18 Proposal for an exchange system
| Reports - Models of Good Practice in Drug Treatment |
Drug Abuse
18 Proposal for an exchange system
Objective of the “Moretreat”-project was to develop recommendations for a concept for a European platform that provides “good practice protocols” in drug treatment and allows the implementation of a continuous exchange and improvement process. The platform should enable the improvement of the dissemination of good practice in Europe. The following inventory refers to the action plan on drugs as the political background. In particular objective 7 of the EU Action Plan on Drugs 2005-200820 states the need to improve coverage of, access to, quality and evaluation of drug demand reduction programmes and to ensure effective dissemination of evaluated best practices. Accordingly, the provision of information on best practices in the Member States and the facilitation of exchange of such practices are mentioned as tasks of the EMCDDA in article 2 of the recast of the EMCDDA regulation, which was adopted by the European Parliament and the Council of the European Union in December 200621 .
Important aspects of an exchange system are
• Mechanisms of continuous development and presentation of given protocols for different areas of treatment (modalities, system level, cross cutting issues)
• Clarification of different forms for the consensus building and selection process for additional or special areas of drug treatment as well as for revision of existing protocols
• Clarification of possible relations of a possible additional exchange platform with existing concepts for platforms for good practice (drug treatment and other treatment areas) with EMCDDA, public Health officials in Europe and in the Member States.
For the proposal the term ‘knowledge transfer’ is understood as part of the knowledge base and the knowledge infrastructure in the area of drug related interventions. The transfer is an important aspect of efforts for evidence-based interventions and policy. Over the last decades different systems have developed that enable the development and dissemination of knowledge-based interventions in the areas of health services and care related interventions. This process started first for medical interventions but has expanded to health care in general and also to interventions related to drug problems, to prevention and treatment including the different areas of pharmacological and psychosocial interventions, and also to policy action.
The investigation of the current situation in this area is the starting point the proposed improvement of exchange of good practice in the field of drug treatment.
18.1 Methods
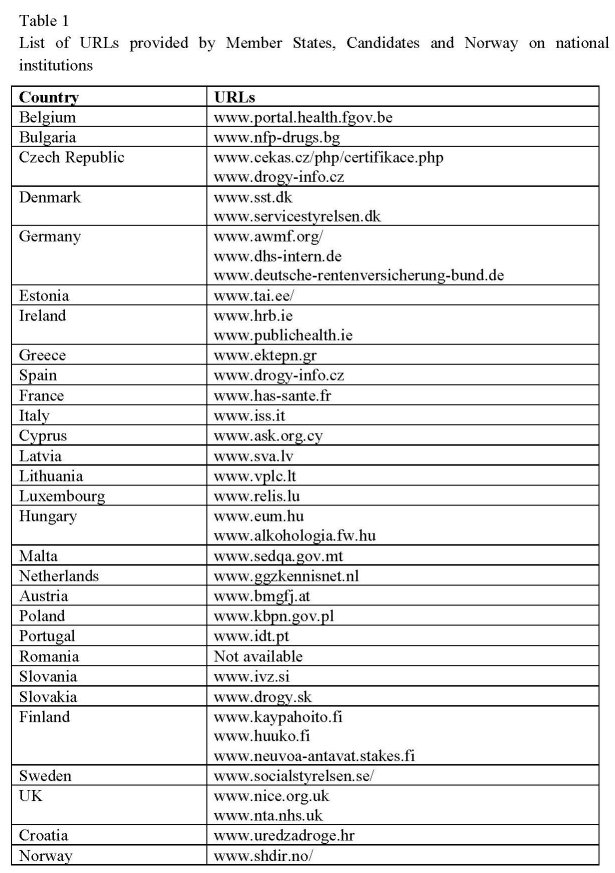
To define the next step for a knowledge transfer it is important to understand the current situation as regards the production of guidelines, their implementation in drug treatment, evaluation and improvement at European level. This includes an overview/survey of existing multipliers that play an important role in the development, collection, dissemination and transfer of good practice in each country (but also at the European level). The inventory of existing platforms for “good practice protocols” in the Member States
(e.g. ‘Models of care’ in England or ‘Resultaten scooren’ in the Netherlands) and at international level (e.g. SAMHSA in USA) serve as examples. Different platforms and efforts of knowledge transfer mainly in the drug treatment area are investigated as basis for a proposal of an exchange system in Europe:
• European network for Health Technology Assessment -EUnetHTA
• World Health Organization has launched the Health Evidence Network (HEN)
• The “National Treatment Agency” (NTA) for substance misuse in England
• Treatment Improvement Protocols“ (TIP) and „Treatment improvement exchange“ (TIE) of the Centre for Substance Abuse Treatment (CSAT) in USA
• Pompidou Group and their role in knowledge transfer
• EMCDDA online portal about best practices – concept of the EMCDDA The investigation of existing European platforms is completed by an overview related to the knowledge transfer in all Member States. This overview is based on an inventory which was realised by the project coordinator in cooperation with the EMCDDA in 2007 (see for details – Degkwitz et al. 2007). The overview refers especially to criteria for quality, selection process, consensus building and the regional knowledge transfer/exchange mechanism.
18.2 Inventory of exchange platforms and knowledge transfer for good practice in health care and drug treatment
A short overview concerning best practice development and exchange in Europe related to health care in general and drug treatment in particular is presented below. In Europe, the issue of best practice exchange has relatively a short history. The first institutions dedicated to the evaluation of health care technologies were established in the 1980s, initially at regional/local level in France and Spain. The first national agency for Health Technology Assessment (HTA) was established in Sweden in 1987. The late 1980s and the 1990s can be described as the era of institutionalisation of HTA in Europe. Since then, in almost all countries of the European Union programmes for HTA have been established through either the foundation of new agencies or institutes or by establishing HTA departments or units in universities or in other existing governmental and non-governmental bodies (Velasco-Garrido & Busse 2005). Several reviews of the stepwise development and institutionalisation of HTA in Europe have been conducted, each with different focuses and levels of comprehensiveness (see Velasco-Garrido & Busse 2005). The heterogeneity of HTA institutions in Europe reflects the variety of traditions and socioeconomic contexts of European health care systems. There are agencies for HTA with national mandates and those with regional ones. There are HTA institutions conceived to support decisions only at the level of investment in equipment for hospitals and those expected to give advice about policies concerning the organisation of the whole health care system. HTA might be directly committed and funded by governments (national or regional) or by non-governmental organisations spending public money. The bodies performing HTAs are mainly funded by resources from the health care system or from the national research and development budget. The task of this chapter is to report on different network models of good practice development and exchange/transfer in health care in general. In principle, all following platforms have connections to drug treatment interventions though with great differences in practice. The chapter is starting with describing general health networks in Europe and at WHO level. Subsequently two exemplary national platforms for best practice dissemination on substance misuse from England and the USA are introduced. Finally the actual European concepts (Pompidou group and EMCDDA) for knowledge transfer in the area of drug treatment are presented.
The presentation of exchange platforms, HTA programmes, and quality assurance systems refers to the
• European network for Health Technology Assessment -EUnetHTA
• World Health Organization (WHO) – the Health Evidence Network (HEN)
• Cochrane Collaboration
• Guidelines International Network (G-I-N)
• Pompidou group and their role in knowledge transfer
• EMCDDA online “best practice portal”
In relation to the mentioned platforms the following aspects are of particular interest:
• Process of the production of guidelines in connection with research, evaluation, evidence reports
• Criteria for quality, the selection process and consensus building
• Knowledge transfer/exchange mechanism
A system of collecting and disseminating evidence – the development of the “European network for Health Technology Assessment” - EUnetHTA22
“Health technology assessment (HTA)” has been defined as “a form of policy research that systematically examines the short- and long-term consequences, in terms of health and resource use, of the application of a health technology, a set of related technologies or a technology related issue” (Henshall et al. 1997). HTA is concerned with the medical, organisational, economic and societal consequences of implementing health technologies or interventions within the health system.
Areas of Health Technology are diagnostics and treatment methods, pharmaceuticals, rehabilitation and prevention methods and also organisational and supportive systems that build the frame for health care provision. The aim of HTA is to formulate safe, effective health policies that are patient focused and seek to achieve best value. In principle the aim comprises as well different aspects of the problems of drug treatment interventions.
The declared purpose of HTA is to support the process of decision-making in health care at policy level by providing reliable information. In this respect, HTA has been compared to a bridge between the world of research and the world of decision-making (Battista 1996). This bridge is intended to allow the transfer of knowledge produced by scientific research to the decision-making process. In order to achieve this objective
HTA is committed to the work of collecting and analysing evidence from research in a systematic and reproducible way, and to make it accessible and usable for decisionmaking purposes, in particular by means of assessment reports.
HTA shares these principles with evidence-based medicine (EBM) and clinical practice guidelines (CPG) and, together with them, builds a body of best practice initiatives (Perleth et al. 2001).
To learn about the knowledge production and exchange it is necessary to look at the implementation of HTA in Europe. In 2004, the European Commission and Council of Ministers defined Health Technology Assessment as “a political priority”, recognising “…an urgent need for establishing a sustainable European network on HTA”. A Commission call was answered in 2005 by a group of 35 organisations throughout Europe, led by the Danish Centre for Evaluation and HTA (DACEHTA) in Copenhagen. The European network for Health Technology Assessment, EUnetHTA, coordinates the efforts of 27 European countries including 24 Member States of the European Union in evaluating health technology in Europe.
The general strategic objective of the Network is to connect public national/regional HTA agencies, research institutions and health ministries in order to enable an effective exchange of information and support to policy decisions by the Member States. During the first 3 years of existence (2006-2008) EUnetHTA aims at developing an organisational framework for a sustainable European network for HTA along with practical tools to ensure timely and effective production, dissemination and transfer of HTA results.
Initially, the EUnetHTA project is being co-financed by the European Commission (DG Sanco) and contributions from network members.
Specific objectives of EUnetHTA are:
• To establish the organisational and structural framework for the network with a supporting secretariat.
• To develop and implement generic tools for adapting assessments made for one country to new contexts.
• To develop and implement effective tools to transfer HTA results into applicable health policy advice in the Member States and EU – including systems for identification and prioritisation of topics for HTAs and assessment of impact of HTA advice.
• To effectively disseminate and handle HTA results, information sharing and coordination of HTA activities through the development and implementation of elaborate communication strategies and clearinghouse activities.
• To monitor effectively emerging health technologies to identify those that will have greatest impact on health systems and patients ().
• To establish a support system in countries without institutionalised HTA activity EuNetHTA as a relevant network is also concerned with the assessment of evidence in the area of drug related action. However, up to now psychosocial interventions in general and especially in drug treatment are a subordinate issue.
The HTA-process contributes to the collection of evidence in the field of drug treatment and also to the dissemination of knowledge. One option is a systematic promotion of these developments.
World Health Organization (WHO) – the Health Evidence Network (HEN)23
The Regional Office for Europe of the World Health Organization has launched the Health Evidence Network (HEN), an Internet-based resource, whose aim is to provide evidence-based answers for questions posed primarily by public health and health care policy-makers in the European Region (www.euro.who.int/HEN). HEN is conceived as network of technical members and financial partners, involving United Nations agencies with a mandate related to health, organisations working with evidence-based health policy and health technology assessment, other institutions and governments interested in funding advanced projects related to public health issues. HEN works with more than 30 international agencies and institutions. They contribute to HEN by, for example:
• proposing questions for response through HEN,
• proposing experts to write and peer review responses to questions,
• identifying and providing evidence for inclusion,
• disseminating the evidence from HEN, and
• suggesting areas for further project development.
The HEN provides concise and standardised reports on available evidence on topics currently under discussion in the countries of the European region, such as reduction of hospital beds or the implementation of disease management programmes. The rationale of HEN is the growing need for timely and relevant information for decision-making. HEN makes it easier for policy-makers and other interested parties to get rapid access to much of this information in one place. Services of HEN are the provision of summarised information from a wide range of existing sources: web sites, databases, documents, national and international organisations and institutions. HEN also replies to specific questions that public health and health care policy-makers may have. The methodological proceeding of HEN after receiving a request is to mobilise a team of specialists, including members of HEN, who search for existing evidence in the area and use it to develop a synthesis report. When the evidence is contradictory, the report outlines the context and level of the debate. Each report goes through three reviews:
• an initial review by the HEN team
• an internal and external peer review
• a quality control by the HEN team
A steering committee advises HEN on its aims, objectives, strategies and approaches. As regards evidence, the WHO/Europe has, with the advice and help from the high-level European Advisory Committee on Health Research, adopted a broad definition of evidence that includes research findings and context-related information from other types of knowledge. Evidence is defined as "findings from research and other knowledge that may serve as a useful basis for decision-making in public health and health care" (European Advisory Committee on Health Research 2003). Working together, HEN and the European Observatory on Health Systems and Policies have launched a new series of joint policy briefs to address questions related to the health system policy in Europe.
• The objective is to produce high-quality, accessible material that is of immediate interest to national policy-and decision-makers seeking key messages based on solid foundations, that can be used by researchers and experts as brief but authoritative reviews.
• In addition to a rigorous peer review process – comprising two external reviews and one internal review – a knowledge-transfer review will be an integral element in the new series. The aim is to ensure that each brief highlights the link between research/evidence and health policy.
• Joint policy briefs will be generated in consultation with Member States stakeholders and reviewed by an international advisory board, as well as the editorial team.
HEN disseminates the evidence-based work of its members by providing it as far as possible the web site. In principle the HEN platform is open for questions and evidence assessment for drug related actions, especially drug treatment interventions and policy actions. However, up to now (August 2008) this platform contains no drug related reports (with the exception of one alcohol related report).
Cochrane Collaboration
The Cochrane Collaboration is an international non-profit-making organisation that produces and disseminates systematic reviews of health care interventions and promotes the search for evidence in the form of clinical trials and other studies of interventions.
The Collaboration’s major product is its database of systematic reviews. These are based on the best available information about health care interventions. They explore the evidence for and against the effectiveness and appropriateness of interventions (medications, surgery, education, etc.) in specific circumstances. The reviews are prepared by health care professionals and published in the Cochrane Library.
The Cochrane Library is a collection of high-quality evidence-based health care databases, providing instant access to over 2000 full-text articles reviewing the effects of health care interventions. It is published every three months with new and updated Cochrane reviews.
The concept contains production and dissemination of systematic reviews also for the field of drug treatment interventions. For many relevant interventions such reviews are available. These products are important references for the production und dissemination of good practice in drug treatment.
Even though the results are a basis for the elaboration of guidelines and best practice models, the transformation of evidence in guidance for practice is not in the focus of the Cochrane Collaboration.
Guidelines International Network (G-I-N)
The Guidelines International Network (G-I-N)24 focusses on the identification, development and dissemination of guidelines. This is aspired in close cooperation with Cochrane. G-I-N is an international non-profit association of organisations and individuals involved in the development and use of clinical practice guidelines.
In fact, G-I-N seeks to improve the quality of health care by promoting systematic development of clinical practice guidelines and their application into practice, and through supporting international collaboration and dissemination. In October 2008 more than 5,400 documents were available on this site. At present only a few guidelines for drug treatment are available (for example: NICE (GB) report: Drug misuse:
psychosocial management of drug misusers in the community and prison settings (CG51)25).
G-I-N, founded in 2002, is a consequence of many countries that have built up experience in the development, appraisal and implementation of clinical practice guidelines at professional, institutional, regional and national levels. Guidelines activities have taking place all over the world. At the European level this proceedings have resulted in the “Recommendation of the Council of Europe on Guidelines Methodology” and in a generic methodology for guideline appraisal (AGREE Instrument). As well G-I-N was established as forum for communication between those involved in developing, appraising and implementing clinical guidelines.
A major stimulus to international cooperation in guideline development in recent years has been the AGREE Collaboration which was formed in 1998 to develop a common guideline appraisal instrument. The AGREE project highlighted the increasing harmonisation of the methodologies used by guideline agencies and programmes around the world, and the Collaboration itself provided a forum for guideline developers, researchers, and implementers to meet and share ideas.
The concept and the objectives of G-I-N provide information on what is necessary in the field of development and dissemination of guidelines for drug treatment interventions. Unfortunately guidelines for drug treatment interventions are not priority area up to now, and available guidelines are delivered casually and not based on an (European) planning.
Pompidou Group and their role in knowledge transfer
With respect to the knowledge transfer and exchange of “good practice” the core mission of the Pompidou Group is to contribute to the development of multidisciplinary, innovative, effective and evidence-based drug policies in its involved 35 states. It seeks to link policy, practice and science and focuses especially on the particularity of local implementation of drug programmes.
The shifting, dynamic nature of the drug phenomenon required of the Group to adapt its role in order to deal with emerging problems and changes in the drug situation.
Against an international background characterised by the presence of many European and international bodies working in the field of drugs, the Pompidou Group provides a multidisciplinary forum at the wider European level where it is possible for policymakers, professionals and researchers to discuss and exchange information and ideas on the whole range of drug misuse and trafficking problems. In order to carry out this mission the Pomidou Group adopts a multidisciplinary, integrated approach to all drug problems and employs a variety of working methods.
Because of its links with the Council of Europe the Pompidou Group also ensures that policy recommendations are consistent with public policy as elaborated in other fields of the Council’s work, such as public health, social cohesion and penal policy and with particular emphasis on ethical issues.
The Research Platform’s prime role is to better support the utilisation of research evidence in policy and practice thus facilitating the development of evidence-based policy. Moreover, it signals the latest issues that arise from drug research in the social and biomedical fields and promotes interaction between research disciplines such as these and psychological drug research.
To improve the exchange of knowledge which has been identified as a major gap during the Strategic Conference on linking research, policy and practice – (“Lessons learned, challenges ahead”) – the online register has been devised in collaboration with the EMCDDA and in accordance with recommendations of the EU Horizontal Drug Group.
The online register devised in 2007 and updated in 2008 offers the possibility to find out who does what in drug research. This initiative is an attempt to improve the exchange of knowledge in drug research. The register contains details of more than 320 researchers and information on about 100 research projects.
The registration of institutes, researchers and actual projects in the field of drug research is an important aspect of exchange of research, but only the first step in the direction of exchange of good practice.
Online “best practices portal” – the concept of the EMCDDA
Based on the initially mentioned political background of the ongoing EU Action Plan that stated the need to improve the provision of information on best practices in the Member States, the task of the facilitation of exchange of such practices is mentioned in the EMCDDA regulation.
The promotion of information dissemination of science-based practices was then included in the EMCDDA 3-year work 2007-2009 programme’s objectives. The Centre recognises that an important but currently under-developed area of work of the EMCDDA is to place the descriptive data in the context of identifying and sharing information on best practices.
Main objectives of the best practice portal are to provide an overview of the latest evidence on the effectiveness of different interventions. It will also present tools and standards aimed at improving the quality of interventions, as well as highlighting best practice examples from the field. The portal is primarily aimed at professionals, policymakers and researchers in the drugs field.
Areas covered in the portal:
(A) Latest available evidence on the efficacy/effectiveness of interventions (summary of knowledge based upon latest reviews)
The overall objective is to provide an online overview on:
• Summary of the conclusions/main findings based on the latest reviews26 (published since 2000) of universal school-based prevention programmes27 .
• Overview of applied methodology used in each of the reviews (i.e. criteria for inclusion of studies, review procedure, rating system applied to assess the strength of evidence).
Additional information is provided for the reviews:
• Reference of all studies, systematic reviews, meta-analysis and their abstracts that were taken into consideration in the presented reviews.
• Glossary (all technical terms will be defined, i.e. meta-analysis, randomised controlled trials)
• Summary of content of selected publication on how to assess the quality of systematic reviews and meta-analysis.
• Acknowledgement of limitations of the overview. I.e. the EMCDDA acknowledges that literature reviews on the effectiveness of interventions pose problems because they have not taken into account all relevant published or unpublished systematic, unsystematic reviews or meta-analyses or individual studies. In addition they are subject to reviewer bias, often biased towards English language publications as well as limited to the provision of evidence of what works under controlled research conditions rather than in real-life conditions. Another source that provides useful information on what works in the drug demand reduction field are the views of practitioners who have experience in the implementation of interventions as well as opinions of persons who are recognised as experts in particular fields of interventions.
(B) Tools to evaluate practices
This area will compile existing EMCDDA information on how to evaluate demand reduction activities such as PERK (Prevention Evaluation Resource Kit), EMCDDA guidelines on evaluation of treatment services, workbooks on the evaluation of psychoactive substance abuse treatment, as well as the evaluation instrument database (EIB) which provides tools that can be used for the evaluation of processes and outcomes. Additional material will be added to this section if regarded as relevant and scientifically sound.
(C) Standards, guidelines for the implementation of practices
This area will focus in a first phase on the description of existing quality standards for interventions in Member States as well as existing national guidelines for the implementation of practices (i.e. national guidelines on clinical management of substitution treatment).
Quality standards
Quality standards or minimum standards belong to the most traditional aspect of quality assurance in service delivery. They specify what agencies should attain in meeting the needs of their clients. These standards set out criteria for the structure of various aspects of service delivery, including the agency organisation and management, patient assessment, treatment delivery (but not content), patient rights, evaluation and staff training and development. Existing models of standards for intervention content (i.e. treatment content) beyond basic procedural aspects of operations will also be described.
Guidelines
A first step will be the collection of national drug use and dependence guidelines on clinical management from Member States. These may refer to guidelines generally concerned with the clinical management of drug misuse and dependence as well as those that focus on specific areas of interventions such as substitution treatment or target groups (i.e. guidelines on clinical management of drug dependence for GPs).
(D) Data base on evaluated Drug Demand Reduction projects in MS, including best practices
Established in 1996, EDDRA provides details on a wide range of evaluated prevention, treatment and harm reduction programmes in the EU, while promoting the exchange of professional expertise and hands-on experience. EDDRA is designed to help professionals and policy-makers planning and implementing interventions in response to drugs. Currently EDDRA contains more than 600 entries. In 2007, EDDRA has been reviewed and reclassified by the EMCDDA and its national EDDRA managers in a move to improve the system’s content and layout. To better identify best practice in evaluation, projects will be structured according to a 'logic model' and classified according to type of intervention and level of quality. This reclassification takes place in the context of the EU drugs action plan (2005–2008) which calls for the ‘effective dissemination of evaluated best practices’ and the EMCDDA’s new mission statement which prioritises the provision of such information. The new-look EDDRA will be migrated to a new technical environment allowing for an improved online presentation of its projects. It will also be integrated into the online portal.
Procedure for the classification of revised projects according to level of quality
Currently all projects that undergo a revision are being classified by two independent project managers according to three basic levels of quality criteria. Level 3 is the most important level (=model projects in EDDRA) and demands:
Content
Based on a theory that is clearly related to the objectives, the initial situation and the indicators.
Type of design chosen
Research design – Control group (CT/RCT Logic model plausible? Can the main elements of the programme be described in a Logical Graphical Model (i.e. flow chart)?
Measures – the operational relevance and psychometric quality of measures used in the evaluation.
Dissemination -Provision of all programme material as well as evaluation tools
The “Best practice portal”28 has started – as planned – in 2008 with a general structure following the concept:
Evidence of efficacy
This section contains reviews on the efficacy of different types of intervention. (This has started but up to now only with collection and transfer in the field of prevention.)
Tools for evaluation
This area contains EMCDDA information on how to evaluate demand reduction activities.
Standards and guidelines
This section contains standards and guidelines for the implementation of practices.
Examples: EDDRA
The Exchange on Drug Demand Reduction Action (EDDRA) provides real-life examples of evaluated practices in the European Union.
18.3 Overview: Guidelines, quality assurance and knowledge transfer in drug treatment in the Member States
Among the European countries there are different mechanisms which rule the identification and dissemination of treatment know-how. These mechanisms also differ with respect to the implementation of an evidence-based culture in the respective national drug treatment systems.
Analysing the status quo of the “knowledge transfer and exchange system of ‘good practice’” implies to assess the main components of the “Quality Systems” in Member States. Accordingly the status quo of quality assurance, knowledge transfer, sharing of experiences and good practice in the drug treatment area in the Member States and Norway has been investigated.
To assess the existence and of the level of quality assurance in drug treatment the following has been considered as main assessment indicators:
• Guidelines – existence, relevance, commitment, contents, funding, guidance for guidelines?
• Guidelines – sources: based on best practice, evidence reports, consensus building process?
• Monitoring – different stages of reporting
• Evaluation – existence and level (systematic, connection to research?)
• Research – outcome studies in drug treatment, clinical research, reviews, evidence reports?
When summarising the current „quality system“ in Member States – which implies the development, dissemination, and transfer of good practice – the following main conclusions can be drawn.
Quality assurance system in the field of drug treatment has been developed in the majority of the Member States. At the same time main components for knowledge transfer and best practice transfer are only partly implemented at present. This is especially the case for:
• Evaluation and research: While evaluation is realised sporadically, research is inadequately developed.
• Reviews and evidence reports: With few exceptions both has not been established as standard in the Member States. Reviews and evidence reports are most likely to be implemented in medical treatment such as substitution and detoxification.
• A systematic procedure for producing and controlling new protocols -as standard for achieving best practice is not yet implemented.
• The consensus process for development of guidelines is currently mostly based upon expert panels.
The evidence based development of guidelines and the transfer of good practice in the filed of drug treatment can be defined as to be at an initial stage compared to other areas of the health system. Currently there are considerable limitations in the transfer of good practice as regards their correspondence with the tasks of the drug action plan and the demands in drug treatment. These gaps are most evident in the realisation of a knowledge infrastructure concerning an exchange system for “good practice” and knowledge transfer.
Regarding the implementation of guidelines and standards in the treatment system, the situation in the Member States can be described according to following basic categories.
• In the first group of states the dissemination of guidance mainly occurs through policy makers and institutions authorised by them.
In this category, public authorities are responsible for the identification and dissemination of defined guidelines and standards for providers. This is an important part of a developing quality system. The dissemination of know-how is mainly based on the experience of different decision-makers – such as policy makers, providers and professionals – and on expert consensus.
The guidelines are mainly limited to general structural aspects of treatment services or interventions. This kind of development and dissemination of guidelines has only a loose connection to drug research; existing research is not regularly involved in the evaluation. There is no regular adaptation/improvement of guidelines based on evaluation, research or evidence reports.
• In the second group the development of standards and guidelines is influenced to a greater extent by professional associations.
The transferred guidelines are based on experience in combination with evaluation of treatment interventions and research. Professional associations and public authorities are responsible for the dissemination. Dissemination is carried out through professional and scientific channels. These are e.g. publications in national scientific journals, newsletters of involved associations, manuals for interventions, workshops and congresses. This is the traditional structure of quality assurance and a transition to evidence-based identification and dissemination of knowledge is ongoing.
• The third group represents a fully developed knowledge infrastructure as background for knowledge transfer.
Dissemination of treatment know-how is based on continuous data collection and evaluation of existing services. The process of identification, preparation and transfer of „good practice“ is concentrated in a commissioned institution acting at national level. This agency can be organised in very different ways. The institutionalisation of a knowledge infrastructure for optimal response is influenced by very different traditions in the individual European Member States. Depending on the national tradition, there exist different links to research. Research can be directly integrated (e.g. if the responsible institution emerged from public health or drug research) or the connexion is assured by relations of cooperation (institutes for quality assurance, institutes for clinical excellence, public health and drug research units). Depending on the constituting role played by the associations of providers in drug treatment, the professional associations of different professional groups involved in drug treatment, public health or drug research units, or university hospitals involved in treatment and research, the “national agencies” are either directly attached to the health ministries or operate as relatively independent networks. The individual Member States can be assigned to one of these categories. E.g. the United Kingdom and the Netherlands belong to the group of countries with a full developed system. The Scandinavian countries are in the process of implementing an evidence-based culture of identification and dissemination of know-how in drug treatment. As reported in the country profiles the “good practice” transfer system is only partly implemented and on an initial stage.
18.4 National examples of an exchange system in drug treatment
As an example for countries with a fully developed system for production and exchange of good practice the United Kingdom will be presented in the following. Although the Netherlands has as a similar developed system (www.ggzkennisnet.nl), most evidence reports and protocols are only available in Dutch language. Only some parts of the system (“fact sheets”29) are available in English.
After describing the example of the UK a short introduction in the system of the United States is given. Even though the US system this is not transferable to Europe, it serves as a role model for a fully developed system.
The “National Treatment Agency” (NTA) for substance misuse in England
The National Treatment Agency (NTA)30 is a special health authority, created by the Government in 2001 to improve the availability, capacity and effectiveness of treatment for drug misuse in England. In other words, aim of the NTA is to ensure that there is more treatment, better treatment and fairer treatment available to all those who need it. This organisation has been established to survey the development of drug treatment services at a national level. Parallel structures have been established with the Scottish Executive and the Welsh and Northern Ireland Assemblies. The NTA describes its functions in its own words as follows:
• Exists to serve the needs of drug treatment service users, their unpaid carers and the communities in which they live
• Will seek to work in partnership with service providers, commissioners of treatment services and communities to improve the quality and effectiveness of treatment
• Will be open, accessible and responsive to the needs of all the diverse communities living in England
• Will be independent, rigorous and fair
• Will operate according to the best available evidence
• Will apply expectations of continuous improvement to their own operations
• Will communicate in a clear and timely way with stakeholders.
In order to improve treatment for drug misuse in England, the NTA concentrates on:
• Ensuring that tax payers’ money is spent on expanding and running effective, well-managed and appropriate treatment. That means improving of knowledge of each area’s need for drug treatment and how to plan and pay for services that meet that need.
• Promoting best practice in drug treatment. That means giving drug workers information and guidance on what approaches to treatment are most effective.
• Improving the performance and availability of drug treatment workers. That means developing training, career development and recruitment opportunities for existing and potential employees.
• Improving the commissioning of drug treatment services. The aim is to ensure that the National Pooled Treatment Budget is spent to best effect, on treatment that really works and that meets the needs of local people.
Promoting best practice in drug treatment
Treatment should be based on evidence. Therefore the institution summarises existing research, carries out own studies and tests new approaches to treatment in order to identify what works, and then publishes the findings and recommendations. In order to ensure equally high standards of treatment across the country, the NTA has developed a set of basic national standards that all drug treatment services should meet. Such standards “Models of Care for the Treatment of Adult Drug Misusers” define the national framework for the commissioning of adult substance misuse treatment.
For improving the performance of treatment services and staff, the NTA is working with key organisations and colleges to improve training for new and existing staff. NTA works in a network with other parts of the health service, including public health and social services, as well as criminal justice agencies including probation and prison services. Additionally NTA works in partnership with those organisations that also strive to tackle the harms associated with addiction.
The important national and regional partners for NTA to develop standards and disseminate good practice are:
• Home Office: The Drug Strategy Directorate within the Home Office is responsible for the Government’s drugs strategy. Close cooperation exists with other departments within the Home Office, including the key criminal justice agencies - probation, police, prison services and youth justice board, to develop policies and approaches to improving treatment, particularly for offenders.
• Healthcare Commission: NTA is working with the Healthcare Commission to develop standards and inspection procedures for drug treatment services
• Royal colleges and training organisations: Cooperation exists with the royal colleges of GPs and psychiatrists, and the British Psychological Society to increase the level of training on drug misuse available in their courses.
• Academic institutions and researchers: NTA works with universities and researchers to identify best practice in drug treatment. In some instances, this involves paying researchers to carry out work on their behalf.
• Government office drug teams: Based in the nine government offices for the regions, these teams are responsible for implementing the national drugs strategy at regional level.
• Drug action teams (DATs): The local consortia responsible for planning and commissioning activities to tackle drug misuse, including drug treatment.
• Drug treatment providers: Drug treatment is provided by NHS organisations (e.g. at hospitals, special clinics and at GP surgeries) and by voluntary organisations and charities. NTA regional managers work closely with the staff of these services in order to improve treatment and share knowledge of what works.
• Service user and carer groups: Drug treatment service users and their carers have developed their own support networks in many areas, and are also represented on many DAT discussion groups. NTA regional managers encourage this involvement, and actively support and consult these groups.
The National Treatment Agency for Substance Misuse (NTA) on behalf of the Department of Health and devolved administrations published an updated version of Drug Misuse and Dependence – UK Guidelines on Clinical Management (28/9/07). The new Clinical Guidelines are based upon the previous evidence-based and wellestablished Clinical Guidelines but reflect some of the considerable changes that have occurred in drug treatment over the past eight years. The latest Clinical Guidelines also reflect the recent suite of guidance from the National Institute for Health and Clinical Excellence (NICE).
Example for a NTA guideline: „Clinical Guidance“ for „Prescribing“
On the website of the NTA there is a link to “work areas” and among there is a further link to „Clinical Guidance“
This website offers „pharmaceutical guidance“ and „prescribing“ with downloads for
• „Best practice guidance for commissioners and providers of pharmaceutical services for drug users“ and
• „Prescribing services for drug misuse“ containing the key findings and recommendations of the NTA’s expert prescribing group on: „The evidence base for the pharmacological treatment of drug misuse, recommended guiding principles of
an effective prescribing regime and recommended components of an effective prescribing service“.
Additionally in this area further links to clinical guidelines and an evidence report are available. Especially there is the link to the „National Institute for Health and Clinical Excellence (NICE)“. This institute has produced „technology appraisals“ on:
• “Methadone and buprenorphine for managing opioid dependence”
• “Naltrexone for the management of opioid dependence”.
For the issue of „substitution treatment“ all levels of knowledge for planning, guidance, and guidelines are available. Also corresponding links to research and evidence reports are presented.
In Summary: The NTA-platform for drug treatment shows an exemplary answer to basic questions of “information dissemination on treatment know-how (scientific evidence) and on good practice”:
• Delivery of guidance, standards, guidelines for all areas of drug treatment and settings of interventions
• Preparation of material for different levels of the decision process on treatment planning and carrying out
• The systematic link to different areas of research: monitoring, epidemiology, evaluation, evidence reports, systematic reviews.
„Treatment Improvement Protocols“ (TIP) and „Treatment improvement exchange“
(TIE) of the Centre for Substance Abuse Treatment (CSAT) in USA
The TIPs and TIEs are carried out by the Centre for Substance Abuse Treatment (CSAT)31. CSAT is a department in the Substance Abuse and Mental Health Services Administration (SAMHSA) which is the leading Federal agency addressing substance abuse and mental health services in the United States. SAMHSA was established as a services agency in 1992. Its resources and programmes are designed to promote the expansion of service capacity and to improve the infrastructure to address existing paps in prevention and treatment.
One main goal is the improvement of service quality by a) improving outcomes of programmes as measured by the SAMHSA National Outcome Measures (NOMs) and b) by contributing to the documentation of effective practices through the National Registry for Effective Programmes and Practices (see below).
The effectiveness goal is also supported by Best Practices Planning and Implementation programmes and Science to Services programmes. Success in ‘Science to Services’ requires adequate documentation and dissemination of potential service improvements to the field, and transfer of information about practices that need further research.
For the question of “Best Practice Development and Exchange” the following processes are of particular importance.
“Treatment improvement protocol” (TIP) and the TIP development process
The Treatment Improvement Protocols (TIPs) are best practice guidelines for the treatment of substance abuse. CSAT's Office of Evaluation, Scientific Analysis, and Synthesis draw on the experience and knowledge of clinical, research and administrative experts to produce the TIPs, which are distributed to facilities and individuals across the country.
The TIPs Development Process includes an Editorial Advisory Board. This is a distinguished group of substance abuse experts and professionals in primary care, mental health, and social services. The State Alcohol and Other Drug Abuse Directors generate topics for the TIPs based on the practices current needs for information and guidance.
After selecting a topic, CSAT invites staff from pertinent Federal agencies and national organisations to a Resource Panel that recommends specific areas of focus as well as resources that should be considered in developing the content for the TIP. Soon after that a consensus panel is held, non-federal experts who are familiar with the topic and are nominated by their peers participate in panel discussions over five days. The information and recommendations on which they reach consensus form the foundation of the TIP. The members of each Consensus Panel represent substance abuse treatment programmes, hospitals, community health centres, counselling programmes, criminal justice and child welfare agencies, and private practitioners. A panel chair ensures that the guidelines mirror the results of the group's collaboration.
As an example the link to the “Treatment improvement Protocols” (www.tie.samhsa.gov/Externals/tips.html) is presented under the heading of „Treatment Improvement Exchange“ (TIE) (see next part). Up to now (December 2007) 45 TIPs are available for different areas of drug treatment interventions. Newer TIPs are revisions of the older ones and replace them against the background of new evidence. Exemplarily the last five protocols are listed:
• TIP 45: Detoxification and Substance Abuse Treatment – This TIP provides clinicians with the latest information on detoxification: the physiology of withdrawal, pharmacologic advances in the management of withdrawal, patient placement procedures and managing detoxification services within comprehensive systems of care.
• TIP 44: Substance Abuse Treatment for Adults in the Criminal Justice System – This TIP presents clinical guidelines to help substance abuse treatment counsellors addressing issues that arise from their clients’ status in the criminal justice system. In addition, it will aid personnel in the criminal justice system in understanding and addressing the challenges of working with offenders with substance use disorders.
• TIP 43: Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs – this TIP provides treatment providers, physicians and other medical personnel with the latest information on medication-assisted treatment for people addicted to opiates. The TIP emphasises the importance of supportive services such as counselling, mental health and other medical services, and vocational rehabilitation in facilitating recovery for patients receiving mediation-assisted treatment.
• TIP 42: Substance Abuse Treatment for Persons With Co-Occurring Disorders – the TIP provides information about new developments in the rapidly growing field of cooccurring substance use and mental disorders, and captures the state of the art in the treatment of people with co-occurring disorders.
• TIP 41: Substance Abuse Treatment: Group Therapy – this TIP contains detailed information about group therapy modalities.
The TIPs can be regarded as a combination of what in Europe is known as “quality standards32” for the implementation of a drug treatment service and “guidelines33” for assisting decisions of professionals in the treatment process.
The TIPs are living documents on “good practice” that are periodically revised in a consensus process based on new knowledge and experience.
Organising Treatment exchange
The Treatment Improvement Exchange (TIE) is a resource sponsored by the Division of State and Community Assistance of the Centre for Substance Abuse Treatment to provide information exchange between CSAT staff and State and local alcohol and substance abuse agencies.
Register of “Evidence based Programmes and Practice”
The National Registry of Evidence-based Programmes and Practices (NREPP) is an online registry of mental health and substance abuse interventions that have been reviewed and rated by independent reviewers. The purpose of this registry is to assist the public in identifying approaches to prevent and treat mental and/or substance use disorders that have been scientifically tested and that can be readily disseminated to the field. NREPP is one way that SAMHSA is working to improve access to information on tested interventions and thereby reduces the lag time between the creation of scientific knowledge and its practical application in the field. NREPP is a voluntary, self-nominating system in which intervention developers are elected to participate. As the “Best Practice Portal” is also a task of the EMCDDA the provided information and the review process are a matter of interest. NREPP publishes a report called an intervention summary on its website for every intervention that has been reviewed. Each intervention summary includes:
• Descriptive information about the intervention and its targeted outcomes
• Quality of research and readiness for dissemination ratings
• A list of studies and materials submitted for review
• Contact information for the intervention developer
Before an intervention will be considered for review, documentation must be provided that shows it meets the following minimum requirements:
1. The intervention demonstrates one or more positive outcomes (p?.05) in mental health and/or substance use behaviour among individuals, communities, or populations.
2. Intervention results have been published in a peer-reviewed publication or documented in a comprehensive evaluation report.
3. Documentation (e.g. manuals, process guides, tools, training materials) of the intervention and its proper implementation is available to the public to facilitate dissemination.
Reported results of an intervention are evaluated independently by different reviewers according to the Criteria for Rating Quality of Research using a defined number of criteria.
An important target of SAMHSA National Registry for Evidence-Based Programs and Practices is to increase the number of candidate programmes applying by 12 (6 each year) from a 2005 baseline of 18.
In addition to these processes the CSAT is linked to a “Co-Occurring Centre for Excellence“ and Technical Assistance Publications (TAPs). TAPs are publications, manuals, and guides developed by CSAT to offer practical responses to emerging issues and concerns in the field of substance abuse treatment. Policy makers, providers or professionals can find for example the evaluated intervention for „substance abuse treatment“, for „adults“ in an urban setting on the following website: In case of the example „Brief Marijuana Dependence Counselling“ (May 2007) the abstract provides a short description: „Brief Marijuana Dependence Counselling (BMDC) is a 12-week intervention designed to treat adults with a diagnosis of cannabis dependence. Using a client-centered approach, BMDC targets a reduction in the frequency of marijuana use, thereby reducing marijuana-related problems and symptoms. BMDC is based on the research protocol used by counselors in the Center for Substance Abuse Treatment's Marijuana Treatment Project conducted in the late 1990s.“ The respective treatment manual offers guidelines for counsellors that can be downloaded directly.
Additionally the CSAT platform delivers assistance to other decisions as to “Peer-to-Peer” support or a “locator” for services:
• “Recovery Community Services Program” (RCSP); Peer-to-peer recovery support services help people to initiate and sustain recovery from alcohol and drug use disorders. Some RCSP grant projects also offer support to family members of people needing, seeking, or in recovery.
• “Substance Abuse Treatment Facility Locator” – This directory of drug and alcohol treatment programmes shows the location of facilities around the country that treat alcoholism, alcohol abuse and drug abuse problems. The Locator includes more than 11,000 addiction treatment programmes, including residential treatment centres, outpatient treatment programmes, and hospital inpatient programmes for drug addiction and alcoholism. Listings include treatment programmes for marijuana, cocaine, and heroin addiction, as well as drug and alcohol treatment programmes for adolescents, and adults.
All in all the different platforms provides under the umbrella of the “Centre for Substance Abuse Treatment” (CSAT) and their systematic links to different areas of research, preparation, dissemination and implementation of “good practice” deliver essential hints for improvement in the Member States and at European level.
18.5 The future of the exchange of good practice in drug treatment in Europe
Compared to the situation in the year 2005, when the proposal for this work package has been prepared, the situation in Europe has changed. The main developments are:
• The general decision about the location for the exchange platform in the field of responsibility of the EMCDDA has been made.
• This platform has a general concept (see “Best Practice Platform” above).
• This platform has already started.
Consequently recommendations for further developments and improvement of best practice exchange have to consider the new developments. To contribute to the improvement of best practice the following aspects should be the main focus:
• The different areas of the implemented portal have to be filled with contents. For some areas this mainly demands the collection of information while in other areas there is a weak substructure at all.
• The quality of the delivered products have to be enhances and the procedures for quality assurance have to be supported.
• The production of evidence reports, guidelines for implementation and manuals for interventions in Europe needs to be strengthened.
Strengthen evidence based culture and infrastructure in Member States
Support in establishing evidence-based cultures und qualifications of knowledge infrastructure in drug treatment at the level of Member States is the indispensable basis for a new level in development and exchange of good practice. In this respect there are different areas where the Member States can benefit from advice and support from the EU.
Main issues are the implementation of authorised institutions/platforms for the coordination and dissemination, as well as for quality assurance and guideline development. A further issue is the coordination with existing research (Drug Research, Health Care, and Clinical Excellence) institutions and networks. Based on the investigation of the “quality system” and the transfer of drug treatment know-how in Member States it can be summarised that quality assurance systems have been developed in the majority of the Member States. However, up to now the main components for knowledge transfer and best practice transfer are only partly implemented in the Member States. This is especially the case for
• evaluation and research,
• reviews/evidence reports,
• implementation of a systematic procedure for producing and controlling new protocols, consensus process, and
• for the development of guidelines.
The area of evidence-based development of guidelines and transfer of good practice in drug treatment must be reinforced and referring to the corresponding tasks of the EU drug action plan.
Adjuvant network for identification and exchange of good practice
In addition to existing activities and the developments within the Pompidou Group and the “Best Practice Portal” of the EMCDDA, in Europe a self-contained network is required in the field of drug treatment, prevention and policy action complementary to and in close cooperation with the EUnetHTA and the G-I-N. The organisational frame should be a net of national/regional official agencies, public bodies, MoHs, research institutions, and international organisations/networks. This net should have the similar priority tasks as the HTA Net and the G-I-N in general:
• Procedures (defined and standardised elements of guidance for obtaining evidence and best practice) which have only to be adopted.
• Priority areas for issues of evidence reviews, research, identification and preparation of good practice as to drug treatment interventions.
• A workplan to realise the main objectives in responsibility of national institutes of the Member States (main areas of drug treatment interventions – evidence, implementation guidance, manuals).
The main reason for the necessity of a distinct net is that the currently initiated HTA (and also the G-I-N) process refers first of all to the central health topics of medical care. Issues concerning psychosocial interventions and drug treatment (appraisal of available evidence, development of guidelines and models of “good practice” and its transfer) are not of first priority in these networks and therefore delayed -this is the experience of the last years.
Important additional aspect of the European exchange platform
Evidence reports are of important value but they should be completed by „treatment improvement guidance“ (the main examples are the “treatment improvement protocols” to all areas of intervention in the US) or guidelines. This requires the implementation of consensus building processes (protocol, procedure) for additional or special areas of drug treatment as well as for revision of existing protocols. The integration of best practice examples (based on criteria) should be broadened by an online registry of mental health and substance abuse interventions which is reviewed and rated by independent reviewers (Example: The National Registry of Evidence-based Programmes and Practices (NREPP) in the US). Such a procedure has been started with the “Best Practice Portal” on basis of the EDDRA database. However, it still has a substantial lack as regards the scientific evaluation of the interventions and the selection criteria and available resources.
20 The EU drugs action plan (2005-2008), www.emcdda.europa.eu/index.cfm?nNodeID=10360
21 „While reaffirming the EMCDDA's main purpose as to provide EU-Member States with 'factual, objective, reliable and comparable information at European level concerning drugs and drug addiction and their consequences', the new regulation broadens the scope of the Centre's tasks.“ www.emcdda.europa.eu/html.cfm/index27868EN.html
22 The European network for health Technology Assessment –
23 World Health Organization – the Health Evidence Network (HEN) –
24 See
25
26 These reviews aim at assessing the available evidence for the efficacy of measures for the prevention of substance use drawing on systematic reviews, unsystematic reviews, meta-analyses and individual studies (mainly randomised controlled trials).
27 This is the first area the EMCDDA had focus on (started in 2008).
28
29 Factsheets in english language see: www.ggzkennisnet.nl/ggz/publicaties/raadplegen.asp
30 National Treatment Agency (NTA) –
31 Centre for Substance Abuse Treatment (CSAT) –
32 Quality standards as generally accepted principles or set of rules for the best/most appropriate way to implement interventions. Frequently they refer to structural (formal) aspects of quality assurance such as environment and staff composition. However they may also refer to process aspects such as adequacy of content, process of the intervention or evaluation processes.
33 Guidelines are systematically developed statements to assist practitioners and patient decisions about appropriate interventions for specific circumstances.
| < Prev | Next > |
|---|












