitution,
indicated through further illicit heroin use (Gowing et al. 2001). Nevertheless, several
pre- and post-treatment outcomes confirmed the effectiveness of methadone
maintenance treatment in a wide range of age and ethnic groups of patients and showed
that MMT leads to higher retention rates and longer treatment duration than placebo or
no treatment.
Even lower doses (≤ 20 mg methadone) were found to be more effective in retaining
individuals in treatment than placebo or no treatment (Connock et al. 2007). Methadone
dosages ranging from 60 to 100 mg/day were found to be more effective than lower
dosages in terms of treatment retention and reduction of heroin and cocaine use during
treatment (Connock et al. 2007). Higher doses (60 mg - 110 mg) of methadone are in
general associated with a lower number of opioid-positive urine samples than moderate
and lower doses (< 40 mg) (Connock et al. 2007). Indeed, lower doses of methadone
seem to be sufficient to stabilise the patient and might be helpful to keep the patient in
treatment, but are inadequate to suppress opiate use (Kleber et al. 2006). In comparison,
the treatment retention rates are higher with moderate doses of 40-60 mg/day of
methadone, which are normally necessary to suppress the opioid withdrawal symptoms
(Kleber et al. 2006). Higher methadone doses are needed during maintenance treatment
to block craving for opiates and illicit drug use (Donny et al. 2005), and especially
heroin addicts with axis 1 disorders benefit from high methadone doses (≥ 100 mg/day)
(Kleber et al. 2006). Yet, one effectiveness report from outside of Europe found no
significant difference in the retention rate between patients with moderate (≥ 40-50
mg/day) and high methadone doses (≥ 80-100 mg/day), maybe due to a plateau of dose
related efficacy of methadone, but marked declines in self-reported illicit drug use in
both groups (Kleber et al. 2006). As the illicit drug use significantly declines in patients
with higher methadone doses, the explanation of a plateau of dose related efficacy of
methadone is only valid for the retention rates (Kleber et al., 2006). However, adequate
daily dosing has an important effect on retention in methadone maintenance treatment
(Anderson & Warren 2004). In the US, low dosages of methadone have to a large extent
been replaced by higher dosages: In 1988, almost 80% of the patients received dosages
of less than 60 mg/day, in 2000, this was the case in 36% of the cases (D'Aunno &
Pollack 2002). Suboptimum methadone doses lead to a lower retention rate, and when
patients remain in treatment, MMT reduces heroin use, delinquency, and HIV-related
risk behaviour and HIV transmission (Ward et al. 1999). Nonetheless, since very high
dosages of methadone have also been associated with the occurrence of Torsade de
Pointes (TdP), high dosages need to be monitored carefully (Krantz et al. 2002).
However, sporadic cases of TdP have also been reported in patients receiving a
recommended dose between 60 and 100 mg methadone per day (Pearson & Woosley
2005) and the risk of death caused by overdoses in heroin users seems to substantially
reduce after stabilisation on methadone (Gowing et al. 2001).
MMT seems to be superior to methadone detoxification treatment or outpatient drugfree
treatment in reducing heroin use, criminal behaviour and risky sexual behaviour
and is associated with greater retention in treatment than therapeutic communities,
outpatient drug-free treatment or naltrexone treatment (Gowing et al. 2001).
Observational studies suggested that the treatment retention is better in a take-home
approach with corresponding doses of methadone and reduced frequent treatment centre
visits (Gowing et al. 2001).
Opioid dependence is commonly associated with psychiatric co-morbidities like
depression and, therefore, associated with poor outcomes. Dean et al. (2004) used a
double-blind, double dummy, randomised controlled trial design to examine whether
heroin users maintained on buprenorphine demonstrate greater improvement in
depressive symptoms than those on MMT (Dean et al. 2004). Contrary to former
findings, which reported depression as a side effect of buprenorphine or described
greater depressive symptom improvement with methadone, no differential benefits of
buprenorphine compared to methadone were found on depressive symptoms in heroin
users engaged in maintenance treatment (Dean et al., 2004). However, a conclusion
based on these results could not be made and requires further investigations. Flexible
doses of methadone were found to be more effective than flexible doses of
buprenorphine for maintenance treatment, maybe because of the higher potential of
methadone to suppress heroin use, especially if high-doses of methadone are used
(Connock et al. 2007; Mattick et al. 2007). Compared to buprenorphine maintenance
treatment, the administration of an average maximum dose of 80 mg methadone leads to
higher treatment durations, longer periods of sustained abstinence and a greater
proportion of cocaine- and opioid-free urine samples than liquid buprenorphine in an
average maximum dose of 15 mg (Schottenfeld et al. 2005). Furthermore, MMT is
associated with a reduction of self-reported adverse effects, a reduction of the relative
mortality risk, an improvement of HIV-related behaviour and a reduction of
delinquency (Gowing et al. 2001; Johnson et al. 2003).
In summary, methadone is the best-studied and most effective opioid agonist for
maintenance treatment so far. Treatment outcome in methadone maintenance has been
shown to improve substantially with increased dosages of methadone. Adequate dosing
is an important issue and avoids on the one hand unpleasant withdrawal symptoms,
especially in the latter half of each inter-dosing interval, and on the other hand
significant adverse effects. The combination with psychosocial treatment such as
counselling and behavioural interventions leads to a broader effectiveness and a greater
range of treatment outcomes such as reduced craving, reduction of illicit drug use and
drug-related delinquency, improvement of health and well-being and reduction of drug
related harm. However, even methadone maintenance treatment without adequate
psychosocial care as an interim solution until entry into a comprehensive methadone
maintenance treatment programme has shown to increase the likelihood of entry into
comprehensive treatment and reduce heroin use and delinquency (Schwartz et al. 2006;
Teesson et al. 2006).
Buprenorphine as a maintenance agent
Buprenorphine proved to be effective and clinically useful in the maintenance treatment
of opioid dependence. Compared to placebo, buprenorphine was found to be an
effective agent for the treatment of opioid dependence in a maintenance approach and
several studies have shown efficacy of buprenorphine in maintenance treatment of
opioid dependence (Ling & Wesson 1984; Mattick et al. 2007). Like methadone, the
efficacy of buprenorphine is dose-related: Higher doses of buprenorphine showed better
outcomes than lower doses, although these differences were not always robust in their
values (Kleber et al. 2006). Low and moderate doses (2 - 8 mg) of buprenorphine are
superior to placebo in the measures of treatment retention, provision of opioid-negative
urine samples, mortality, and psychological and social functioning (Kleber et al. 2006).
When using equipotent doses, the efficacy of buprenorphine in the maintenance
treatment of opioid dependents is comparable to that of methadone (Kleber et al., 2006).
Therefore no significant differences were found between low dose buprenorphine and
low dose methadone with regard to treatment retention, opiate free urine samples and
self-reported heroin use (Mattick et al., 2007), whereas moderate doses of
buprenorphine are superior to low doses of methadone (Kleber et al. 2006). In general
contrary to these dose-related results, Connock et al. found that methadone in
comparable and especially in flexible doses is superior to buprenorphine with regard to
treatment retention, with the exception of lower doses (Connock et al. 2007).
The maximum therapeutic effect of sublingual buprenorphine tablets occurs in the range
of moderate (8 mg) to higher doses (16 mg), comparable to moderate methadone doses
of 40-60 mg (Kleber et al. 2006). In flexible dosage, methadone is significantly more
effective than buprenorphine in retaining patients in treatment, perhaps because of the
higher potential of methadone to suppress heroin use, especially if high doses of
methadone are used (Mattick et al. 2007).
Methadone seems to be superior to buprenorphine in the maintenance treatment of
opioid dependents with co-occurring cocaine dependence (Schottenfeld et al. 2005). The
administration of an average maximum dose of 80 mg methadone leads to higher
treatment durations, longer periods of sustained abstinence and a greater proportion of
cocaine- and opioid-free urine samples than liquid buprenorphine in an average
maximum dose of 15 mg (Schottenfeld et al. 2005). However, Montoya et al. (2004)
showed in their double-blind, controlled clinical trial with strict eligibility criteria that
daily doses of 8 and 16 mg of buprenorphine solution in combination with drug abuse
counselling are feasible and effective in maintenance treatment of outpatients with cooccurring
opioid and cocaine dependence (Montoya et al. 2004).
The longer duration of therapeutic action of buprenorphine provides the advantage of a
less than daily schedule, however, the comparison of daily vs. intermittent
administration lead to different results. Some findings showed no increase of
buprenorphine doses under intermittent administration, while others found a doubling of
doses (Kleber et al. 2006). However, another trial found that intermittent doses for 48-
hours provide adequate effects and are preferable to daily dosing (Kleber et al. 2006).
From a clinical point of view, dosing of buprenorphine on every fourth day is possible
and was found to lead to similar effects on the measures of adverse effects and efficacy
than daily doses (Kleber et al. 2006). A recent controlled trial confirmed these results
(Marsch et al. 2005). In this comparison no differences were found between one per
day, three times a week and twice a week administration of buprenorphine regarding
treatment retention and opiate use (Marsch et al. 2005). However, the less-than-daily
schedule with adapted doses was found to be effective, is often preferred by the patient
and provides the opportunity to serve a greater number of opioid-dependent patients.
The efficacy of buprenorphine maintenance treatment was found to be comparable to
methadone maintenance with advantages in some treatment settings, in alternate day
dosing, better safety profile, and milder withdrawal syndrome (Mattick et al. 2007). In
two small-scale studies, buprenorphine prescription in primary care was associated with
good retention (70-80%) and reasonable rates of opiate free urines (43-64% achieving
three or more consecutive weeks of opiate free urines) (Fiellin et al. 2002; O'Connor et
al. 1996). These positive effects were confirmed in a larger trial, showing a reduction of
opiate use and craving under buprenorphine (Fudala et al. 2003). Similar results were
obtained in France some years ago (Duburcq et al. 2000). Buprenorphine reduced the
risk of overdose related death compared to methadone (Kleber et al. 2006; Simoens et
al. 2000) and was found to reduce mortality in maintenance treatment (Auriacombe et
al. 2001). However, recently, Lofwall et al. (2005) examined the safety and side effect
profiles in 164 opioid dependents in buprenorphine and methadone outpatient treatment.
After randomisation to buprenorphine (n = 84) or to methadone (n = 80) all patients
were maintained for 16 weeks. Besides very few clinical gender differences, common
profiles of safety and side effects were found for both groups (Lofwall et al. 2005).
Connock et al. (2007) found in their recent health technology assessment no
generalisable results in the comparison of methadone and buprenorphine with regard to
mortality (Connock et al. 2007). In general, buprenorphine is associated with lower
levels of withdrawal symptoms than heroin or methadone (Gowing et al. 2001).
In general, maintenance treatment with buprenorphine provides some advantages for the
treatment of opioid dependence in comparison to methadone, e.g. a better safety profile
at high doses, a lower abuse potential, the possibility of a less-than-daily administration
and lower impairment in psychomotor and cognitive functioning. Similar to methadone,
the efficacy of buprenorphine in maintenance treatment is dose related; higher doses of
buprenorphine (12 mg/day or more) improve the treatment retention and reduce illicit
heroin use. Provided in effective doses, buprenorphine appears to be at least as effective
as methadone with regard to reduction of illicit opioid use and treatment retention,
whereas methadone maintenance in high doses is associated with higher rates of
retention in treatment and better suppression of withdrawal symptoms than
buprenorphine maintenance treatment (Mattick et al. 2007). The recent Cochrane review
recommends that buprenorphine maintenance should be supported as a maintenance
treatment, when higher doses of methadone cannot be administrated (Mattick et al.
2007). However, Marsch et al. (2005) demonstrated that predictors of treatment success
of LAAM, buprenorphine, and methadone appear to be largely comparable, and they
did not detect any factors that would prefer one medication over the others (Marsch et
al. 2005).
Buprenorphine-naloxone combination as a maintenance agent
The buprenorphine-naloxone combination contains the partial opiate agonist and
antagonist buprenorphine as well as the opioid antagonist naloxone to deter illicit
intravenous preparation of the tablet. This is intended to attenuate the effects of
buprenorphine on opioid-naive users should this formulation be injected.
Fudala et al. (2003) used a randomised blinded placebo-controlled trial design including
4-week follow-up to demonstrate that sublingual tablet formulation of buprenorphine
and naloxone is effective for the treatment of opiate dependence compared to placebo
(Fudala et al. 2003). Recently, Mintzer et al. (2007) showed the feasibility and efficacy
of buprenorphine-naloxone treatment in primary care settings (Mintzer et al. 2007).
An Australian pilot study showed the tolerability and feasibility of unsupervised
administration of buprenorphine-naloxone combination tablets in the maintenance
treatment of opioid dependence (Bell et al. 2004). Another double-blind crossover study
found only minor impairment with buprenorphine-naloxone administration in the
highest dose of 32 mg/8 mg (Mintzer et al. 2004). However, both recent studies
included only a small number of patients and further investigations are needed with
larger sample sizes in a control group design to confirm these findings. Both for
methadone or buprenorphine maintenance alone, new research focuses on the
improvement of adherence through additional psychosocial treatment. Fiellin et al.
(2006) conducted a 24-week randomised, controlled clinical trial with 166 patients to
investigate the effect of adding two different kinds of counselling to buprenorphinenaloxone
maintenance therapy for opioid dependence (Fiellin et al. 2006). The
participants were randomly allocated to a brief, manual-guided, medically focused
counselling and either once-weekly or thrice-weekly medication or enhanced medical
management with extended sessions and thrice-weekly medication dispensing. The
patients in all three treatment types showed significant reductions of illicit opioid use,
although no differences were found regarding opioid-negative urine samples, the
duration of abstinence from illicit opioids and the retention in treatment. The efficacy of
buprenorphine in combination with naloxone seems to be comparable to buprenorphine
alone in the maintenance treatment of opiate dependency. Patients treated with
buprenorphine and naloxone showed lower rates of opiate-positive urine samples,
showed fewer craving symptoms for opiates, and greater improvement in overall health
and well-being than patients who received placebo.
Slow-release oral morphine as maintenance agent
Slow release oral morphine (SROM) acts as an agonist on the μ-receptor and the long
duration of action permits to administer a once-a-day preparation. SROM has been
authorized for maintenance treatment of opioid dependence mainly in a few European
countries. Only little evidence was found from outside of Europe. Jones et al. (2005)
showed in their recent randomised trial the feasibility and safety of switching opioiddependent
pregnant women from short-acting morphine to buprenorphine or methadone
during the second trimester3 of pregnancy (Jones et al. 2005). Further studies will have
to confirm these results in order to be able to evaluate the added value of this substance
for the treatment of heroin dependence. In summary, SROM might be a promising
compound for maintenance treatment. Further details are provided in the respective
European chapter.
Pharmacotherapy for relapse prevention
Naltrexone for relapse prevention
The opiate antagonist naltrexone is indicated for prescription for those who have
achieved abstinence. In a human laboratory setting, naltrexone showed to be effective to
block the effects of short acting opioids such as heroin (Kleber et al. 2006). Low doses
of naltrexone had no discernible advantage, and participants preferred 50 mg per day.
Despite the preference of patients for blocking doses of oral naltrexone (like 50 mg per
day), the effectiveness of naltrexone appeared not to be dose related (Rea et al. 2004).
Due to the prevention of the euphoria effect of opiates, outpatient double-blind placebo
controlled trials with long-acting opiate antagonist are very uncommon. Placebocontrolled
trials showed extremely high dropout rates, which implicates that the general
acceptability of the participants is low (Kleber et al. 2006). On the other hand, the high
drop out rates lead to highly selective patient samples in most of the naltrexone
maintenance studies and it could not be precluded that these groups of patients have a
high level of motivation (Kleber et al. 2006). Indeed, the retention in treatment was
found to be the most important predictor for the effect of naltrexone in treating opioid
dependence, and authors therefore propose to add counselling to naltrexone
maintenance treatment (Ritter 2002). O’Brien et al. (2005) suggested in their metaanalytic
review that medications for relapse prevention are most effective in the context
of counselling, therapeutic and behavioural techniques (O'Brien 2005). However, Nunes
et al. (2006) concluded in their recent randomised control trial that there may be a limit
on the extent to which behavioural therapy can overcome poor adherence to oral
naltrexone (Nunes et al. 2006): The authors investigated the effectiveness of
Behavioural Naltrexone Therapy (BNT) including voucher incentives, motivational and
cognitive behavioural therapies. Sixty-nine patients were randomly administrated to the
admission of BNT or to a standard treatment control including compliance
enhancement. In both groups, treatment retention after six months was low (22% BNT
vs. 9%), whereas most patients remaining in treatment after three months achieved
abstinence from opioids (Nunes et al. 2006). Tucker et al. (2004) found no reasonable
effects, although the provision of an additional 12-week manualised group-counselling
programme including a cognitive-behavioural relapse prevention approach provides
additional benefit to naltrexone treatment (Tucker et al. 2004).
An alternative strategy to improve the retention rates is the administration of sustainedrelease
depot formulation of naltrexone instead of oral naltrexone in treating opioid
dependence. A recent randomised controlled trial found promising results (Comer et al.
2006): Sixty heroin-dependent males and females were randomly allocated to placebo
or 192 or 384 mg of depot naltrexone, including twice weekly relapse prevention
therapy for all participants. The sustained-release depot formulation of naltrexone was
well tolerated. After two months, 60-68% of patients in the 192 mg of naltrexone and
384 mg of naltrexone groups, respectively, remained in treatment compared to 39% of
the placebo group. The mean dropout time was dose related, varying between 27 days
for the placebo group and 48 days for the 384 mg of naltrexone group. However, the
study sample was small and no direct comparison with oral naltrexone was provided, so
that the potential advantages should be regarded as promising but not proven. The
former assumption that the combination of naltrexone with a Selective Serotonin Reuptake
Inhibitor (SSRI)4 is more effective than naltrexone alone, could not be
confirmed in recent randomised, placebo-controlled trials (Farren & O'Malley 2002). A
recent primarily double-blind, placebo controlled RCT with a small number of patients
suggests that the additional administration of lofexidine to oral naltrexone leads to
higher opioid abstinence rates and improved relapse outcomes as compared to the
combination of placebo and naltrexone (Sinha et al. 2007). However, these promising
results have to be proven in larger sample sizes.
Naltrexone is considered to be a safe medication with few side effects; only high doses
can lead to transaminase elevations in liver function tests (Kleber et al. 2006). Two
other issues related to the prescription of naltrexone deserve special attention: the
potential induction of depression by naltrexone, and the overdose risk following
discontinuation of a naltrexone treatment. A systematic review of the available literature
found no evidence for a relationship between naltrexone and depression or anhedonia,
but found that reduced opiate tolerance following naltrexone treatment may indeed
increase the risk of heroin overdose (Dean et al. 2006; Ritter 2002). Therefore, a clear
warning to patients treated with oral naltrexone regarding the risk of heroin overdose is
warranted. One possibility to avoid this risk is the administration of long acting
sustained release naltrexone implants. Hulse et al. (2005) showed a reduced number of
opioid overdoses observed in the 6-12 months post-implant treatment (Hulse et al.
2005). However, a most recent case report indicates that patients can die from an opioid
overdose with a naltrexone implant and blood naltrexone levels higher than reported
blockade levels (Gibson et al. 2007).
In summary, the effectiveness of antagonist maintenance with oral naltrexone for opioid
dependence has been limited by high dropout rates. This conclusion is corroborated by
the findings of the National Evaluation of Pharmacotherapies for Opioid Dependence
(NEPOD) in Australia, which showed that only 4% of the patients in naltrexone
maintenance treatment were still in treatment after six months (NDARC 2001).
Furthermore, patients preferred relapse prevention treatment with buprenorphine or
methadone (Digiusto et al. 2005). Naltrexone maintenance seems not to be effective as a
stand-alone treatment and should be, therefore, part of a broader treatment programme
or should be reserved only for highly motivated patients living in a stable life situation.
Nevertheless, a promising strategy to improve treatment retention in broader range
could be the combination of long-acting implantable naltrexone formulations and
behavioural methods.
5.2 Pharmacotherapy for the treatment of stimulant-related disorders
In summary, non of the proofed medication has been found yet that can be considered a
standard for treating stimulant dependence effectively, although a number of different
medications has been tried (Kleber et al. 2006). The treatment of cocaine dependence
frequently still includes the use of antidepressants, especially SSRIs, despite the low
evidence level for their efficacy. Some typical and atypical psychotic agents such as
haloperidol, olanzepine and risperidone, were found to be effective in the treatment of
patients with co-occurring schizophrenia and cocaine dependence. Also promising
results are expected from topiramate and other antiepileptic drugs, and much hope is
being placed in the development of the cocaine vaccine.
Detoxification treatment for stimulant-related disorders
Symptoms of intoxication are treated in different ways. Labetalol, an alpha-1 and beta
adrenergic blocker used to treat high blood pressure, has been used for treating
symptoms of cocaine intoxication, but the little clinical research shows that the use of
adrenergic blockers and dopaminergic antagonists should be used carefully in acute
cocaine intoxication (Kleber et al. 2006). Benzodiazepines (such as Oxazepam,
Alprazolam) are given those cocaine users with acute intoxication who are very agitated
(Kleber et al. 2006).
One way of treating withdrawal symptoms during detoxification, such as sleep
difficulties, symptoms of depression, anxiety, anhedonia is to give dopamine agonists
(e.g. amantadine), but research findings have been ambiguous, with two studies finding
positive effects and two others with no significant effect (Kleber et al. 2006). The same
is true for bromocriptine that acts as a dopamine agonist. Bromocriptine has potential
use in treating cocaine addiction, since the addictive effects of cocaine are caused by it
blocking dopamine reuptake. First studies seemed to be promising, until a double-blind
RCT found a higher rate of negative urine-samples but higher dropout rate with
bromocriptine than amantadine, an antiviral drug, releasing dopamine from the nerve
endings of the brain cells (Kleber et al. 2006). Another double-blind RCT found no
significant differences between bromocriptine and placebo concerning reduction of
cocaine use (Kleber et al. 2006). One uncontrolled inpatient study found no reduction of
craving with bromocriptine (Kleber et al. 2006). Therefore, the UNODC report
(UNODC 2002) comes to the conclusion that there is no significant effect of both
bromocriptine and amantadine. For patients with relatively severe withdrawal
symptoms, propranolol has showed some effect (Kleber et al. 2006).
Antipsychotic medication has been prescribed and reported to be somewhat effective in
treating cocaine-related delusions, but most patients recover from delusions without
medication after a few hours (Kleber et al. 2006. No evidence has been found that
anticonvulsants reduce cocaine-induced seizures (Kleber et al. 2006). Gillman et al.
(2006) found reduced cocaine withdrawal symptoms in cocaine dependents treated with
psychotropic analgesic nitrous oxide (PAN), a titrated mixture of oxygen and nitrous
oxide (Gillman et al. 2006).
A recent placebo-controlled pilot study investigated the safety and efficacy of
mirtazapine, an antidepressant used for the treatment of moderate to severe depression,
in amphetamine detoxification (Kongsakon et al. 2005). Twenty amphetamine
dependents were randomly allocated to either mirtazapine treatment (9 patients) or
placebo (11 patients), of which seven patients in the mirtazapine and nine in the placebo
group completed the study. Patients in the mirtazapine group showed significant
improvements in the total Amphetamine Withdrawal Questionnaire (AWQ)5 score
versus placebo at days 3 and day 14. Despite reported mild adverse events like headache
etc. and the small sample size the authors suggested, that mirtazapine may be an option
for amphetamine detoxification treatment (Kongsakon et al. 2005).
Substitution treatment for stimulant-related disorders
Different approaches have been considered for replacement therapy in the treatment of
cocaine dependence. Replacement therapies with methylphenidate or sustained-released
amphetamine showed better patient retention and greater reduction in cocaine use
compared to placebo, but further studies are needed (Kleber et al. 2006). Buprenorphine
has been tried with those patients with double dependence (opiate and cocaine) and
showed some effect on cocaine use in open trials but not in double-blind studies (Kleber
et al. 2006). Montoya et al. (2004) showed reducing concomitant opiate and cocaine use
under the provision of 16 mg daily doses of sublingual buprenorphine solution
(Montoya et al. 2004). Schottenfeld et al. (2005) found significantly longer treatment
retention rates, longer periods of sustained abstinence and a greater proportion drug-free
tests in co-occurring cocaine and opioid dependents maintained with methadone than
patients assigned to receive buprenorphine (Schottenfeld et al. 2005).
Stoops et al. (2007) recently indicated that acute d-amphetamine pre-treatment does not
increase stimulant self-administration (Stoops et al. 2007). Grabowski et al. (2004)
conducted two studies to investigate efficacy of sustained release d-amphetamine as
well as risperidone (an atypical antipsychotic medication for cocaine dependence), each
in combination with methadone in 240 (120/study) cocaine and heroin co-dependents,
which randomly allocated to one trial medication or placebo (Grabowski et al. 2004).
All patients underwent a methadone induction, were stabilised at 1.1mg/kg and received
one behavioural therapy session per week. The combination of the methadone and damphetamine
was found to be significantly more effective than methadone and placebo,
and also better than methadone and risperdione for treatment of concurrent cocaine and
opioid dependents (Grabowski et al. 2004).
Methylphenidate (MPH), a prescription stimulant commonly used to treat attentiondeficit
hyperactivity disorder (ADHD), was recently found to be effective for reducing
intravenous drug use in patients with severe amphetamine dependence respectively
cocaine use in patients with cocaine dependence (Levin et al. 2007; Tiihonen et al.
2007). Furthermore, methylphenidate can be safely provided in an outpatient setting
with active cocaine users (Winhusen et al. 2006).
Recently, Collins et al. (2006) found that the provision of up to 20mg memantine, a
non-competitive N-methyl-d-aspartate (NMDA) antagonist, did not alter the subjective
or reinforcing effects of cocaine in methadone-maintained cocaine smokers (Collins et
al. 2006). Also, the maintenance treatment with gabapentin, a medication originally
developed for the treatment of epilepsy, did not alter the choice to self-administer
cocaine by treatment-seeking cocaine-dependent individuals and was found not to be
clinically useful for the treatment of cocaine and methamphetamine dependence (Haney
et al. 2005; Hart et al. 2007; Hart et al. 2007a; Hart et al. 2004; Heinzerling et al. 2006).
Also, baclofen, a GABA-ergic compound, was found to be ineffective at suppressing
self-administration, especially in more intensive cocaine users and seems to have only a
small therapeutic effect for the treatment of methamphetamine dependence compared to
placebo (Heinzerling et al. 2006).
Abstinence maintenance for stimulant-related disorders
No medication has shown clear efficacy in treating cocaine dependence (Kleber et al.
2006), and no antagonists have been found yet to be effective (UNODC 2002).
However, patients with severe forms of dependence and severe withdrawal symptoms
or those not responding to psychosocial treatment may find medication to be useful for
them (Kleber et al. 2006).
Shoptaw et al. (2006) indicated that the antidepressant sertraline is contraindicated for
the treatment methamphetamine dependence due to significant more adverse events
compared to placebo conditions (Shoptaw et al. 2006). Newton et al. (2006) suggested
that the antidepressant bupropion has some effectiveness in reducing
methamphetamine-induced subjective effects and cue-induced craving (Newton et al.
2006). Newton et al. (2006) found reduced acute methamphetamine-induced subjective
effects and reduced cue-induced craving under the administration of bupropion, an
atypical antidepressant that acts as a norepinephrine and dopamine reuptake inhibitor,
and nicotinic antagonist (Newton et al. 2006). Furthermore buprion was found to be
well-tolerated by patients and seems to alleviate the cardiovascular effects of
experimentally administered methamphetamine (Newton et al. 2005).
The selective serotonin reuptake inhibitor fluoxetine and the dopamine reuptake
inhibitor bupropion had some benefit in small studies but not in larger trials (Kleber et
al. 2006). The tricyclic antidepressant desipramine has been studied with inconsistence
findings, some studies showing positive effects others not. One study compared
desipramine with placebo and found a short term effect of 6 weeks but not at 12 weeks
or longer (Kleber et al. 2006). Several recent clinical trials confirmed, that the use of
antidepressants such as paroxetine, reboxetine, nefazodone, sertaline, and venlafaxine
do not support the treatment of cocaine dependence (Ciraulo et al. 2005; Ciraulo et al.
2005a; Passos et al. 2005; Winhusen et al. 2005). Desipramine, a tricyclic
antidepressant (TCA) that inhibits the reuptake of norepinephrine, is associated with
depression improvements and therefore with improvements in cocaine use in treatment
of cocaine-dependents with depression in an outpatient setting (McDowell et al. 2005).
However, the administration with desipramine lead to higher dropout rates due to side
effects and medical adverse events (McDowell et al. 2005).
After some initial promising results, the anticonvulsant carbamazepine had no effects in
later double-blind placebo-controlled studies (Kleber et al. 2006). In recent clinical
trials the anticonvulsants valproate, lamotrigine, and gabapentin were found to be not
more effective than placebo in treating cocaine dependence (Berger et al. 2005; Bisaga
et al. 2006; Gonzalez et al. 2007; Reid et al. 2005). For the utility of divalproex (an
anticonvulsant and mood-stabilising drug) in patients with bipolar disorder and primary
cocaine dependence further high quality experimental, placebo-controlled studies are
warranted to confirm the promising results of a first pilot study (Salloum et al. 2007).
Tiagabine, an anti-convulsive medication, has been shown to lead to reduced positive
urine samples in patients treated for cocaine dependence compared to placebo and may
merit further study, although the patients of a recent trial showed difficulties in
tolerating low dose of tiagabine (Gonzalez et al. 2007; Winhusen et al. 2005).
Topiramate, an anticonvulsant drug, showed recently some promising results in one
double-blind study (Kleber et al. 2006) and Kampman et al. (2004) demonstrated that
topiramate-treated patients were more likely to be abstinent from cocaine compared to
placebo-treated (Kampman et al. 2004).
The GABA agonist baclofen has shown some minor effect (Heinzerling et al. 2006),
and one double-blind clinical trial with tiagabine showed more effect than placebo in
reducing cocaine use (Kleber et al. 2006). The narcoleptic medication modafinil has
shown some effects, but needs further studies (Kleber et al. 2006). Modafinil blocked
the euphoric effects of cocaine, significantly decreased systemic exposure to cocaine
during the first 180 minutes following intravenous cocaine administration and improves
clinical outcome when combined with psychosocial treatment for cocaine dependence
(Dackis et al. 2005; Donovan et al. 2005; Ginsberg 2005). Malcolm et al. (2006) found
in their recent clinical trial6 no significant hemodynamical interactions between
modafinil and cocaine, but further outpatient trials appeared to be warranted (Malcolm
et al. 2006). The systematic review by the APA describes mixed results on dopamine
agonists: amantadine, an antiviral drug, has been best studied but with no overall
benefit, only in some studies (Kleber et al. 2006). Kampman et al. (2006) used a doubleblind,
placebo-controlled design to evaluated the efficacy of amantadine, propranolol, a
non-selective beta blocker mainly used in the treatment of hypertension, and their
combination in one hundred and ninety-nine cocaine dependent patients with severe
cocaine withdrawal symptoms (Kampman et al. 2006). Neither propranolol nor
amantadine or their combination was found to be significantly more effective than
placebo in promoting abstinence from cocaine in these extremely difficult-to-treat
patients, whereas highly adherent patients to study medication showed better treatment
retention and higher rates of cocaine abstinence under the provision of propranolol
compared to placebo (Kampman et al. 2006).
Reid et al. (2005) found no effectiveness of the atypical antipsychotic agent olanzapine
for the treatment of cocaine dependence with regard to cocaine use, as measured by
urine Benzoylecgonine (BE)7 levels and self-report (Reid et al. 2005) and risperidone,
another atypical antipsychotic medication, were found to be insufficient in reducing
cocaine craving in cocaine dependents (Smellson et al. 2004). The partial dopamine
agonist aripiprazole have shown promising results in a small clinical trial regarding
subject-related and cardiovascular effects, but further research is needed to confirm the
effectiveness (Lile et al. 2005). However, typical and atypical psychotic agents such as
haloperidol, olanzepine and risperidone, were found to be effective in the treatment of
patients with co-occurring schizophrenia and cocaine dependence (Albanese & Suh
2006; Rubio et al. 2006; Sayers et al. 2005; Smelson et al. 2006). Stoops (2006)
indicated that the aripiprazole, an atypical antipsychotic medication approved for the
treatment of schizophrenia and acute manic and mixed episodes associated with bipolar
disorders, may have clinical utility in treating stimulant dependence, but large-scale
clinical trials are needed to confirm the efficacy (Stoops 2006). Otherwise, mazindol, a
catecholamine reuptake inhibitor and antipsychotic agent, was fount to be ineffective in
reducing cocaine consumption, cocaine craving, and psychiatric symptoms in patients
diagnosed with comorbid schizophrenia and cocaine abuse or dependence (Perry et al.
2004).
Dopamine agonists like selegiline, l-dopa/carbidopa, pergolide had inconclusive or
negative findings and altogether no superiority to placebo (Kleber et al. 2006) and also
recent findings did not confirm the support for the efficacy of dompamine agonists for
the treatment of cocaine dependence (Ciraulo et al. 2005; Focchi et al. 2005; Gorelick &
Wilkins 2006). However, Shoptaw et al. (2005) found good results for cabergoline, a
potent dopamine receptor agonist, regarding improvements in addiction severity and
negative urine samples for cocaine metabolites and provided empirical support for
conducting a larger study of the medication (Shoptaw et al. 2005).
The opiate antagonist naltrexone has not been found useful for treatment of cocaine
dependence (Kleber et al. 2006; Schmitz et al. 2004). Schmitz et al. (2004) found, that
50 mg/day of naltrexone failed to reduce either cocaine or alcohol use in co-occurring
cocaine and alcohol abusers, whereas psychotherapy significantly reduced cocaine use
during the first 4 weeks of treatment (Schmitz et al. 2004). Baker et al. (2007) found
that the administration of disulfiram reduced cocaine-associated subjective effects
(‘high’ and ‘rush’) (Baker et al. 2007). Carroll et al. (2004) showed that the provision of
disulfiram alone and in combination with cognitive behaviour therapy (CBT) is
effective in reducing cocaine use in cocaine-dependent outpatients (Carroll et al. 2004).
Several further medications were recently investigated with regard to their efficacy for
treatment of cocaine dependence. Progesterone, a steroid hormone, attenuated some of
the physiological and subjective effects of cocaine, but further studies are warranted to
assess the efficacy (Sofuoglu et al. 2004). High doses of dehydroepiandrosterone, a
natural steroid prohormone, seems to be contraindicated as a pharmacotherapy for
cocaine dependence due to increasing cocaine use compared with placebo (Shoptaw et
al. 2004). Tryptophan, an essential amino acid, did not significantly prevent relapse to
cocaine use or attenuate cocaine use after relapse (Jones et al. 2004). Levodopa (Ldopa),
an intermediate in dopamine biosynthesis, and amlodipine, a calcium channel
blocker, were found to be not superior to placebo in reducing cocaine use (Malcom et
al. 2005; Mooney et al. 2007). Also selegiline, a drug used for the treatment of
Parkinson's disease, does not support the treatment of cocaine dependence (Elkashef et
al. 2006), as well as celecoxib, a non-steroidal anti-inflammatory drug (Reid et al.
2005).
Immunisation and vaccination are two strategies with a long tradition and very little
empirical proof of effectiveness (Kantak 2003). In (passive) immunisation, catalytic
antibodies are injected that bind cocaine and subsequently hydrolyse cocaine into the
inactive products ecognine methyl ester and benzoic acid. A cocaine vaccine has also
been proposed; this would attempt to block the effects of cocaine using cocaine
antibodies (Bagasra et al. 1992). This unique approach to the pharmacotherapy of
cocaine addiction was initiated by immunisation experiments that demonstrated specific
cocaine antibody production in animals (Carrera et al. 1995; Carrera et al. 2000; Fox
1997; Fox et al. 1996). Cocaine-specific antibodies can sequester cocaine molecules in
the bloodstream, thereby allowing naturally occurring enzymes (cholinesterases) to
convert cocaine into inactive metabolites, which are then excreted. As the antibodies
cannot cross the blood-brain barrier, the vaccine is not expected to have any direct
psychoactive effect. As the antibodies prevent cocaine from having an effect, the
reinforcing effect of continued cocaine use would be dampened. Furthermore, the
vaccine persists for months, so there is no need for daily administration of medication.
A randomised, double-blind, placebo-controlled clinical trial involving 34 former
cocaine users was carried out to assess the safety and immunogenicity of the therapeutic
cocaine vaccine TA-CD (Kosten & Biegel 2002). The results of this trial showed that
the vaccine induced cocaine antibodies in a time- and dose-dependent manner and that it
was well tolerated with no serious adverse events during 12 months of follow-up. This
trial was then followed up by an open-label, 14-week, dose escalation study evaluating
the safety, immunogenicity and clinical efficacy of the cocaine vaccine (Martell et al.
2005). Ten cocaine-dependent subjects received a total dose of 400 μg of vaccine in
four injections over the course of 8 weeks and eight cocaine-dependent subjects
received a total dose of 2 000 μg of vaccine in five injections over the course of 12
weeks. The results showed a high completion rate, no serious adverse events, good
tolerance and a significantly higher likelihood of cocaine-free urine in the high-dose
group at 6 months. The results are most encouraging when compared with other
pharmacological strategies, but will have to be replicated in further studies.
Pharmacotherapy for the treatment of cannabis related disorders
Neurobiological trials on cannabis withdrawal demonstrate the importance of the
development of further pharmacological options for the treatment of cannabis
dependence. Different published studies have employed laboratory animals to evaluate
medication effects on cannabinoid withdrawal symptoms. Nevertheless clinical trials of
human participants are rare and none of the included effectiveness reports found clinical
trials supporting a medication for the pharmacotherapy of cannabis dependence (Kleber
2003; UNODC 2002). Some findings suggest that oral delta-9-tretrahydrocannabinol
(THC) might be helpful in suppressing cannabis withdrawal (Budney et al. 2007). In a
recent clinical trial eight daily cannabis-using adults were randomly allocated to placebo
or lower dose of THC (30 mg) or higher doses of THC (90 mg) during three 5-days
periods of abstinence from cannabis. A lower daily dose of THC reduced withdrawal
discomfort, where as higher daily doses showed a greater effect in suppressing
withdrawal symptoms (Budney et al. 2007). These results replicated the findings of
another clinical trial that demonstrated that THC administration beginning on the first
day of marijuana abstinence lead to decreased symptoms of cannabis withdrawal, like
anxiety, misery, chills or self-reported sleep disturbance, relative to placebo (Haney et
al. 2004). Oral THC also decreased marijuana craving during abstinence compared to
placebo. The same study investigate the effect of the mood stabiliser divalproex to
attenuate a broader range of cannabis withdrawal symptoms, compared to
antidepressants, such as nefazodone and burpropion (Haney et al. 2004). As like
bupropion, maintenance with divalproex prior to and during marijuana abstinence also
markedly worsened mood such as irritability, edginess, anxiety and sleepiness (Haney et
al. 2004). Another double-blind placebo-controlled study focused on the effectiveness
of the anticonvulsant drug gabapentin in suppressing cannabis use and cannabis
withdrawal symptoms (Escher et al. 2005). In several studies gabapentin was found to
be effective and safe in treatment of depression, anxiety, insomnia, aggression, and
alcohol withdrawal. Twenty-one non treatment-seeking volunteers with concurrent
DSM IV8 cannabis and alcohol abuse or dependence were randomly treated with
gabapentin (1200 mg/d) or placebo. Gabapentin administration decreased a subset of
marijuana withdrawal symptoms compared to placebo as measured by the Marijuana
Withdrawal Checklist (MWC). Patients reported less sleep disturbance and enhanced
sleep quality. Gabapentin was also associated with diminished urge to use cannabis and
alcohol (Escher et al. 2005).
Quetiapine, an atypical antipsychotic medication, seems to decrease cravings for
cannabis in patients with co-occurred psychotic and substance use disorders (Potvin et
al. 2006). Nevertheless, these findings were only shown in an open label trial and a final
conclusion could only made after verification in a randomised, placebo-controlled trial
design. In summary, different agents, such as bupropion, divaleproex, naltrexone, and
nefazodone were investigated for the treatment of cannabis dependence and for the
prevention of cannabis reinstatement after abstinence, but each medication missing
broader effectiveness (Kleber 2003; UNODC 2002). Oral delta-9-tretrahydrocannabinol
(THC) might be helpful in suppressing cannabis withdrawal.
5.3 Psychosocial interventions for the treatment of drug dependency
A wide range of psychosocial interventions is available for the treatment of drug
dependence. As many different study designs were used to explore psychosocial
treatment, it is difficult to compare the individual direct outcomes. The optimal duration
of treatment might be a key point but has hardly been studied. The review of Gowing et
al. found limited strength of evidence that best outcomes are associated with treatment
duration of at least three months with at least weekly sessions (Gowing et al. 2001) The
intensity of treatment has been investigated in a few studies. Comparing a once-weekly
with a thrice-weekly counselling for buprenorphine-naloxone maintenance treatment,
Fiellin et al. did not find significant differences between the groups (Fiellin et al. 2006).
Highly structured relapse prevention seems to be more effective than less structured
interventions, with regard to cocaine users with co-morbid depression (UNODC 2002,
p.14). Treatment should match the patient and should be relevant to the individual
(Gowing et al. 2001). Some form of treatment may be more useful for women than for
men, others might be better for cocaine users than cannabis users (Haro et al. 2006), so
it is important to carefully choose and provide the optimal treatment setting for the
individual.
Often different approaches and methods are combined or compared. Combining
different treatment approaches can lead to improved results. One small American study
compared motivational enhancement plus CBT plus vouchers with motivational
enhancement only or with CBT. The latter two groups showed on average 7 days of
abstinence in the month prior to the last measurement, the three-way group had 13 days
on average (Rigter et al. 2004).
In general, treatment outcomes may differ if treatment is coerced: one study on
methamphetamine users compared those with legal and/or other agencies’ treatment
referrals to those who entered treatment voluntarily. Treatment outcomes did not differ;
however, those with legal pressure had more relapses within 6 months (Brecht et al.
2005).
One study on adolescent cannabis users (12-18 years) with 600 participants compared
five different interventions: Motivational enhancement followed by a short CBT for 6
weeks, 8-10 additional CBT sessions on top of the motivational enhancement and short
CBT for 12 weeks, family support network additionally to the extensive CBT,
Adolescent Community Reinforcement Approach (ACRA) and multidimensional family
therapy. (Dennis et al. 2004). All of these interventions reduced the number of problems
connected with cannabis use and the number of days of use was reduced. There was no
difference between the more intensive and less intensive interventions. A critical point
of this study mentioned by Rigter et al. (2004) is the fact, that not all the users were
dependent and did not seek help themselves but were referred to, as cannabis use in the
USA is considered more of a problem than in Europe (Rigter et al. 2004, 46).
Psychosocial treatment usually improves substitution maintenance treatment outcomes
for opiate dependent patients (Montoya et al. 2005).
Cognitive-Behavioural Therapy (CBT)
Cognitive-behavioural therapy as a structured psychosocial intervention aims at
modifying cognition, behaviour, beliefs. Usually some kind of skills training and
practice to deal with craving is involved, as well as monitoring high-risk situations for
relapse. There can also be the focus on relapse prevention, by training the drug users to
develop skills on avoiding high-risk situations and to cope with such situations. Some
kind of cognitive-behavioural interventions are used in many therapy settings in Europe.
They might be modified and used in different approaches.
CBT is of the most common and best evaluated methods for treating cocaine
dependence in the USA (UNODC 2002). CBT also seems to have long-term effects
with respect to decrease of cocaine use after leaving treatment (Kleber et al. 2006).
Compared with no treatment in the control group, CBT showed better outcomes
(UNODC 2002). CBT appears to be especially effective in patients with more severe
dependence or co-morbid mental illness (Kleber et al. 2006). CBT seems to be more
effective on long-term abstinence than most others psychosocial interventions (Gowing
et al. 2001). CBT shows some usefulness, especially for moderation of use, but research
outcomes are inconclusive (Rigter et al. 2004). Homework compliance within the CBT
programme for cocaine dependence was significantly linked with better retention and
reduction of use, also in quantity and quality of coping skills (Carroll et al. 2005;
Gonzalez et al. 2006). Four RCTs compared CBT with the twelve steps or similar
programmes and considered CBT superior especially concerning moderation of use
(Rigter et al. 2004). In one Australian study on CBT with amphetamine users, the
authors reported improvements in somatic symptoms, anxiety, and depression and in
amphetamine refusal self-efficacy (Feeney et al. 2006). Concerning the intensity of
CBT one trial found that the number of treatment sessions had a significant effect on the
level of depression, and also abstinence rates were better in those attending at least
twice (Baker et al. 2005). CBT has greater benefits than less intensive approaches under
controlled conditions (Kleber et al. 2006), and seems to be at least as effective as
manual-guided disease-model approaches. Another RCT on cannabis compared 14 CBT
sessions with two sessions of motivational enhancement and had a control group with
no treatment. After four months the two treatment groups had better outcomes than the
control group concerning moderation of use and symptoms of dependency. Also after
16 months the two treatment groups were equally effective with 25% being abstinent
(Kleber et al. 2006; Rigter et al. 2004). In order to increase treatment adherence in
heroin dependent patients in naltrexone treatment a behavioural naltrexone therapy was
conducted in one RCT. It was more successful than a control group in standard
treatment, but still had substantial drop-out and rather poor retention at 6 months
(Nunes et al. 2006). Other variables like crime, health and social functioning did not
differ between the treatment and control group, reduction in amphetamine use was
found in both groups (Baker et al. 2005).
One RCT on substance use disorders with psychotic disorders compared standard
treatment with MI/CBT intervention for psychotic patients with alcohol, cannabis
and/or amphetamine problematic use (Baker et al., 2006). There were no differences in
substance use at 12-month except for a small one in amphetamine use, but there was a
short-term improvement in depression and also in cannabis use and effects on general
functioning for the MI/CBT group (Baker et al. 2006). According to one study among
mostly homeless and mentally disordered crack smokers, CBT had better outcomes than
a 12-step programme and CA participation, but overall there was a high dropout rate
(UNODC 2002).
One special form of behavioural treatment especially for those with severe mental comorbidity
was studied in a randomised trial on drug dependent (cocaine, heroin or
cannabis) and mentally ill patients. The Behavioural Treatment for Substance Abuse in
Severe and Persistent Mental Illness (BTSAS) was compared with Supportive
Treatment for Addiction Recovery (STAR) as a control condition; both were conducted
twice a week for six months. The BTSAS programme was significantly more effective
in clean urine samples, attendance, treatment retention rate and attendance at sessions
(Bellack et al. 2006).
One RCT investigated the so-called Matrix Model, a manualised behavioural approach,
in the treatment of methamphetamine dependence, and found it to be efficacious
although over time the effects did not differ anymore from the control group (Rawson et
al. 2004).
Brief skills interventions led to shorter and less severe relapses than “attention placebo”,
both conditions having been combined with 12-step-principles and social learning
principles (UNODC 2002).
A comparison between CBT and interpersonal psychotherapy showed that CBT had
more treatment completers and longer abstinence after treatment (UNODC 2002), these
results being especially significant with severe cocaine users (UNODC 2002).
A manual-guided spiritual self scheme therapy, a form of behavioural treatment, was
studied in a stage I study for drug dependence. This integrates a cognitive model of self
with a Buddhist framework suitable for all faith backgrounds (Avants et al. 2005).
There was evidence for a shift in self-scheme, and this shift (from ‘addict self’ to
‘spiritual self’) was correlated with change in drug use (Avants et al. 2005).
In summary, CBT has especially good outcomes in the long-term view and for different
patient groups and especially for those with more severe dependence symptoms or comorbid
mental illness. It has been conducted for cocaine dependence in a number of
studies with good results, and also for other substances.
Motivational Interviewing (MI)
This intervention is based on cognitive-behavioural principles and was developed by
Miller and Rollnick (1991). MI does focus on enhancing motivation to change
problematic behaviour and uses methods like developing a feeling for discrepancies,
expressing empathy, support self-efficacy. It is often used as a brief intervention.
In substance-unspecific treatment “motivational enhancement“ has been examined in a
number of research studies. In general good results were found with respect to
reinforcing the willingness to undergo and continue interventions (Carroll et al. 2006).
Motivational enhancement has especially good outcomes for patients with lower initial
motivation than for those with higher initial motivation (Rohsenow et al. 2004). Also
for cannabis use positive results for MI have been found, i.e. greater reduction in use
and use-related problems (UNODC 2002).
A controlled study from Australia on heroin users in methadone maintenance treatment
showed Motivational Interviewing to lead to less drug use, later relapse, longer stay in
treatment (UNODC 2002). A US “Marijuana Treatment Project” compared two groups:
The first had two motivational enhancement sessions, the second had nine sessions
consisting of motivational enhancement, CBT and case management. A control group
consisted of a no treatment group: those on the waiting lists. Both treatment groups
reduced the days of use, and nine sessions had better results than two sessions. Also the
number of symptoms of cannabis dependence and the number of problems with
cannabis were reduced, but the second group did not do better regarding coping-skills as
it was expected (Litt et al. 2005).
A brief motivational intervention for cocaine and heroin users tested abstinence at 3-
and 6-month follow-up, and found better results for the treatment group, for both
cocaine and heroin use (Bernstein et al. 2005). A brief MI intervention for young
methamphetamine dependent patients was more successful than the psychoeducation
control group although MA use decreased in both groups only on the short-term scale
(Srisurapanont et al. 2007). A multi-site study with 450 cannabis-dependent patients
compared a delayed treatment control with a two-session motivational approach and
with a nine-session combined motivational and coping skills approach. The two latter
interventions had greater reductions in cannabis use than the delayed treatment, both at
4 month and 15 month follow-up (Kleber et al. 2006, 159). The combination of brief MI
intervention with psycho-physiological personalised feedback was effective in one pilot
RCT (Stotts et al. 2007). As a low-threshold intervention in a group setting it can be
helpful to start and maintain participation in treatment, especially for patients with more
severe dependence (Rosenblum et al. 2005). Also for special subgroups like co-morbid
patients MI showed effectiveness. A two-session MI and the control group with
standard psychiatric interview for co-morbid patients (psychosis and drug use disorders)
did find improved treatment outcomes for both groups; differences were significant
when looking at different kind of drugs used: for cocaine users the MI intervention had
better treatment outcomes, but for the cannabis users the SI (standard psychiatric
interview) group had better outcomes (Martino et al. 2006).
Community Reinforcement Approach (CRA)
The Community Reinforcement Approach (CRA) uses a range of methods and is based
mainly on cognitive-behavioural principles. Its concept includes that environmental
contingencies (like family, peers, work, leisure time involvement) can play a helpful
role in encouraging or discouraging drug use. CRA is often combined with Contingency
Management or similar incentive programmes.
A meta-analysis on CRA found strong evidence that CRA with incentives is more
effective than usual care or CRA without incentives for the treatment of cocaine
dependence. The same found limited evidence that CRA with incentives is more
effective in an opioid detoxification programme and more effective than a methadone
maintenance programme (Centre for Reviews and Dissemination 2007b). One RCT
compared the impact of different values of the vouchers during a CRA treatment; the
high-value group (maximal value $1995/12 weeks) had greater and longer abstinence
than the low-value group (maximal $499/12 weeks), but this relationship weakened
over time (Higgins et al. 2007).
First reports on CRAFT (CRA Family Training) are promising for drug users in general,
without substance-specific effects (Rigter et al. 2004). One study on Adolescent
Community Reinforcement Approach (ACRA) compared the intervention as an
aftercare programme with normal aftercare, and found reduced days of use and a higher
rate of abstinence after one year in the ACRA group (Rigter et al. 2004).
One study compared CBT, rewards, and the combination of both, where all three
seemed to be successful in reducing the use, but without significant differences (Rigter
et al. 2004).
Some studies compared CRA with standard drug counselling with referral to AA,
randomised and controlled, and found better outcomes regarding abstinence, duration of
abstinence, personal functioning improvements and staying in treatment, finding that
the different components of the CRA contribute to the overall outcomes (UNODC
2002).
Contingency management (CM)
Contingency management is another form of behavioural approach. The principle of
this approach is that “rewards” are given to those who have negative urine samples to
reinforce abstinent behaviour. Those incentives can be implemented in the form of
vouchers or prizes, and also privileges in the treatment setting. CM is usually embedded
in a treatment like CRA or structured drug counselling. As Contingency Management is
hardly conducted in Europe, research on the effectiveness comes almost exclusively
from the USA. CM was found to be effective in reducing drug use and treatment
retention, but these results tend to be short-term only.
A meta-analysis found CM to be effective in reducing drug use in methadone treatment
(Centre for Reviews and Dissemination 2007a), but not all research found positive
outcomes of voucher-based interventions (Gowing et al. 2001). It has been found to be
effective in a number of studies, in different samples and settings: cocaine users in
methadone maintenance, pregnant women, homeless people, freebase using people
(Kleber et al. 2006).
The motivation to change substance use was studied in one randomised trial, where
patients were randomised to either standard treatment or standard treatment plus CM,
and motivation was measured with the stages of change model URICA 3 months later.
The CM group had longer duration of abstinence, but the groups did not differ
concerning their motivation to change substance use (Ledgerwood et al. 2006).
Apart from longer duration of abstinence CM also seems to improve Quality of life,
measured with the Quality of Life Inventory (QOLI) in cocaine users (Petry et al. 2007).
For methamphetamine users CM also had good results (Roll, Petry et al. 2006).
Contingency reinforcement therapy showed promising results in abstinent cocaine
users; compared to interpersonal problem-solving a treatment package combined with
voucher payments had better outcomes in the one study, when vouchers were delivered
immediately after negative urine samples, than in a second study where vouchers were
delivered weekly with a small value in the beginning (UNODC 2002). In the first study,
half of the respondents completed treatment and achieved one-month abstinence in their
cocaine use, whereas in the second study nobody achieved this goal (UNODC, 2002).
Reinforcement treatment is more successful when the reinforcements have increasing
magnitude for consecutive abstinence and reset after positive urinalysis (Roll et al.
2006). In order to link opioid dependent patients from hospital treatment to further drug
treatment vouchers for free methadone were compared with case management. Both
interventions had higher percentage of enrolled patients at three months and at six
months, and are therefore more helpful than standard treatment in linking drug
dependents to treatment system (Sorensen et al. 2005).
The effects of CM have been investigated for methadone maintenance patients in a
number of studies. CM attendance resulted in longer periods of abstinence than a
performance feedback control group, but this difference disappeared at the end of the
24-weeks intervention (Schottenfeld et al. 2005). CM condition in connection with
standard outpatient treatment resulted in more and longer abstinence among cocaine and
amphetamine users, and also retention was better than in the control group (Petry et al.
2005). Concerning the possible amount of prizes, for more severe dependent patients
the outcomes on abstinence were magnitude-dependent, whereas with those patients
who started treatment already with negative urine samples, the level of prizes did not
effect abstinence during treatment and was here the same a in the control group (Petry et
al. 2004). Combined with group therapy in methadone clinic, the prize-based CM
patients had more cocaine-negative urine samples and attended more group sessions
than the control group with standard treatment (Petry et al. 2005). Brief voucher-based
reinforcement for cocaine users in a methadone maintenance patient sample was
effective in the short-term (Sigmon et al. 2004). On the other hand, a long-term
reinforcement for cocaine use in methadone patients was investigated as well in a 52-
weeks intervention, and vouchers were highly effective in decreasing cocaine use
(Silverman et al. 2004).
CM showed better treatment retention and drug-free urine in cannabis users and even
more so in combination with Motivational Enhancement and CBT, while CBT in
combination with Motivational Enhancement (MET) had continued reduction in use
through a six-month follow-up (Carroll et al. 2006).
Directly compared with CBT, CM treatment resulted in better retention rates and lower
stimulant use during treatment whereas CBT had longer-term outcomes, and no additive
effect for the combination of both interventions was found (Rawson et al. 2006). This
was shown as well for cocaine using methadone patients (Rowan-Szal et al. 2005). For
homeless cocaine users in a shelter a CM intervention was effective on reducing cocaine
use (Tracy et al. 2007). A clinical trial on adult cannabis dependent persons found
vouchers to maintain abstinence during treatment, whereas CBT enhanced the posttreatment
abstinence maintenance (Budney et al. 2006).
A comparison of contingent voucher treatment with a motivated stepped care (MSC)
found similar outcome on negative urine samples for both groups, both significantly
higher than Standard Care, and a still higher proportion for the combined therapy of
vouchers and MSC. Regarding retention the voucher group was superior while the
stepped-based care had better adherence to counselling sessions (Brooner et al. 2007).
Different approaches and deliveries of contingencies are compared in a number of
studies. The effectiveness of prize-based incentives in stimulant dependent patients was
studied, and different treatment histories and experiences were taken into account. The
effectiveness of incentives did not differ between the experienced and inexperienced
patients (Killeen et al. 2007). Alessi et al. conducted a two-phase crossover design study
on prize-based contingency management, where standard treatment was compared with
CM condition, which consisted of a 12-week standard treatment plus the possibility of
winning prizes for negative urine samples and treatment attendance (Alessi et al. 2007).
Outcome was measured in weeks retained in treatment and duration of abstinence (at 6
and 9 month follow-up). Weeks retained did not differ between groups but the longest
duration of sustained abstinence (LDA) was significantly higher in the CM condition
(Alessi et al. 2007). Another form of CM is to reinforce goal-related activities instead of
reinforcing abstinence by negative urinalysis, but the latter group had better outcomes
(Petry et al. 2006). On the other hand both vouchers and prizes as a contingent treatment
have similar outcomes on treatment (Petry et al. 2005).
Also housing has been used as contingencies for homeless substance users: An intensive
behavioural treatment for homeless cocaine-dependent people with three groups:
treatment only, treatment plus housing for six months and treatment plus housing as a
contingency for drug abstinence. The two housing groups had better outcomes
concerning stable housing and employment (Kertesz et al. 2007). Another study on
contingent housing and work also found more abstinent patients who also stayed
abstinent for a longer time and had fewer relapses than the control group (Milby et al.
2004).
A comparison between voucher and buprenorphine contingency and standard treatment
without contingencies for heroin-dependent patients with cocaine use showed no
difference in the retention rate between the groups, but the buprenorphine group had
more weeks of continued abstinence from heroin and cocaine (Gross et al. 2006).
Another study found that combining CM with bupropion had better outcome on cocaine
use in methadone patients than bupropion alone (Poling et al. 2006).
Guidelines for voucher purchases did not seem to be a critical aspect of voucher
programmes, as no differences in the kind of purchases were found (Pantalon, et al.
2004).
Those patients who participate in family activities during their CM treatment remained
longer in treatment, were abstinent for more weeks and reported greater reduction in
family conflicts than those who did not participate in family activities (Lewis et al.
2005).
Concerning cocaine users with schizophrenia in a small-scale study CM reduced
cocaine use in all three individuals (Roll et al. 2004).
Cue exposure therapy (CET)
Cue exposure is based on learning theory principles. It consists of repeated exposure to
stimuli or cues associated with drug use (e.g. sight of o syringe for intravenous drug
users) and aims at controlling or changing responses to these cues. Until now this
intervention has been mainly done in laboratory conditions.
Aversion therapy works with cues, and one experimental controlled comparative study
on crack cocaine craving compared three different aversion therapies: chemical, covert
sensitization and faradic; results indicate the usefulness of aversion therapy in order to
reduce craving (Bordnick et al. 2004).
Psychodynamic and interpersonal therapies
Psychodynamic interventions originate in the psychoanalytical approach and work on
unconscious conflicts, relationships and problematic situation. The therapist-patient
interaction and relationship is an important feature in this approach. Other Interpersonal
therapies focus on interpersonal relationships and issues as well, and aim at resolving
interpersonal problems.
No RCTs have been conducted for treatment using psychodynamic or interpersonal
therapy, but a case series on individual psychodynamic psychotherapy and some reports
on group psychodynamic therapy showed some efficacy. One clinical study on the
comparison between interpersonal psychotherapy (IPT) and CBT found CBT to be
superior (Kleber et al. 2006). Supportive-expressive therapy, a type of psychodynamic
therapy, was one of four interventions studied in the NIDA collaborative cocaine
treatment study, but seemed to be less effective than individual plus group drug
counselling in decreasing cocaine use (Kleber et al. 2006).
A comparison of Relational Psychotherapy Mothers’ Group (RPMG) with Recovery
Training for substance dependent mothers in a methadone clinic found better outcomes
for the first group concerning child maltreatment, cocaine use, and greater improvement
for the children of those mothers. But at six months follow-up these differences between
the two groups were not present any longer (Luthar et al. 2007).
A Dual Focus Schema Therapy (DFST) was conducted for personality disordered
opioid dependent persons in methadone maintenance treatment. Compared to the 12-
step control group the treatment group had more rapid decreases in the frequency of use,
on the other hand the control group had better reductions of disphoric affect. There were
no group differences for retention, utilisation, reduction in psychiatric symptoms and
other severity indicators (Ball 2007).
Ketamine-assisted psychotherapy was tested as a single-session intervention and as a
three-session intervention for heroin dependence and showed a higher rate of abstinence
for the second group while both groups had better outcomes than the control group with
standard treatment (Krupitsky et al. 2007).
Counselling
Counselling can be defined as a client-centred intervention to help the individual to
overcome problems (EMCDDA 2007). In the US standard treatment is often based on
the 12-step principle, both for individual and group counselling. However, in Europe
counselling is not necessarily based on the 12-step principle.
One study found less frequent cocaine use after regular abstinence-oriented counselling
(UNODC 2002), another study compared intensive counselling in a structured day
programme with four-weeks inpatient treatment of cocaine users, and found
improvements for both groups (UNODC 2002). For the treatment of cannabis
dependence counselling approaches seem to be beneficial according to a Cochrane
systematic Review, as well as CBT and CM approaches, yet with low abstinence rates
for all of them, so the overall conclusion of this review is inconclusive and highlights
the fact that treatment of cannabis dependence seems difficult (Denis et al. 2007).
An Australian RCT studied the effect of a postnatal home visit programme for drugusing
(heroin, amphetamine, cannabis, benzodiazepines) mothers. Concerning drug use
there was no difference between the treatment group and the control group (no visits),
both reduced the drug use during pregnancy but drug use increased again by six-month
post-partum (Bartu et al. 2006).
A brief counselling approach – Medical Management – was conducted as a preliminary
study in methadone maintenance treatment and showed effects on drug use, as well as
drug counselling (Pantalon et al. 2004).
A further study showed that the frequency of attendance is positively related to lower
risk of relapse in a six-month follow-up (UNODC 2002). Telephone-based continuing
care following outpatient treatment for cocaine and/or alcohol users produced the same
abstinence-related outcomes than the control groups with either face-to-face relapse
prevention or standard 12-step group counselling (McKay et al. 2004), but seemed to be
somehow effective as an step-down treatment for most patients (McKay et al. 2005).
The effect of either 12-step facilitation or Acceptance and Commitment Therapy (a
behavioural oriented, spiritual approach) was investigated for patients in methadone
maintenance treatment and compared to no psychosocial treatment in addition to the
methadone treatment. Both conditions had better outcome than the methadone only
control group concerning drug use (Hayes et al. 2004).
Group counselling
One large study by the NIDA on cocaine dependence compared four treatment settings:
group counselling alone, group counselling with individual counselling, group
counselling with cognitive psychotherapy, group counselling with supportive expressive
psychotherapy (UNODC 2002). Concerning reductions of use, the group and individual
counselling together was the most successful while the other three groups were similar
in outcome (UNODC 2002). One RCT on a manualised group intervention for comorbid
(psychosis) drug users found substance reduction in the treatment condition
(James et al. 2004).
Also professional treatment uses 12-step principles in group and individual drug
counselling. Intensive sessions (36 individual and 24 group sessions over 24 weeks)
have shown significant effects in reducing cocaine use, the greatest effects for 12-step
based individual drug counselling plus group drug counselling, compared to supportiveexpressive
therapy, cognitive therapy and drug counselling alone (Kleber et al. 2006).
12-step-oriented standard group counselling seems to be similarly effective than relapse
prevention aftercare (Kleber et al. 2006). One study of mild cannabis dependence
among adolescents focused on a manual-guided, group-based treatment and found
reduced use at 6 months and also sustained at 12 months (Kleber et al. 2006).
Twelve-step and other self-help
The 12-step approach is based on the principles of Alcohol Anonymous and has been
adapted for other groups as well. 12-step interventions are one of the most common
approaches in the USA and also rather common in Europe in different. Participation in
12-step oriented self-help groups seems to reduce cocaine use, the higher the frequency
of participation, the greater the effect (Kleber et al. 2006). Also active participation in
self-help groups predicted less cocaine use and seems more important than attendance
alone (Weiss et al. 2005). TSF (twelve-step fellowship) showed significantly greater
effects in alcohol and cocaine users than clinical management for reducing cocaine use,
comparable to the effects of CBT (Kleber et al. 2006). A post-treatment participation in
12-step self-help had better outcome in a group of cocaine- or alcohol-dependent
patients in a day hospital rehabilitation programme (UNODC 2002).
Therapeutic Communities (TC) and other inpatient treatment
Therapeutic communities (TC) have an inpatient treatment approach originated in the
USA. They are based on democratic and de-institutionalised principles and aim at
abstinence, often also at smoking cessation. A Cochrane systematic review on
therapeutic communities included seven RCT’s. There is only limited evidence that TC
is significantly superior to other inpatient treatment; compared to community residence
no differences were found concerning treatment completion, compared to day TC the
residential group was significantly better in attrition and abstinence rates, and two of the
RCTs investigated TCs in prison (see WP 4) (Smith et al. 2007).
Other group and family therapies
A rather special form of treatment has been tried in a small initial randomised pilot
study: Mindfulness meditation plus standard treatment was compared with standard
treatment only on substance-abusing patients (Alterman et al. 2004). There were no
differences found in urine results or psychological health, but the ASI composite scores
indicated greater improvement in medical problems for the meditation group (Alterman
et al. 2004). One preliminary study on spiritually-focused group therapy plus
acupuncture found longer abstinence from heroin and cocaine than in the acupuncture
only group (Margolin et al. 2005).
The JEWEL project (Jewellery Education for Women Empowering their Lives) was an
economic empowerment and HIV prevention intervention for illicit drug using women
with prostitution involvement. Compared to pre-treatment there were reductions in daily
drug use and number of sex partners (Sherman et al. 2006).
One study found better outcomes regarding cocaine use for an aftercare programme
with a combination of group therapy and structured relapse prevention than for group
therapy alone (after intensive outpatient treatment for both groups) (UNODC 2002).
5.4 Evidence from Europe
Pharmacological treatment agents for opioid-related disorders
Pharmacotherapy of opioid withdrawal/detoxification
Various Cochrane reviews on detoxification indicate that the most extensively tested
effective strategy for the detoxification of heroin dependent patients is replacement of
the illicit short-acting opioid by the long-acting opioid-agonist methadone, which is
subsequently tapered and finally discontinued (Amato et al. 2005). The process and
outcome of long-acting opioid-agonist tapering may be improved through additional
prescription of a calcium channel blocker such as nimodipine (Jimenez-Lerma et al.
2002), whereas additional prescription of amantadine (antiviral drug also used as an
antiparkinsonic) does not seem to improve the effectiveness of methadone tapering in
heroin dependent patients with or without a co-morbid cocaine dependency (Perez de
los Cobos et al. 2001).
Methadone as a detoxification agent (including methadone reduction treatment)
Methadone the most commonly used opiate agonist for detoxification treatment in
Europe, mainly carried out in a linear reduction schedule with equal dose decreases.
Reducing doses of methadone is currently accepted as a standard detoxification
approach and despite the low retention rate, most patients in Europe are treated in an
outpatient treatment setting (Gossop 2006). Methadone has been described as the most
effective pharmacotherapeutic agent currently used in detoxification (Kreek 2000).
Nevertheless, various patients relapse to heroin use and in comparison to methadone
maintenance treatment, methadone withdrawal treatment leads to high drop-out rates,
even though the effect on the proportion of positive urine samples in both treatment
modalities remains high (Amato et al. 2007; Simoens et al. 2000). Methadone reduction
treatment, as a special form of long-term methadone detoxification treatment, has
similarities with gradual methadone treatment (Gossop 2006). Likewise the results are
analogical to those of methadone maintenance programmes. As only two thirds of the
patients in methadone reduction treatment received the planned reducing doses,
methadone reduction treatment is frequently not delivered as intended (Gossop 2006).
Even if methadone reduction treatment is delivered as intended, the outcomes remain
poor especially in comparison to methadone maintenance treatment in terms of
reduction of illicit opioid use and criminal behaviour (Gossop 2006). Higher doses of
methadone (60 mg) for non-rapid detoxification were found to be more effective than
lower doses (20 mg) with regard to treatment retention (Berglund et al. 2003). Also
fixed methadone detoxification programmes may lead to higher retention rates than
flexible methadone detoxification schedules, maybe because of reduced mean doses in
the flexible regime group (Simoens et al. 2000). However, another European report
found no differences between fixed and flexible reduced mean doses (Gossop 2006).
Patients who are informed about the methadone withdrawal schedule have better
outcomes than uninformed patients, although patients do not have better outcomes,
when they control their methadone schedule on their own (Rigter et al. 2004).
Compared to other opioid agonists, methadone showed better outcomes in terms of
completion rate and less severe withdrawal symptoms (Amato et al. 2004). Different
European effectiveness reports demonstrated that the potential of methadone to alleviate
withdrawal symptoms is equal to α2-adrenergic agonists, like clonidine or lofexidine
(Berglund et al. 2003; Rigter et al. 2004). Nevertheless, due to several important
limitations, these recent findings should be interpreted with caution and the most recent
Cochrane review found no statistically significant differences between methadone and
adrenergic agonists (Amato et al. 2005). Furthermore, an analysis of single studies in
this systematic review showed that methadone detoxified patients experience fewer side
effects and withdrawal symptoms than patients treated with adrenergic agonists. In
particular, early withdrawal symptoms were more adequately controlled with
methadone than with lofexidine (Amato et al. 2005). These results correlate with former
suggestions that methadone treatment is more effective than α2-adrenergic agonists in
terms of treatment retention and relapse rate and provide a better safety profile (Amato
et al. 2004). One European effectiveness report suggested that the combination of
methadone and nimodipine, a dihydropyridine calcium channel blocker, could improve
treatment outcomes, but no recent clinical trial could confirm these findings (Rigter et
al. 2004).
In summary, European evidence showed that detoxification treatment using tapered
doses9 of methadone is associated with adequate rates of completion of withdrawal,
reduction of withdrawal symptoms to tolerable levels, and minimal adverse effects.
Control by the clinician rather than the patient of the rate of reduction of the methadone
dose is associated with greater reductions in methadone doses. Compared to the effects
of methadone in maintenance treatment, the efficacy of methadone for detoxification
treatment is limited. The attrition rate of methadone detoxification treatment remains
high, particularly in an outpatient setting compared to an inpatient setting. Despite the
findings related to methadone and α2-adrenergic agonists of one recent RCT, the current
systematic Cochrane review shows that methadone had better outcomes than other
opioid agonists in terms of completion rate, and patients have shown less severe
withdrawal symptoms. A Cochrane review found psychosocial treatment offered in
addition to any pharmacological detoxification programme to be effective in terms of
completion of treatment, results at follow-up and compliance (Amato et al. 2004).
Buprenorphine as a detoxification agent
The partial μ-agonist and κ-antagonist buprenorphine is a commonly used agent for the
detoxification treatment of opiate dependents in Europe. Like methadone, the
detoxification treatment with buprenorphine is carried out in a linear reduction schedule
with equal dose decreases.
Under the provision of equal doses, the efficacy of buprenorphine in the detoxification
of opioid dependents is comparable to methadone with regard to treatment retention,
illicit drug use, and suppression of withdrawal symptoms (Rigter et al. 2004). Gossop et
al. suggested that detoxification with buprenorphine has less severe withdrawal
symptoms in comparison to methadone detoxification and may lead to a higher number
of completed detoxification treatments (Gossop 2006). Nevertheless, Kornor et al.
(Kornor et al. 2006) recommend that outpatient buprenorphine tapering should be
closely monitored due to the substantial psychological distress and increased death risk.
Like methadone the efficacy of buprenorphine for detoxification treatment depends on
the treatment setting; the relative efficacy of outpatient and inpatient withdrawal
remains somewhat unclear (Lingford-Hughes et al. 2004). The Trimbos effectiveness
report found buprenorphine to be less effective in outpatient than in inpatient setting,
but with better retention rates than methadone in outpatient setting (Rigter et al. 2004).
The efficacy of buprenorphine for detoxification treatment depends on the dosage; low
doses of buprenorphine were found to be effective in attenuating withdrawal symptoms
with acceptable rates of treatment retention, despite additional medication for nonspecific
symptoms such as anxiety and insomnia (Fuscone et al. 2005). The additional
application of carbamazepine, an anticonvulsant and mood stabilising drug in the
treatment of epilepsy and bipolar disorders, seems to improve the clinical outcomes of
buprenorphine assisted detoxification in opiate dependents with additional multiple drug
abuse (Seifert et al. 2005). Patients treated with buprenorphine and carbamazepine
showed better outcomes in psychological status and a more effective short-term relief of
affective disturbances than patients treated with methadone and carbamazepine.
However, only 26 patients were included in this clinical trial so further studies are
needed to confirm these findings. Compared to the α2-adrenergic agonist clonidine and
methadone, buprenorphine has fewer cardiac side effects (Gossop 2006; Rigter et al.
2004). Additional behavioural treatment added to detoxification treatment with
buprenorphine (and voucher incentive programme and community reinforcement
approach) leads to better outcomes on the measure duration of abstinence than in
standard methadone detoxification treatment (Simoens et al. 2000).
α2-adrenergic agonists as detoxification agents
The use of α2 adrenergic agonists (clonidine, lofexidine) to manage the acute phase of
opioid withdrawal is common Europe. However, most studies on the effectiveness of
clonidine and lofexidine were done outside of Europe and shown, that clonidine and
lofexidine could be considered as an effective detoxification option especially for
patients, who prefer non-opioid treatment for detoxification. A recent European RCT
found that patients randomised to lofexidine + naloxone had longer periods of
abstinence before relapse than those who received methadone (McCambridge et al.
2007). Furthermore, patients treated with lofexidine were more likely to complete
detoxification, and more likely to be abstinent from opiates after 5 months, than those
who detoxified with methadone. These findings were found to be consistent with the
results of former studies reporting a more rapid resolution of withdrawal symptoms
after lofexidine compared to methadone detoxification (McCambridge et al. 2007). This
makes lofexidine particularly suitable in a prison context when methadone prescription
is not possible (Howells et al. 2002). Lofexidine provided like clonidine the benefit that
detoxification and naltrexone induction can be achieved within 5 days and without risk
of opiate diversion. Raistrick et al. (2005) used an open-label randomised controlled
trial design to examine the equal clinical effectiveness of buprenorphine and lofexidine
in a community opiate detoxification. Two hundred and ten patients were randomised
either to buprenorphine or lofexidine detoxification treatment in a specialist out-patient
clinic according to a predefined protocol. 46% of the patients treated with lofexidine
and 65% treated with buprenorphine completed the detoxification programme. A 7-day
buprenorphine detoxification showed to have some benefit in comparison to 5-day
lofexidine detoxification with regard to the severity of withdrawal (Raistrick et al.
2005). The additional provision of symptomatic medications enhanced the effectiveness
of adrenergic agonists, and especially the combination with opioid antagonists such as
naltrexone and naloxone leads to less severe withdrawal symptoms in detoxification
compared to the treatment with lofexidine alone (Buntwal et al. 2000).
In summary and taking into account the evidence from outside of Europe, clonidine and
lofexidine could be considered as an effective detoxification option especially for
patients, who prefer non-opioid treatment for detoxification. Compared to tapering
doses of methadone, opioid withdrawal management with α2-adrenergic agonists like
clonidine and lofexidine leads to equal rates of completion of withdrawal and overall
severity of withdrawal, but to more side effects and therefore to higher drop-out rates
especially at an earlier stage of treatment. Lofexidine showed fewer side effects with
similar clinical effectiveness in comparison to clonidine. The most described adverse
effect of the opioid withdrawal treatment with clonidine is hypotension, which leads to
the recommendation to check patients` blood pressure regularly. Due to the hypotensive
side effects of clonidine, lofexidine should be preferred in outpatient settings.
Buprenorphine-naloxone combination as a detoxification agent
In Europe, the combination of buprenorphine and naloxone is available for the
maintenance and detoxification treatment of opioid dependence. However, European
studies on the effectiveness of this combination are only available from outside of
Europe and shown in the respective chapter. The intention of adding naloxone to
buprenorphine is to deter intravenous misuse and reduce the symptoms of opiate
dependence and the evidence of effectiveness shows that the combination of
buprenorphine and naloxone is effective and safe for the detoxification of opioid
dependents and well tolerated by patients.
Codeine/dihydrocodeine as a detoxification agent
The analgesic agent dihydrocodeine is available as tablet, oral solution or injection. A
recent open label randomised controlled trial compared buprenorphine with
dihydrocodeine for detoxification from illicit opiates in primary care10 (Wright et al.
2007). Sixty illicit opiate using participants were randomly treated either with daily
sublingual buprenorphine or daily oral dihydrocodeine, both under a standard regimen
including reduction of not more than 15 days. Abstinence was indicated by a urine
sample and the secondary outcomes were recorded during the detoxification period and
three and six months after detoxification. The attrition rate was high: Only 23% of the
participants stayed in the prescribed course of detoxification medication and provided a
urine sample at the final prescription. Risk of non-completion of detoxification was
higher in the administration of dihydrocodeine, and a lower proportion of people
allocated to dihydrocodeine provided a clean urine sample compared with those who
received buprenorphine (3% vs. 21%). Furthermore, the participants allocated to
dihydrocodeine were more likely to call on professional carers during detoxification and
more participants allocated to buprenorphine were abstinent at three months and six
months post detoxification. In summary, the included European study provides only
little evidence to support dihydrocodeine as a first line agent for opiate detoxification.
Compared to buprenorphine, dihydrocodeine leads to higher drop-out rates and to a
lower rate of opiate free urine samples.
Pharmacotherapy for opioid maintenance
Opioid-assisted maintenance programs are among the most important strategies in this
respect, as they are associated with reductions of heroin use and HIV risk behaviour.
Considering the high rate of relapse after detoxification of opioid dependence,
maintenance therapy is currently considered to be the first-line treatment for such
patients. Opioid-assisted maintenance programs have been introduced in most countries
of the world, yet the medication of choice differs from one country to the next.
Methadone is the most extensively studied and most widely used opioid in maintenance
treatment. Other μ-opiate agonists that are used include levo-acethylmethadol (LAAM),
codeine, slow-release oral morphine and diacetylmorphine, as well as the partial μ-
opioid agonist buprenorphine. In Europe several agents are approved for maintenance
treatment of opiate dependents (Table 6).
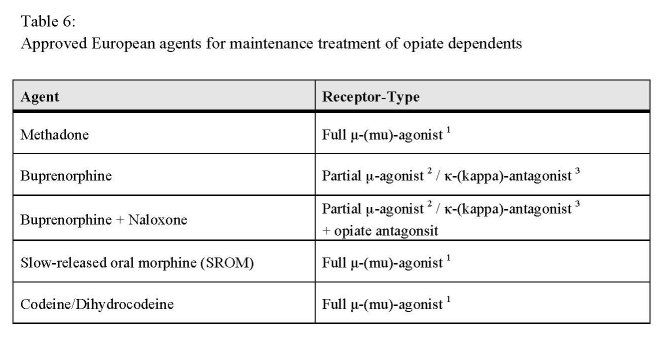
1 Full agonists have affinity for and activate a receptor, displaying full efficacy at that receptor
2 Partial agonists also bind and activate a given receptor, but have only partial efficacy at the receptor
3 A receptor antagonist is a drug that does not provoke a biological response itself upon binding to a
receptor, but blocks or attenuates agonist-mediated responses. Antagonists have an affinity but no
efficacy for their cognate receptors.
Methadone as a maintenance agent
The spectrum of efficacy is connected to the methadone dose and the treatment duration
(Berglund et al. 2003). For example, methadone dosages ranging from 60 to 100
mg/day were found to be more effective than lower dosages in terms of treatment
retention and reduction of heroin and cocaine use during treatment (Faggiano et al.
2003). A comparative meta-analysis indicated that high doses of methadone (≥ 50
mg/day) were more effective than low doses of methadone (< 50 mg/day) in reducing
illicit opiate use, that high doses of methadone were more effective than low doses of
buprenorphine (< 8 mg/day) and equally effective compared to high doses of
buprenorphine (≥ 8 mg/day) in terms of treatment retention and reduction of illicit
opiate use (Farre et al. 2002). Indeed, lower doses of methadone seem to be sufficient to
stabilise the patient and might be helpful to keep the patient in treatment, but are
inadequate to suppress opiate use (Simoens et al. 2000). Besides the better outcomes in
retention rates and prevention of illicit drug use, higher methadone doses lead also to an
improved physical and psychological situation for the patient and therefore to a better
quality of life (Rigter et al. 2004). European reports confirmed the dose-related retention
rate including better outcomes for patients with higher methadone doses (Simoens et al.
2000). In order to avoid overdose related deaths, it is recommended to initiate
methadone maintenance treatment with lower doses varying between 10 to 40 mg/day.
At the end of the treatment the dose should be in the range between 60 and 120 mg/day
to be effective (Rigter et al. 2004). Low dosage of methadone has been described to be
one of the main problems of methadone treatment also in other countries, such as Italy
(Schifano et al. 2006) and The Netherlands (Termorshuizen et al. 2005).
In summary, methadone is the best-studied and most effective opioid agonist for
maintenance treatment so far. Treatment outcome in methadone maintenance has been
shown to improve substantially with increased dosages of methadone: Higher doses are
associated with better treatment retention rates and lower rates of illicit opioid use.
Daily methadone doses of 60mg/day or more were found to be most effective in
methadone maintenance treatment (Berglund et al. 2003). Adequate dosing is an
important issue and avoids on the one hand unpleasant withdrawal symptoms,
especially in the latter half of each inter-dosing interval, and on the other hand
significant adverse effects.
Buprenorphine as a maintenance agent
Besides methadone, buprenorphine is the most used agent for the maintenance treatment
of opiate dependence in Europe. Due to its partial μ-opioid agonist properties,
buprenorphine has lower abuse potential and a lower risk for overdose compared to full
μ-agonists like methadone or LAAM (Berglund et al. 2003) and like methadone, the
efficacy of buprenorphine is dose-related. Kakko et al. found a considerably higher level
of treatment retention in patients treated with buprenorphine in a maintenance approach
compared to detoxification (Kakko et al. 2003). The longer duration of therapeutic
action of buprenorphine provides the advantage of a less than daily schedule.
Low and moderate doses (2 - 8 mg) of buprenorphine are superior to placebo in the
measures of treatment retention, provision of opioid-negative urine samples, mortality,
and psychological and social functioning (Rigter et al. 2004). Similar to methadone,
higher fixed doses of buprenorphine are more effective than lower doses with superior
levels of retention in treatment and opiate use (Berglund et al. 2003). However,
moderate doses of methadone (50-65 mg/day) were found to be slightly more effective
than moderate doses of buprenorphine (2-8 mg) (Simoens et al. 2000). High doses of
buprenorphine lead to equal retention rates as high doses of methadone, although
methadone seems to be more effective in reducing illicit opioid use (Rigter et al. 2004).
The longer duration of therapeutic action of buprenorphine provides the advantage of a
less than daily schedule. European effectiveness reports found similar effects in the
measure of treatment retention in thrice weekly administration compared to daily
administration (Rigter et al. 2004; Simoens et al. 2000).
The efficacy of buprenorphine maintenance treatment was found to be comparable to
methadone maintenance showing a reduction of opiate use and craving under
buprenorphine (Duburcq et al. 2000). Buprenorphine reduced the risk of overdose
related death compared to methadone (Gossop 2006; Simoens et al. 2000) and was
found to reduce mortality in maintenance treatment (Auriacombe et al. 2001).
Buprenorphine has further advantages for special groups of opioid dependents, like
pregnant women, indicated by a low level of withdrawal symptoms in newborns
(Simoens et al. 2000). Giacomuzzi et al. (2006) suggested that buprenorphine treatment
is as effective as methadone with respect to quality of life and physical symptoms
(Giacomuzzi et al. 2006). Another possible advantage of buprenorphine is the
antidepressant effect. The maximum effective dose of buprenorphine seems to be
limited to five days (Simoens et al. 2000) and a switch from methadone to
buprenorphine maintenance treatment seems to be possible, but more research on this
topic is needed (Rigter et al. 2004).
In general, maintenance treatment with buprenorphine provides some advantages for the
treatment of opioid dependence in comparison to methadone, e.g. a better safety profile
at high doses, a lower abuse potential, the possibility of a less-than-daily administration
and lower impairment in psychomotor and cognitive functioning. Similar to methadone,
the efficacy of buprenorphine in maintenance treatment is dose related.
Buprenorphine-naloxone combination as a maintenance agent
The Buprenorphine-naloxone combination contains the partial opiate agonist and
antagonist buprenorphine as well as the opioid antagonist naloxone to deter illicit
intravenous preparation of the tablet. This is intended to attenuate the effects of
buprenorphine on opioid-naive users should this formulation be injected. Kakko et al.
(2007) used a randomised controlled trial design to show that an adaptive,
buprenorphine/naloxone based stepped care strategy is equally effective than an optimal
methadone maintenance treatment (Kakko et al. 2007).
Heroin as a maintenance agent
Some clients do not benefit from maintenance treatment with methadone or
buprenorphine, which lead to the question of the effectiveness of heroin prescription,
especially for patients who dropped out of treatment or who continued illicit opioid use
while in treatment. Heroin (diacetylmorphine, diamorphine) is a semi-synthetic opioid
synthesized from morphine and acts on the endogenous μ-opioid receptors. So far, all
studies on the effectiveness of heroin as matenance agent were accomplished in Europe.
A first British randomised clinical trial comparing heroin (diamorphine) and methadone
found that the prescription of heroin is not clearly superior in comparison to methadone
(Gossop 2006). However, later clinical trials demonstrated the feasibility and clinical
effectiveness of heroin prescription, with better outcomes in patient recruitment,
treatment retention and treatment compliance (Gossop 2006; Rigter et al. 2004). Also
reduced delinquency and reduced illicit heroin and cocaine use were found, although the
uses of other drugs were less marked and the use of benzodiazepine declined slowly
(Gossop 2006). Some patients benefit form prescribed heroin right after initiation, while
other patients improve after several months (Gossop 2006). Especially patients, who
were unsuccessfully treated in conventional drug treatment programmes, benefit form
prescribed heroin treatment (Rigter et al. 2004). Nevertheless, up to 60% of the clients
did not profit from the prescription of heroin and continue to be difficult to treat (Rigter
et al. 2004). Blanken et al. (2005) pooled the data of two open label randomised trials
including four hundred and thirty heroin dependents to investigate predictors for the
treatment response to medical heroin prescription compared to standard methadone
maintenance treatment (Blanken et al. 2005). The participants were randomly allocated
to methadone plus injectable heroin or methadone plus inhalable heroin administration
or to methadone alone prescribed over 12 months. The outcome measures were
recorded according to a response index, including indicators of physical health, mental
status and social functioning. An intention-to-treat analysis resulted in a significant
better treatment response for the participants in heroin-assisted treatment. Heroin
dependent patients with a history of several abstinence oriented treatments benefit more
from heroin prescription and show a higher treatment response compared to patients in
methadone maintenance treatment. Patients without a history of abstinence-orientated
treatment do not benefit more from heroin-assisted treatment than from methadone
maintenance treatment and show equal treatment response rates (Blanken et al. 2005). A
limitation of previous heroin trials was that psychosocial treatments were not
standardised and uncontrolled. A recent randomised controlled trial assessed the
efficacy of prescribed intravenous diamorphine (DAM) versus oral methadone
including clinical, psychological, social and legal support (March et al. 2006). Sixty-two
opioid-dependent individuals, who failed in standard treatments, were directly streetrecruited
and randomly assigned to the administration of intravenous diacetylmorphine
or oral methadone with equivalent opioid dosage. Both groups improved with respect to
physical and mental health as well as social integration, but the experimental DAM
group showed greater improvement in terms of physical health and risk behaviour.
Furthermore, in the experimental group, the use of street heroin decreased as well as the
number of days with drug problems (March et al. 2006).
In the recent open-label randomised controlled trial Haasen et al. examined the
effectiveness of medically prescribed and supervised heroin injection (Haasen et al.
2007). Overall, 1015 persons were included who represent one of two groups of people
with heroin dependence: those who do not sufficiently respond to methadone
maintenance treatment and those who are currently not in substance misuse treatment.
To control for the impact of psychosocial treatment, participants in each group were
randomised to one of two types of psychosocial care: psycho-education including
individual counselling or case management and motivational interviewing. Each of
these interventions has been described in manuals, and training of all therapists was
conducted prior to the study to minimise site differences. Heroin-assisted treatment of
severe opioid dependent and treatment resistant persons was found to improve health
and reduce illicit drug use more effectively than methadone maintenance treatment.
Retention was higher in the heroin (67.2%) than in the methadone group (40.0%) and
the heroin group showed a significantly greater response on both primary outcome
measures (health and illicit drug use). However, more serious adverse events were
found in the heroin group, and were mainly associated with intravenous use. The main
effect of heroin-assisted treatment on each primary outcome measure was seen within
the first few months of treatment, and became more pronounced over the following
months, thus indicating the necessity of long-term treatment to increase health benefits.
The use of two structured psychosocial interventions in each treatment condition
suggests that the observed differences between the methadone and heroin groups were
not the result of differences in psychosocial treatment. The response rates in the
methadone group also remain high, indicating that a well-structured treatment with
trained therapists using standardised and clinically relevant psychosocial interventions
can lead to positive outcomes even in a group that has previously responded poorly to
methadone treatment. Ferri et al. (2007) conducted in 2005 the most recent Cochrane
review to assess the efficacy and acceptability of heroin maintenance versus methadone
or other substitution treatments for opioid dependence (Ferri et al. 2007). A total of four
studies including 577 patients were found, but nevertheless a general conclusion about
the effectiveness of heroin treatment could not be drawn, due to the non-comparability
of the included studies (Ferri et al. 2007). With regard to the primary outcome measures
retention in treatment and relapse to illicit heroin use, opposite findings were found. In
summary, there is some evidence that heroin-addicted patients with a history of
abstinence-orientated treatment notably benefit from the prescription of heroin. Due to a
higher risk of serious adverse events, heroin prescription should be applied under
medical supervision.
Codeine/dihydrocodeine as maintenance agent
The analgesic agent codeine/dihydrocodeine is approved for maintenance treatment in
some European countries. Robertson et al. (2006) indicated that dihydrocodeine (DHC)
seems to be superior to placebo in the maintenance treatment of opioid dependent
patients (Robertson et al. 2006). Their recent pragmatic open-label randomised
controlled study investigated the efficacy of dihydrocodeine as an alternative to
methadone in the maintenance treatment of opiate dependence over a period of up to 42
months after recruitment (Robertson et al. 2006). Two hundred and thirty-five
participants suitable for opiate maintenance treatment were randomised to treatment
either with methadone (1 mg/ml) or with a lower (30 mg), respectively higher dose (60
mg) of dihydrocodeine tablets. The primary outcome measure (retention in treatment)
and eight secondary outcomes (including illicit opiate use measured by self-reports)
were compared over a period of 42 months. Although participants treated with
dihydrocodeine were more likely to switch treatments, no group differences in treatment
retention were found at follow-up and over the observation time. The authors concluded
that dihydrocodeine is a viable alternative to methadone for the maintenance treatment
of opiate dependence. In summary, more research on the efficacy of codeine for the
maintenance treatment of opioid dependents is needed, especially with regard to the
safety profile and cost-effectiveness of codeine maintenance due to the probably more
intensive treatment supervision. Provided that the good treatment retention in the study
by Robertson et al. (2006) will be replicated in other treatment settings including the
analysis of urine samples to confirm the reduction of illicit opioid use, codeine could be
an additional option for the maintenance treatment of opioid dependents. Provided that
the good treatment retention in the study by Robertson et al. (2006) will be replicated in
other treatment settings including the analysis of urine samples to confirm the reduction
of illicit opioid use, codeine could be an additional option for the maintenance treatment
of opioid dependents.
Slow-release oral morphine as maintenance agent
Slow release oral morphine (SROM) acts as an agonist on the μ-receptor and the long
duration of action permits to administer a once-a-day preparation. SROM has been
authorized for maintenance treatment of opioid dependence in a few European
countries, namely Austria, Slovenia and Bulgaria. Two recent RCTs compare the
effectiveness, safety and accessibility of slow release oral morphine to methadone or
buprenorphine, another one investigated the safety and withdrawal discomfort of the
transitioning of opioid dependent pregnant women from short-acting morphine to
buprenorphine or methadone (Eder et al. 2005; Giacomuzzi et al. 2006; Jones et al.
2005). Eder et al. found slow-release morphine to be as effective as methadone in the
treatment of opioid dependency. Sixty-four opioid dependent participants were
administrated daily under supervised conditions oral slow-release morphine or
methadone during two study periods, each consisting of a 1-week titration11 and a 6-
week fixed-dose treatment phase. The retention in treatment was high and no significant
group differences in treatment retention or use of illicit drug use were found,
irrespective of treatment group or medication. Patients treated with oral slow-release
morphine showed fewer psychiatric scores in depression and anxiety, so these findings
suggest a comparable safety and tolerability of oral slow-release morphine versus
methadone in equal doses. Giacomuzzi et al. used a randomised study design to
compare SROM to methadone and buprenorphine treatment with respect to quality of
life (QOL) and physical symptoms in patients entering treatment compared to patients
treated in an outpatient setting over a period of 6 months. Patients treated with SROM
showed lower quality of life values, despite equal effectiveness in the reduction of illicit
drug use compared to methadone and buprenorphine treatment (Giacomuzzi et al.
2006). However, other smaller and mostly open-label studies have shown positive
results of SROM with respect to retention, reduction of heroin use and/or quality of life
(Eder et al. 2005; Kraigher et al. 2005; Mitchell et al. 2004; Vasilev et al. 2006).
Furthermore, as with buprenorphine, there is criticism concerning the potential
diversion of prescribed SROM towards illicit drug use. Of special concern is the fact
that SROM has been found in most fatal intoxications in Austria in 2004, despite the
fact that most of these cases were not in maintenance treatment (ÖBIG 2006). Further
studies will have to confirm these results in order to be able to evaluate the added value
of this substance for the treatment of heroin dependence. In summary, SROM might be
a promising compound for maintenance treatment. Patients treated with SROM showed
improvements including decreased heroin consumption, improved functioning and a
decrease in delinquency. Slow-release morphine might represent a future treatment
option that will improve long-term outcomes for opioid dependents.
Pharmacotherapy for relapse prevention
In most European countries relapse prevention programs are offered, though the
duration and setting differ from country to country. While some countries limited
relapse prevention to long-term inpatient treatments intended to last at least nine months
and often using the therapeutic community format, others provided shorter inpatient
treatments generally lasting less than six weeks. The positive effects of both long-term
and short-term programs are, however, rather limited. In a three-month follow-up of 242
opioid dependent patients in residential treatment in the National Treatment Outcome
Research Study (NTORS), 34% of the patients relapsed to heroin use within three days,
45% within seven days, 50% within 14 days, and 60% within 90 days. According to the
authors, the results of this study highlight the need to provide aftercare services to help
patients maintain the benefits achieved during treatment and to avoid the high risk of
relapse at this time (Gossop et al. 2002). However, relapse prevention is also important
to reduce the spread of infectious diseases like HIV or HCV and should therefore be
widely available. Naltrexone, a long acting opioid antagonist, is used as a maintenance
pharmacotherapy for persons who detoxified completely from heroin and seems to be
helpful to speed up the withdrawal treatment and to prevent relapses (Gossop 2006).
However, due to the prevention of the euphoria effect of opiates, outpatient doubleblind
placebo controlled trials with long-acting opiate antagonist are very uncommon.
Placebo-controlled trials showed extremely high dropout rates, which implicates that the
general acceptability of the participants is low (Gossop 2006). One strategy to improve
treatment adherence includes the combination of naltrexone with voucher-based
contingency management (CM), which implies also increased treatment retention rates
and less illicit opiate use (Gossop 2006; Johansson et al. 2006). The additional effect of
CM was independent of other support measures and not related to the magnitude of the
vouchers. A most recent multi-centre study suggested high abstinence rates in patients
maintained with oral naltrexone in combination with a community reinforcement
approach (De Jong et al. 2007).
Naltrexone is considered to be a safe medication with few side effects; only high doses
can lead to transaminase elevations in liver function tests (Gossop 2006). However,
Stella et al. (2005) found high incidences of insomnia, panic attack, anxiety and
hyperexcitability12 in patients treated with oral naltrexone (Stella et al. 2005). In the
same study the additional administration of the benzodiazepine prazepam to oral
naltrexone maintenance was found to be effective in the reduction of this side effects
and to lead, in comparison to oral naltrexone alone, to higher abstinence rates from
illicit opioid use (Stella et al. 2005).
In summary, the effectiveness of antagonist maintenance with oral naltrexone for opioid
dependence has been limited by high dropout rates. Based on a systematic review of the
available evidence, according to the Cochrane reviewers no benefit was shown in terms
of retention in treatment, side effects or relapse results even compared to placebo
(Minozzi et al. 2006). Krupitsky et al. (2004) found oral naltrexone for heroin
dependence treatment to be significant superior to placebo with regard to treatment
retention and relapse over a period of 6 months (Krupitsky et al. 2004). However, these
results were found in a RCT with a small sample size. Naltrexone maintenance seems
not to be effective as a stand-alone treatment and should be, therefore, part of a broader
treatment programme or should be reserved only for highly motivated patients living in
a stable life situation. Nevertheless, a promising strategy to improve treatment retention
in broader range could be the combination of long-acting implantable naltrexone
formulations and behavioural methods.
Pharmacotherapy for the treatment of stimulant-related disorders
In summary, none of the proofed medication has been found yet that can be considered
a standard for treating stimulant dependence effectively, although a number of different
medications has been tried (EMCDDA 2007). The treatment of cocaine dependence
frequently still includes the use of antidepressants, especially SSRIs, despite the low
evidence level for their efficacy. Some typical and atypical psychotic agents such as
haloperidol, olanzepine and risperidone, were found to be effective in the treatment of
patients with co-occurring schizophrenia and cocaine dependence. Also promising
results are expected from topiramate and other antiepileptic drugs, and much hope is
being placed in the development of the cocaine vaccine.
Detoxification treatment for stimulant-related disorders
Propanolol (a non-selective beta blocker mainly used in the treatment of hypertension)
can moderate withdrawal symptoms but evidence is weak (Rigter et al. 2004). For
treating withdrawal symptoms in amphetamine dependence, amineptine (atypical
tricyclic antidepressant that selectively inhibits the reuptake of dopamine) has been
tested in two RCTs: it did not have an effect on withdrawal symptoms or craving, but
improved the general well-being of those who stop (Rigter et al. 2004).
Substitution treatment for stimulant-related disorders
There was one European RCT for dextroamphetamine (a psychostimulant which
produces increased wakefulness, energy and self-confidence in association with
decreased fatigue and appetite) and methylphenidate (a prescription stimulant
commonly used to treat Attention-deficit disorder (ADD) and Attention-deficit
hyperactivity disorder, or ADHD) each, the first showing that patients with 15-30 mg
stayed longer in treatment than placebo groups and those with higher doses, while
methylphenidate did not show effects (Rigter et al. 2004). Diethylpropion, act by
blocking and reversing norepinephrine transporter (NET) activity, also did not show any
effect on cocaine craving13 (Rigter et al. 2004). Sometimes amphetamines are given on
prescription, usually dexamphetamine, with good results in reducing street
amphetamine and other injecting drugs (Rigter et al. 2004). Prescribing amphetamines
is done in the UK for maintenance (Gossop 2006). Compared to a control group,
amphetamine prescription increased treatment contact and retention (Gossop 2006).
Another study found good results for dexamphetamine regarding retention and
compliance - patients attended more often counselling (Gossop 2006). Methylphenidate
(MPH), a prescription stimulant commonly used to treat attention-deficit hyperactivity
disorder (ADHD), was recently found to be effective for reducing intravenous drug use
in patients with severe amphetamine dependence respectively cocaine use in patients
with cocaine dependence (Tiihonen et al. 2007).
Abstinence maintenance for stimulant-related disorders
For abstinence maintenance for stimulant-related disorders, no medication has been
found yet to help on amphetamine or methamphetamine dependence (Rigter et al.
2004). Four different antidepressants have been tested in four RCTs with no influence
on the amphetamine use (Rigter et al. 2004). On antidepressant medication 21 RCTs
were found, with no effects also on cocaine dependence (Rigter et al. 2004). Szerman et
al. (2005) suggested that reboxetine might be an effective and safe therapeutic option
for cocaine dependence disorder including marked decreases in psychometric measures
during treatment (Szerman et al. 2005). One European effectiveness report also found
no effect for anticonvulsives (e.g. carbamazepine) according to six RCTs (Rigter et al.
2004). Rigter et al. found 12 RCTs on dopamine agonists and other substances, which
imitate dopamine, but no effects were found concerning a reduction of quantity or
frequency of cocaine use (Rigter et al. 2004). Also Berglund et al. found no effect
differences between dopamine agonists and placebo (Berglund et al. 2003). Typical and
atypical antipsychotics were not superior to placebo in treatment of cocaine dependents
except for patients with co-occurring psychotic disorders. Compared to placebo,
patients treated with the atypical antipsychotic medication aripiprazole were found to
have significantly more amphetamine-positive urine samples (Tiihonen et al. 2007).
However, typical and atypical psychotic agents such as haloperidol, olanzepine and
risperidone, were found to be effective in the treatment of patients with co-occurring
schizophrenia and cocaine dependence (Rubio et al. 2006).
The opiate antagonist naltrexone has not been found useful for treatment of cocaine
dependence (Rigter et al. 2004). Otherwise, Jayaram-Lindstrom et al. (2005)
demonstrated reduced consumption of amphetamine during treatment compared to pretreatment
in amphetamine-dependent patients receiving 12 weeks of treatment
comprised of naltrexone (50 mg) combined with relapse prevention therapy (Jayaram-
Lindstrom et al. 2005). The provision of disulfiram, an aversive drug producing an
acute sensitivity to alcohol, appeared to be more effective than naltrexone in the
provision of negative urine samples for cocaine and cocaethylene, but also suggested
that disulfiram does not add to the capability of CBT to retain cocaine dependents in
treatment (Grassi et al. 2007). Immunisation and vaccination are two strategies with a
long tradition and very little empirical proof of effectiveness. In (passive) immunisation,
catalytic antibodies are injected that bind cocaine and subsequently hydrolyse cocaine
into the inactive products ecognine methyl ester and benzoic acid. A cocaine vaccine
has also been proposed; this would attempt to block the effects of cocaine using cocaine
antibodies (Garcia Sevilla 1997; Navarro & Rodriguez De Fonseca 2000).
Pharmacotherapy for the treatment of cannabis related disorders
Neurobiological trials on cannabis withdrawal demonstrate the importance of the
development of further pharmacological options for the treatment of cannabis
dependence. Different published studies have employed laboratory animals to evaluate
medication effects on cannabinoid withdrawal symptoms. Nevertheless clinical trials of
human participants are rare and no European clinical trials were found supporting a
medication for the pharmacotherapy of cannabis dependence (Rigter et al. 2004).
Compared to placebo, nefazone (an antidepressant drug) decreased a subset of
withdrawal symptoms like anxiety and muscle pain, while bupropion worsened mood
during cannabis withdrawal. Rimonabant acts as an antagonist on the cb-receptor and is
supposed to reduce the pleasures of users of cannabis. Nevertheless, a non-randomised
clinical trial supports this assumption (Rigter et al., 2004). A conceivable approach
could be the blockade of alpha7 nicotinic receptors, which reverses abuse-related
behavioural in rats (Solinas et al., 2007).
Psychosocial interventions for the treatment of drug dependency
A wide range of psychosocial interventions is available for the treatment of drug
dependence. As many different study designs were used to explore psychosocial
treatment, it is difficult to compare the individual direct outcomes. Different approaches
are compared and different names used for similar forms of intervention. Different
kinds of treatment have showed different levels of effectiveness, but in general it is
clear than any psychosocial treatment is better than none (e.g. Amato et al. 2007), and
the quality of treatment also depends on the training and ability of staff (EMCDDA
2007).
As there is no effective pharmacological therapy for cocaine and amphetamine
dependence, a variety of psychosocial interventions has been conducted in this field,
whereas in the field of opiate dependence psychosocial interventions are most often
combined with pharmacological treatment, namely substitution maintenance treatment.
This combination leads to significant improvements (Berglund et al. 2003). Treatment
should match the patient and should be relevant to the individual (EMCDDA 2007).
Some form of treatment may be more useful for women than for men, others might be
better for cocaine users than cannabis users (Haro et al. 2006), so it is important to
carefully choose and provide the optimal treatment setting for the individual.
Psychosocial treatment usually improves substitution maintenance treatment outcomes
for opiate dependent patients. For opiate dependence psychosocial interventions have
been investigated in addition to pharmacological treatment (detoxification with
methadone or buprenorphine) in a Cochrane overview, with four different psychosocial
approaches (behavioural, counselling, family therapy, CM). Any of those treatments
were effective in terms of treatment completion, compliance and follow-up results
(Amato et al. 2007).
Cognitive-Behavioural Therapy (CBT)
Cognitive-Behavioural Therapy as a structured psychosocial intervention aims at
modifying cognition, behaviour, beliefs. Usually some kind of skills training and
practice to deal with craving is involved, as well as monitoring high-risk situations for
relapse. There can also be the focus on relapse prevention, by training the drug users to
develop skills on avoiding high-risk situations and to cope with such situations. Some
kind of cognitive-behavioural interventions are used in many therapy settings in Europe.
They might be modified and used in different approaches. Except for the review by
Rigter et al. (2004) there are no studies from the EU on evidence of the effectiveness of
CBT included in this report, so all research in this chapter comes from the USA and
Australia. Concerning the intensity of CBT, one trial found no difference: outcomes of
CBT were similar with the intervention given once or twice a week or every fortnight
(Rigter et al. 2004). One RCT on cannabis dependent users, who were not in treatment
before, compared one session of CBT with six sessions of CBT and a control group
with no treatment. The group with six sessions had higher abstinence rates than those
with one session (15% compared to 5%), both had less severe symptoms of dependence
than the control group after 7-8 months (on average) and those with 6 sessions had the
greatest reduction on the daily dose consumed compared with the other two groups
(Rigter et al. 2004). According to one study among mostly homeless and mentally
disordered crack smokers, CBT had better outcomes than a 12-step programme and CA
participation, but overall there was a high dropout rate (Rigter et al. 2004). Four studies
on CBT did not find success in relapse prevention for cocaine use (Rigter et al. 2004).
Motivational Interviewing (MI)
This intervention is based on cognitive-behavioural principles and was developed by
Miller and Rollnick (1991). MI does focus on enhancing motivation to change
problematic behaviour and uses methods like developing a feeling for discrepancies,
expressing empathy, support self-efficacy. It is often used as a brief intervention.
In substance-unspecific treatment, “motivational enhancement“ has been examined in a
number of research studies. In general good results were found with respect to the
willingness for abstinence or moderate use (Rigter et al. 2004). Motivational
enhancement has especially good outcomes at early stages of treatment (Gossop 2006).
Also for cannabis use positive results for MI have been found, i.e. greater reduction in
use and use-related problems (Gossop 2006). MI seems to be effective for improving
retention in heroin users in a drug-free treatment programme (Secades-Villa et al. 2004).
A comparison between standard assessment and enhanced assessment plus MI for drug
users found the latter group to be more likely to attend further treatment (Gossop 2006).
Even a one-session MI intervention has some beneficial effects on drug use among
young people, mainly on moderation of use and not cessation after three months
(McCambridge et al. 2004), but effects wore off at 12-month follow-up (McCambridge
& Strang 2005). A pilot trial on a single MI session for reducing crack cocaine use in
MMT patients found some impact on the crack use and significant reduction of heroin
use in the sample (Mitcheson et al. 2007). Brief Motivational Psycho-educational
Therapy (BMPT) improved motivation to undergo treatment, especially for women
(Haro et al. 2006). A randomised study found greater reduction in use and greater
likeliness of abstinence for amphetamine dependence than for the control group with a
self-help booklet (Gossop 2006). Drug users, who were court-ordered to undergo
treatment, were more likely to attend and complete treatment with MI than without
(Gossop 2006). A study on depressive cocaine users found fewer post-treatment
psychiatric problems and more patients remaining in treatment for MI intervention
compared to “treatment as usual” (Gossop 2006). But not all research was in favour of
MI interventions. One study did not find any effects of a brief MI intervention, which
was applied in addition to standard treatment (Gossop 2006). And another randomised
trial also did not find differences in abstinence of a brief motivational intervention for
young stimulant and alcohol users compared to a control group who received written
health risk information (Marsden et al. 2006).
Community Reinforcement approach (CRA)
The Community Reinforcement Approach (CRA) uses a range of methods and is based
mainly on cognitive-behavioural principles. Its concept includes that environmental
contingencies (like family, peers, work, leisure time involvement) can play a helpful
role in encouraging or discouraging drug use. CRA is often combined with Contingency
Management or similar incentive programmes.
For cocaine treatment the TRIMBOS report found reasonable indications of evidence
for “a change of lifestyle with CRA“ (Rigter et al. 2004). Two RCTs showed better
outcomes for CRA than for customary care (Rigter et al. 2004). Two other RCTs found
better outcome for CRA with compared to without rewards (vouchers) (Rigter et al.
2004).
Contingency management (CM)
Contingency management is another form of behavioural approach. The principle of
this approach is that “rewards” are given to those who have negative urine samples to
reinforce abstinent behaviour. Those incentives can be implemented in the form of
vouchers or prizes, and also privileges in the treatment setting. CM is usually embedded
in a treatment like CRA or structured drug counselling. As Contingency Management is
hardly conducted in Europe, research on the effectiveness comes almost exclusively
from the USA. CM was found to be effective in reducing drug use and treatment
retention, but these results tend to be short-term only. Generally CM results in good
treatment outcomes like retention and abstinence, but results tend to be short-lived
compared to CBT interventions (Rigter et al. 2004).
Cue exposure therapy (CET)
Cue exposure is based on learning theory principles. It consists of repeated exposure to
stimuli or cues associated with drug use (e.g. sight of o syringe for intravenous drug
users) and aims at controlling or changing responses to these cues. Until now this
intervention has been mainly done in laboratory conditions. The little research is not
considered to be promising (EMCDDA 2007; Rigter et al. 2004). One RCT from the
Netherlands on cue exposure therapy in an inpatient setting for opiate dependence even
found significantly higher dropout and relapse rates for the treatment group (Marissen et
al. 2007), so it does not seem to be an intervention that can be advisable presently.
Psychodynamic and interpersonal therapies
Psychodynamic interventions originate in the psychoanalytical approach and work on
unconscious conflicts, relationships and problematic situation. The therapist-patient
interaction and relationship is an important feature in this approach. Other Interpersonal
therapies focus on interpersonal relationships and issues as well, and aim at resolving
interpersonal problems.
No RCTs have been conducted for treatment using psychodynamic or interpersonal
therapy, but a case series on individual psychodynamic psychotherapy and some reports
on group psychodynamic therapy showed some efficacy. The Trimbos report stated that
the little existing research on psychoanalytical treatment showed no evidence for an
effect in treating cocaine dependence (Rigter et al. 2004).
Counselling/Group Counselling
Counselling can be defined as a client-centred intervention to help the individual to
overcome problems (EMCDDA 2007). In the US standard treatment is often based on
the 12-step principle, both for individual and group counselling. However, in Europe
counselling is not necessarily based on the 12-step principle. Counselling seems to be
useful for the moderation of use, as one RCT stated (Rigter et al. 2004). Also
counselling and psycho-education with respect to reducing the risk of HIV and other
infections has shown effectiveness (Rigter et al. 2004). While an effectiveness report
from outside of Europe suggested, that concerning reductions of use, the group and
individual counselling together was the most successful, the other three groups were
similar in outcome (UNODC, 2002), none of these treatments reduced the craving for
cocaine, and the Trimbos research group sees it as problematic that there was a high
dropout rate and also that not all the care providers were very experienced (Rigter et al.
2004).
Other group and family therapies
For opiate dependent patients in methadone maintenance treatment a group
psychotherapy showed less drug use than the MMT group only, therefore additional
psychotherapy is recommended for methadone maintenance treatment to improve
treatment outcomes (Scherbaum et al. 2005). Five RCTs on multidimensional family
therapy (MDFT) with young cannabis users who often had other problems as well found
favourable results on frequency of use and family functioning, compared to CBT and
other control interventions (Rigter et al. 2004).
5.5 Conclusion
Most studies included in pharmacological part of this review were conducted outside of
Europe. Overall two of three studies were conducted outside of Europe, whereas some
differences in several chapters attract attention. In the research on treatment of
psychostimulant- and cannabis-related disorders the included evidence from outside of
Europe is strongly predominant. Of the seventy-four studies, mainly randomised clinical
trials and other clinical studies included in the chapter of pharmacotherapy of
psychostimulant related disorders, sixty-four were conducted outside of Europe.
Similarly, the chapter on pharmacotherapy of cannabis-related disorders leaves a nearby
similar picture even though the number of included references is lower: Six of seven
studies were conducted outside of Europe. Furthermore all included studies on crisis
intervention and most on relapse prevention (thirteen out of twenty) of opiate-related
disorders were conducted from outside of Europe. A more balanced picture is found for
the pharmacotherapeutic detoxification and maintenance treatment of opiate-related
disorders. In the implementation of new maintenance agents for the treatment of opiate
related disorders (like SROM, diamorphine) the main research is conducted in Member
States of the European Union.
Most studies on psychosocial interventions come from outside Europe, mainly USA but
also Australia. Especially for cognitive behavioural interventions and for contingency
management there is hardly any evidence from European Member States, whereas for
other interventions it is more balanced.
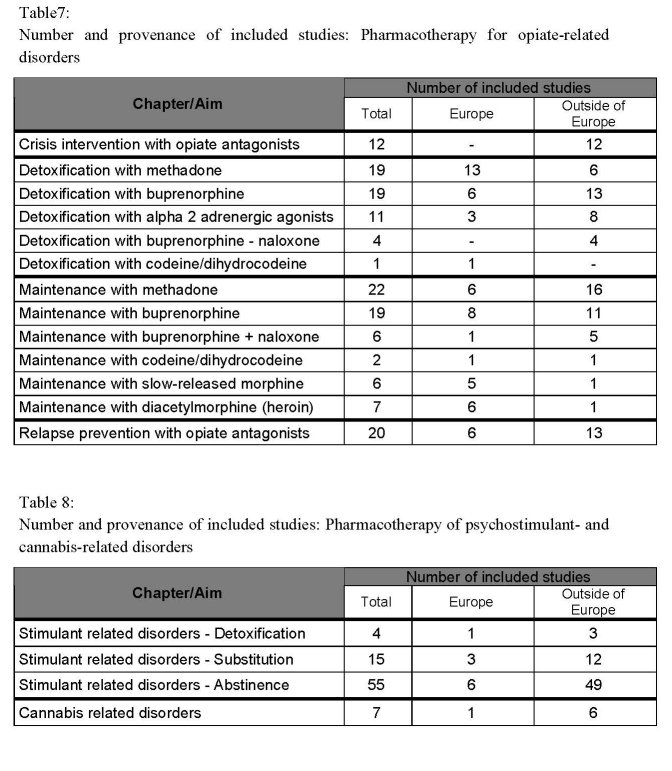
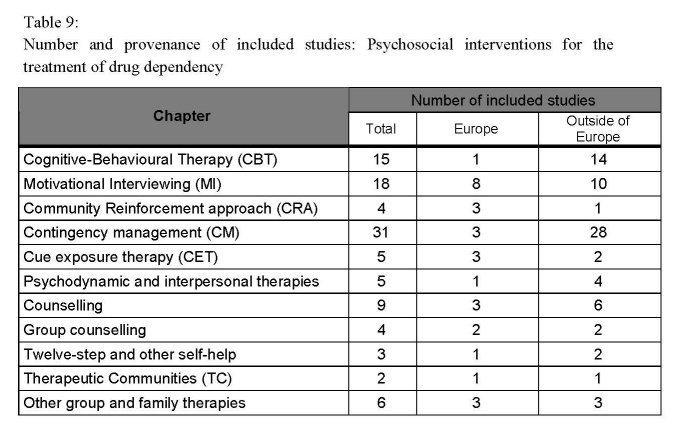 Table 9:
Table 9:
Taking into account the European and non-European evidence of effectiveness of drug
treatment the following conclusion can be made:
• Especially in the pharmacotherapy of psychostimulant- and cannabis-related
disorders and crisis intervention and relapse prevention for opiate related disorders,
as well in several psychosocial interventions like cognitive behavioural treatment,
Motivational Interviewing and Contingency management, research from outside of
Europe is predominant.
• In other areas the contribution of research activities from European Union Member
States is stronger, such as research on new agents for maintenance treatment for
opiate related disorders.
• Despite the heterogeneity of research data and varying evidence, several
interventions for the treatment of opiate-, psychostimulants- and cannabisdependence
were found to be effective. For withdrawal and maintenance treatment of
opiate dependence different pharmacological agents are available including full μ-
agonists (e.g. methadone), combined partial μ-agonists / κ- antagonists (e.g.
buprenorphine) and opioid antagonists (e.g. naloxone).
• Methadone is an effective pharmacotherapeutic agent for opiate detoxification, but
compared to the effectiveness of methadone in maintenance treatment, the efficacy
of methadone using tapered doses for detoxification treatment is limited and
especially the attrition rate in methadone detoxification treatment remains high,
particularly in an outpatient setting.
• There are some indications, that buprenorphine as well as the combination of
buprenorphine and naloxone have similar efficacy as tapering doses of methadone
for the treatment of opioid detoxification with comparable effectiveness in improving
withdrawal symptoms and in completing detoxification treatment and provides at
least more effectiveness in withdrawal management compared to clonidine including
fewer adverse effects.
• The replacement of heroin by buprenorphine in tapered doses followed by the
prescription of α2-adrenergic agonist (e.g. clonidine or lofexidine) to reduce
withdrawal symptoms proved to be an effective strategy for detoxification of opioid
addicts. Adrenergic agonists (clonidine and lofexidine) could be considered as an
effective detoxification option especially for patients, who prefer non-opioid
treatment for detoxification, but leads to more side effects and therefore to higher
drop-out rates especially at an earlier stage of treatment. Lofexidine showed fewer
side effects with similar clinical effectiveness in comparison to clonidine.
• A recent RCT provides only little evidence to support dihydrocodeine (DHC) as a
first line agent for opiate detoxification, and larger, well designed RCTs are needed
to assess the efficacy of DHC for detoxification.
• Methadone is the best-studied and most effective opioid agonist for maintenance
treatment so far. Treatment outcome in methadone maintenance has been shown to
improve substantially with increased dosages of methadone, whereas higher doses
are associated with better treatment retention rates and lower rates of illicit opioid
use. Daily methadone doses of 60mg/day or more were found to be most effective in
methadone maintenance treatment. Adequate dosing is an important issue and avoids
on the one hand unpleasant withdrawal symptoms, especially in the latter half of
each inter-dosing interval, and on the other hand significant adverse effects. The
combination with psychosocial treatment leads to a broader effectiveness, but even
methadone maintenance treatment without adequate psychosocial care has shown to
reduce heroin use and delinquency.
• Maintenance treatment with buprenorphine alone or in combination with naloxone
provides some advantages for the treatment of opioid dependence in comparison to
methadone, e.g. a better safety profile at high doses, a lower abuse potential, the
possibility of a less-than-daily administration and lower impairment in psychomotor
and cognitive functioning. Similar to methadone, the efficacy of buprenorphine in
maintenance treatment is dose related and higher doses of buprenorphine improve the
treatment outcomes. Provided equal effective doses, buprenorphine appears to be at
least as effective as methadone with regard to reduction of illicit opioid use and
treatment retention, whereas methadone maintenance in high doses is associated with
higher rates of retention in treatment and better suppression of withdrawal symptoms
than buprenorphine maintenance treatment.
• Current findings shown, that heroin-assisted treatment is a valuable addition to the
treatment repertoire, especially effective for people with opioid dependence who
continue intravenous heroin use while on maintenance or who are not enrolled in
treatment.
• Codeine and slow-release morphines could also be additional options for the
maintenance treatment of opioid dependents, provided that the first results will be
confirmed in larger well designed RCTs.
• There is some evidence, that naltrexone maintenance for relapse prevention is not be
effective as a stand-alone treatment. Nevertheless, a promising strategy to improve
treatment retention in broader range could be the combination of long-acting
implantable naltrexone formulations and behavioural methods.
• The pharmacological treatment of cocaine dependence frequently still includes the
use of antidepressants, especially SSRIs, despite the low evidence level for their
efficacy. More promising results are expected from topiramate and other antiepileptic
drugs, and much hope is being placed in the development of the cocaine vaccine.
• Similarly, different agents such as antidepressants, anticonvulsants, and
antipsychotics were investigated for the treatment of cannabis dependence and for
the prevention of cannabis reinstatement after abstinence, but each medication
missing broader effectiveness. Recent findings suggest that the administration oral
delta-9-tretrahydrocannabinol (THC) might be helpful in suppressing cannabis
withdrawal, but further research is necessary.
Psychosocial interventions play an important role in the treatment of the different types
of drug dependency. There is a wide range of different forms of interventions and not
all of them have shown sufficient evidence of their effectiveness. New approaches are
tried out and implemented, and others are used in modified versions. This makes it
rather difficult to directly compare different interventions. The high drop-out rate can be
problematic in some studies.
• In the field of maintenance treatment, the addition of psychosocial interventions,
especially behavioural approaches, are effective in terms of retention in treatment
and reduction of illicit drug use.
• For stimulant-dependency psychosocial treatment is especially important, as no
effective pharmacological treatment approaches exist. Therefore a great number of
psychosocial intervention studies are available especially on cocaine dependence.
But most research in this field comes from the US and is not always transferable one
to one to other countries, as the social context and also health system might be
different. Psychosocial interventions for cannabis dependence have only rarely been
investigated and concentrate mainly on young and adolescent users, often involving a
family therapy type of intervention. Generally speaking, most psychosocial
interventions are helpful in reduction of use, retention in treatment and social health
development.
• Voucher-based interventions are especially helpful on short-term outcomes, whereas
behavioural approaches like CBT tend to be more long-lasting.
• Methods of Motivational Interviewing (MI) have shown effectiveness particularly for
those with initial low motivation and less severe dependency.
• And cue exposure therapy seems to have contrary effects according to one RCT,
where drop-out and relapse was higher for the cue exposure group.
• There is some evidence for different types of counselling and 12-step approaches,
especially when they are integrated in a structured programme. Altogether there is
rather little research on special subgroups, particularly poly-drug users, as well as
women, adolescents or those with co-morbid psychiatric disorders.
In summary, most research on the effectiveness of pharmacological and psychosocial
interventions is conducted in the United States of America (USA). In the
pharmacological part two of three; in the psychosocial part four of five included studies
are from outside of Europe, mainly from the USA. In several pharmacotherapeutic
issues (like opiate antagonists for crisis intervention and relapse prevention,
pharmacotherapy of psychostimulant- and cannabis-related disorders) and most
psychosocial issues (especially cognitive behavioural interventions and contingency
management), evidence from outside of Europe, mainly USA but also Australia, is
predominant. On the other hand, pharmacological drug related research from Member
States of the European Union is leading in research on the implementation of new
agents for maintenance treatment of opiate related disorders (such as slow-release oral
morphine (SROM) and diacetylmorphine (heroin)).
1 Gradually reducing methadone over time
2 SAE = untoward medical occurrence results in e.g. death, life-threatening, inpatient hospitalization
etc.
3 Month four through six of the pregnancy
4 SSRI = a class of antidepressants used in the treatment of depression, anxiety disorders etc.
5 Standard questionnaire; provided patient’s aggregate score on amphetamine withdrawal
6 Phase I of clinical trials: First stage of testing a drug/agent/medication in human subjects
7 Benzoylecgonine is the major metabolite of cocaine
8 DSM = Diagnostic and Statistical Manual of Mental Disorders; list of categories of mental disorder
and the criteria for diagnosing them
9 Gradually reducing methadone over time
10 = Health care provider as a first point of consultation or treatment
11 = Process of gradually adjusting the dose of a medication until the desired effect is achieved
12 = generalised term: cover a spectrum of disorders that exhibit the symptoms of continuous muscle
fiber activity
13 = strong desire for the substance causing the dependence
| < Prev | Next > |
|---|












