Chapter 14 Criminal justice approaches to harm reduction in Europe
| Reports - EMCDDA Harm Reduction |
Drug Abuse
Chapter 14 Criminal justice approaches to harm reduction in Europe
Alex Stevens, Heino Stöver and Cinzia Brentari
Abstract
This chapter reviews the spread of harm reduction services in European criminal justice
systems, and their evaluation. It begins with a discussion of the tensions and contradictions
inherent in providing harm reduction services (which may accept continued drug use) in
criminal justice settings (that do not). It then draws on research carried out for the
Connections project, for its predecessor the European Network on Drug and Infections
Prevention in Prisons and on the information gathered by the European Monitoring Centre
for Drugs and Drug Addiction. It examines services such as needle and syringe exchange,
opiate substitution and distribution of condoms and disinfectants in prisons. It also
examines harm reduction services that have been developed in the context of police
custody, and in the attempt to provide through-care and aftercare to drug users who pass
through the criminal justice system. The chapter concludes that the tensions between harm
reduction and criminal justice aims can be overcome in providing effective services to
reduce drug-related harms.
Keywords: criminal justice systems, harm reduction, prison, decriminalisation, syringe
exchange, opioid substitution treatment, arrest-referral.
Introduction
Harm reduction is often seen as conflicting with the use of law enforcement to reduce drug
use, but there are ways in which policies and practice can develop in order to reduce harms
related to drugs within the criminal justice system. The principle of harm reduction may also
be applied to law enforcement itself. Drug prohibition can inadvertently increase the
harmfulness of drug use as it means that users rely on illicit forms of supply and consume
drugs of unknown purity and quality in a risky manner. It also creates artificially high prices,
which stimulate acquisitive crime and facilitate corruption and violence. Given that drug
markets cannot be eliminated, but may operate in ways that are more or less socially
harmful, the key questions for law enforcement become: what sort of markets do we least
dislike and how can we adjust the control mix so as to push markets in the least harmful
direction? In this chapter, we leave aside more detailed discussion of the wider impact of
drug law enforcement or criminalisation on societal levels of drug-related harm. We focus
instead on the provision of services that aim to reduce harms done to drug users within the
criminal justice system.
Many of the people who are caught up in the criminal justice system are highly exposed to
drug-related harms (EMCDDA, 2009a; Singleton et al., 1997; Stöver, 2001; Rotily et al.,
2001; Møller et al., 2007; Stöver et al., 2008a; Dolan et al., 2007). These people do not lose
their right to adequate and effective healthcare when they enter the criminal justice system
(Carter and Hall, 2010). The ideal criminal justice system would therefore protect their health
by offering the full range of healthcare approaches. Some European systems have been
moving closer, in various ways, to achieving this, and we describe some of these
developments in this chapter. We will examine how measures such as opioid substitution
treatment (OST), needle and syringe exchange, and the provision of disinfectants and
condoms have worked in prison contexts. We will look at issues of through-care and
aftercare and we will explore how processes that follow arrest can divert drug users into
treatment. Before looking at specific harm reduction measures we provide a short discussion
of the inherent tensions between controlling drugs through the criminal law and efforts to
reduce harms to drug users.
Tensions between law enforcement and harm reduction
There are at least two contradictions that hinder the effort to reduce harm through the
criminal justice system. The first is the fact that criminal justice systems themselves produce
harms. Of course, the criminal justice system also produces benefits to the extent that it
protects people from crime and insecurity. But arrests, fines, community penalties,
imprisonment and parole all infringe on individual freedoms and pleasures. The special pains
of imprisonment have been a particular focus of criminological research (Sykes 1958;
Mathiesen, 2006). The idea that these pains are justified by the need to reduce crime is
challenged by the lack of evidence for the effectiveness of imprisonment, the most painful
form of criminal justice intervention currently used in Europe (Tonry, 2004; Gendreau et al.,
1999). It is well known, for example, that there is little relationship between imprisonment and
crime rates (Kovandzic and Vieraitis, 2006; Reiner, 2000). Countries do not use prison as a
direct, rational measure to reduce crime. Rather, they choose — through a complex process
of ideological, moral, political and juridical negotiation — the level of pain that they are
willing to inflict on their citizens (Christie 1982). If we choose the level of harm that we inflict,
we can also choose to reduce it.
The second contradiction in pursuing harm reduction in the criminal justice system is that
between the pursuit of abstinence and the acknowledgement of continuing drug use.
Countries are obliged, through the UN drug conventions, to prohibit and to penalise the
possession of certain substances. The criminal justice system is the process that puts these
obligations into practice. It is very difficult for the same system to acknowledge that the
people under its control continue to defy the law. Until the mid-1990s, for example, it
was common for prison governors to deny that drug use was going on within their walls
(Duke, 2003). More recently, it has been suggested by Phillip Bean (2008) that treatment
agencies working with the criminal justice system should expect to subordinate their aims
to those of the criminal justice agencies. Harm reduction approaches have traditionally
been developed to meet the needs of people who continue to use illicit drugs, and
therefore do not fit with the prescription that people under penal control should abstain.
Some parts of the criminal justice system and some countries appear to negotiate this
conflict more easily than others. This may be due to the different perceptions of the ideal
goal of abstinence. Within the prison system, for example, abstinence has a relatively
high value, because it fits with the prison’s goal of incapacitating the prisoner from
committing further crimes (e.g. drug purchase and possession). Probation services, with a
greater focus on rehabilitation and relatively less control of the person’s behaviour, seem
to have less emphasis on absolute abstention, at least in Europe. In the United States,
drug use while on probation often leads to imprisonment. It is more often tolerated in
European probation systems, as long as no other offences are committed (Stevens,
forthcoming).
So how do we deal with these contradictions? First, it seems axiomatic that the best way to
reduce the amount of drug-related harm that occurs inside the criminal justice system is to
reduce the number of drug users who enter it. Drug users cannot cause harm (or be
harmed) in criminal justice settings if they are not actually in these settings. The number of
drug users in criminal justice settings can be reduced through decriminalisation of drugs,
which means that no drug users enter the criminal justice system for possession offences
(though decriminalisation of drugs would not necessarily reduce the number of drug users
who enter the system for other offences, which could be reduced by developing diversion
or alternative sanctions) (Stevens, forthcoming). Different European countries have tried
various forms of decriminalisation. They include the Netherlands’ expedient nonprosecution
of cannabis supply at the retail level, as well as the non-criminal offences of
personal drug use in the Czech Republic, Estonia, Italy, Spain and suspension of
prosecution of personal use offences in Germany and Austria.
The most comprehensive process of decriminalisation so far has occurred in Portugal.
From July 2001 people who are found by the Portuguese police to be in possession of
fewer than ten days’ personal supply of any drug have not been arrested, though the
drug is still confiscated. They have instead been referred to regional drug dissuasion
committees, which have the option of imposing warnings, fines, administrative sanctions
(such as taking away driving or firearms licences), or — in the case of dependent users
— referring them to treatment. Since decriminalisation, and the simultaneous expansion
of prevention, treatment and harm reduction services, there have been dramatic
reductions in drug-related deaths and HIV. Rates of drug use seem to have fallen among
children, but risen slightly in adults, in line with pan-European trends. The respective
roles of decriminalisation and the simultaneous expansion of drug treatment in producing
these changes can be debated (IDT, 2007; IDT, 2005; Hughes and Stevens, 2007;
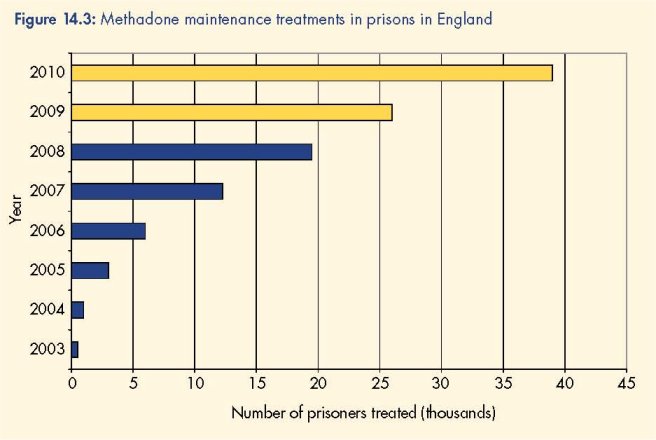
Greenwald, 2009). But Figure 14.1 shows clearly that decriminalisation reduced the use
of imprisonment for drug offences and led to an overall reduction in the prison
population (IDT, 2006, Table 62). This reduction has also been accompanied by
substantial reductions in the number of people using drugs and living with HIV within
Portuguese prisons (Torres et al., 2009).
The second contradiction is just a more extreme form of the long-standing argument that
harm reduction conflicts with the goal — still subscribed to by all UN members (ECOSOC,
2009) — of eliminating illicit drug use. Over time, there has been a gradual acceptance
that harm reduction measures do not prevent people from achieving abstinence, but
rather protect the health of people who will continue to use drugs, whether or not they
have the means to protect their health. This acceptance has been supported by decades
of evaluative research on harm reduction measures outside the criminal justice system,
including opiate substitution treatment (using methadone, buprenorphine or heroin itself)
and needle and syringe exchange programmes (Hunt, 2003; Ritter and Cameron, 2005;
Tilson et al., 2007; Kimber et al., 2010). As evidence develops on the use of such
measures within the criminal justice system, we could expect that resistance to harm
reduction within the criminal justice system will also subside. But we should not be too
optimistic. The negotiations at the high level segment of the Commission on Narcotic
Drugs in Vienna in March 2009 showed that resistance to harm reduction remains strong,
even outside the criminal justice system. A glimmer of hope from that meeting can be
perceived, if we look hard enough, in the commitment to provide treatment and ‘related
support services ... on a non-discriminatory basis, including in detention facilities’
(ECOSOC, 2009).
Harm reduction in the criminal justice system
Our exploration of existing harm reduction services in criminal justice systems starts in the
place where drug-related harms of the criminal justice system are most acute: prisons.
In a report on the implementation of the European Council Recommendation (of 18 June
2003 (1)) on the prevention and reduction of health-related harm associated with drug
dependence (2) it was stated that a policy to provide drug users in prisons with services
that are similar to those available to drug users outside prisons exists in 20 EU Member
States and was about to be introduced in four countries (van der Gouwe et al., 2006).
However, recent European monitoring data show that that the implementation of harm
reduction programmes is quite heterogeneous in European prisons (EMCDDA, 2009a).
Availability and accessibility of many key harm reduction measures in prisons lag far
behind the availability and accessibility of these interventions in the community outside
prisons (EMCDDA, 2009b).
(1) http://europa.eu.int/eur-lex/pri/en/oj/dat/2003/l_165/l_16520030703en00310033.pdf
Illustrating this gap most vividly is the provision — or lack thereof — of needle and syringe
programmes (NSP), currently only implemented in five EU countries (EMCDDA, 2009c). The
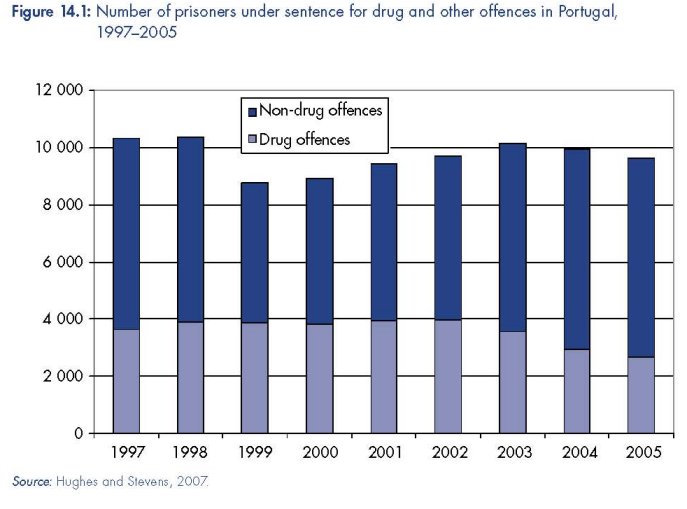
availability of opioid substitution treatment (OST) in prisons is low compared to the level of
OST provision in the community in most European countries (EMCDDA, 2009d; see Figure
14.2). These findings support an earlier statement from the European Commission that:
Harm reduction interventions in prisons within the European Union are still not in accordance with
the principle of equivalence adopted by UN General Assembly, UNAIDS/WHO and UNODC,
which calls for equivalence between health services and care (including harm reduction) inside
prison and those available to society outside prison. Therefore, it is important for the countries to
adapt prison-based harm reduction activities to meet the needs of drug users and staff in prisons
and improve access to services.
(European Commission, 2007, conclusion 5).
These findings also echo a 2008 WHO Regional Office for Europe report that monitored
State progress in achieving Dublin Declaration goals. The Dublin Declaration commits the
signatory States to take 33 specific actions — and in some cases meet specific targets — to
address the HIV prevention, care, treatment and support situation across the region. The
report found that, of the 53 signatory countries, condoms were available in prisons in only
18, syringe exchange programmes available in six and substitution treatment available in 17
(Matic et al., 2008). A more recent review (in 2009) by the International Harm Reduction
Association (IHRA) found the situation has only marginally improved, with nine countries (out
of 46) in Europe and Central Asia having syringe exchange in prisons and 28 substitution
treatment (Cook, 2009; see also Cook et al., 2010).
Calls for an urgent and comprehensive response to addressing health risks within prison
settings, including harm reduction measures (WHO Regional Office for Europe, 2005) are
not new, and have been highlighted in international reports and policy documents spanning
two decades (Parliamentary Assembly of the Council of Europe, 1988; UNODC et al., 2006;
WHO, 1993; Matic et al., 2008). However, despite existing recommendations, guidelines and
commitments made by governments and many others (Lines, 2008), only very few countries
within the European region have come close to achieving the goals set out (Cook, 2009).
There are four key harm reduction tools for the prison setting. We describe each of these,
including an example of best practice, below.
(2) http://ec.europa.eu/health/ph_determinants/life_style/drug/drug_rec_en.htm
Notes:
This figure is available at: http://www.emcdda.europa.eu/stats09/hsrfig2.
Comments:
Data were not available for Sweden.
Rating scales:
Prison: expert rating of the availability of OST programmes in prisons in the country (and does not reflect level of
OST provision in prison):
• Full: substitution/maintenance treatment exists in nearly all prisons.
• Extensive: exists in a majority of prisons but not in nearly all of them.
• Limited: exists in more than a few prisons but not in a majority of them.
• Rare: exists in just a few prisons.
Community: expert rating of the level of provision of OST in the community, in relation to the needs of target group
problem opioid users:
• Full: nearly all problem opioid users (POUs) in need would obtain OST.
• Extensive: a majority but not nearly all POUs in need would obtain OST.
• Limited: more than a few but not a majority of POUs in need would obtain OST.
• Rare: just a few POUs in need would obtain OST.
Sources: EMCDDA, 2009d. Structured questionnaire on ‘treatment programmes’ (SQ27/P1), submitted by NFPs in 2008.
Data for Malta is from DG Health and Consumer Protection, ‘Final report on prevention, treatment, and harm reduction
services in prison, on reintegration services on release from prison and methods to monitor/analyse drug use among
prisoners’, SANCO/2006/C4/02.
Needle and syringe exchange programmes in prisons
A position paper of the United Nations system identifies NSP as one component of ‘a
comprehensive package for HIV prevention among drug abusers’ (Commission on Narcotic
Drugs, 2002). In prisons, NSPs have been operating successfully for more than 15 years. A
meta-analysis (based on 11 evaluations of the implementation of prison-based NSPs)
revealed that none of the fears often associated with planned NSPs occurred in any project:
syringe distribution was followed neither by an increase in drug intake nor in administration
by injection. Syringes were not misused as weapons against staff or other prisoners, and
disposal of used syringes was uncomplicated. Sharing of syringes among drug users
disappeared almost completely or was apparent in very few cases. These studies
demonstrate both the feasibility, safety and efficacy of harm reduction including NSP in
prison settings (Meyenberg et al., 1999; Stöver and Nelles 2003).
At present, NSPs have been established in prisons in nine countries worldwide (Lines et al.,
2006), including six countries in Europe. Coverage of the national prison systems is, however,
variable. In Spain, implementation of needle and syringe exchange is authorised in all
prisons (see box below) and in 2006, programmes existed in 37 prisons (Acín García,
2008). In Switzerland, NSPs are available in eight of 120 prisons, and in Germany,
Luxembourg, Romania and Portugal such programmes operate in one or two prisons. Other
countries, including the United Kingdom (Scotland), are considering the implementation of
pilot projects (EMCDDA, 2009a; Lines et al., 2006). A review published in 2007 stated:
Prison NSPs have been implemented in both men’s and women’s prisons, in institutions of varying
sizes, in both civilian and military systems, in institutions that house prisoners in individual cells
and those that house them in barracks, in institutions with different security ratings, and in different
forms of custody (remand and sentenced, open and closed).
(Stöver et al., 2009, p. 83)
|
Prison-based needle and syringe exchange programmes in Spain Spanish prisons implement needle and syringe programmes (NSPs) via negotiated protocols • a Commission is created, with the Director and vice directors (including sanitary vice reducing potential harm to prison staff (Ministry of Labour and Social Security, 2002). |
Opioid substitution treatment
While opioid substitution treatment (OST) has become standard practice in community drug
treatment services in many European countries (EMCDDA, 2009a), the implementation of
OST in custodial settings in most European countries is still lagging behind the availability
and quality of the treatment provision in the community (Kastelic et al., 2008; EMCDDA,
2009d).
Studies have indicated that OST initiated in the community is most likely to be discontinued in
prisons (Stöver et al., 2004; Stöver et al., 2006; Michel, 2005; Michel and Maguet, 2003).
This often leads to relapse both inside prisons and immediately after release, often with
severe consequences, as indicated by high mortality rates after release from prisons
(Singelton et al., 2003). Many studies have also shown the benefits of OST for the health and
social stabilisation of opioid-dependent individuals passing through the prison system
(Stallwitz and Stöver 2007; Larney and Dolan, 2009).
Substitution treatment has been widely recognised as an effective treatment for opioid
dependence in the general community (Dolan et al., 1998; Farrell et al., 2001; Larney and
Dolan, 2009; UNODC et al., 2006) and as having crime reducing effects (Lind et al., 2005).
Despite this and the fact that methadone and buprenorphine have been added to the WHO
model list of essential medicines (WHO, 2005), it remains controversial for prisons,
particularly in Eastern European countries where substitution treatment also only exists on a
low level in the community (van der Gouwe et al., 2006). Nevertheless, experience has
clearly shown the benefits of this treatment in prisons (WHO et al., 2007; Heimer et al.,
2005; Stöver et al., 2008b; Stöver and Michels, 2010).
In countries that provide OST in prisons, it is most commonly used for short-term
detoxification, and less frequently as a maintenance treatment (Kastelic et al., 2008). In some
countries, such as Austria, England (see box on p. 387) and Spain, substitution treatment is
provided as standard therapy to many prisoners who began treatment in the community and
are deemed likely to continue it after release (Stöveret al., 2004). In others it is either not
available in prisons at all, although legally possible (Estonia and Lithuania), or only provided
in very rare cases (Sweden). OST treatment that has been started in the community cannot
legally be continued in prisons in Slovakia, Latvia, Cyprus and Greece. New substitution
treatments cannot be initiated in Slovakia, Latvia, Cyprus, Greece, Portugal, Finland and
Estonia (EMCDDA, 2009a).
Acknowledgement that the benefits of substitution treatment in the community might also
apply to the prison setting has taken years. The sources of the controversy — and the slow
and patchy manner of the intervention’s implementation thus far — can be traced first to the
prisons’ general failure to provide adequate healthcare, with limited resources for
populations with high concentrations of poor physical and mental health (Møller et al., 2007;
Bertrand and Niveau, 2006). Second, due to the parallel prison healthcare system (separate
to the national health services in most countries), responsibility for a prisoner’s medical
treatment is often transferred to healthcare providers only after that prisoner has been
released. Third, the ethos of coercion and incapacitation manifests itself in a strict abstinence
based approach to drug use. Therefore, while opioid-dependent individuals in the community
may be treated as patients and receive substitution treatment, in prison they continue to be
treated as prisoners who are supposed to remain drug free. This double standard leads to
frequent interruptions in treatment and inconsistency in dosages, especially as many opioid
users spend substantial periods of time incarcerated.
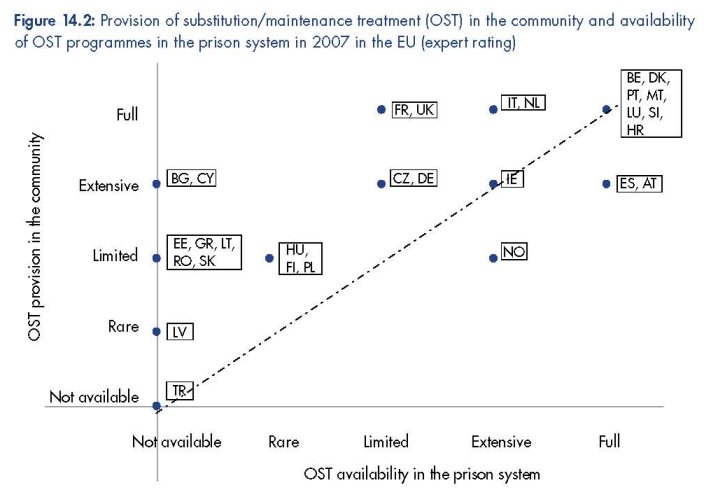
The number of methadone maintenance (OST) treatments started in prisons in England has increased from 700 in 2003 (1) to 19 450 for the year 2008. All 130 adult prisons in the country are now funded to provide OST. Approximately 26 000 treatments are anticipated for 2009, rising to 39 000 for the year 2010 (Marteau and Stöver, 2010).
The massive expansion of OST in prisons is the result of: a shift of responsibility for prison This example shows that the Integrated Drug Treatment System (IDTS) has been welcomed by (1) Refers to the fiscal year 2003–04 which runs from 1 March 2003 until end February 2004. All dates cited in this box |
Evidence shows that methadone maintenance treatment (MMT, the most studied form of
pharmacological drug treatment) can reduce risk behaviour in penal institutions, such as
reduced frequency of illicit drug use in prison and reduced involvement in the prison drug
trade (Dolan et al., 1998; Kimber et al., 2010). Studies have also demonstrated that
methadone maintenance treatment provision in a prison healthcare setting can be effective in
reducing heroin use, drug injection and syringe sharing among incarcerated heroin users
(Stöver and Marteau, 2010). A sufficiently high dosage also seems to be important for
improving retention rate, which helps in the provision of additional healthcare services (Dolan
et al., 2002).
There is evidence that continued MMT in prison has a beneficial impact on transferring
prisoners into drug treatment after release. The initiation of MMT in prisons also contributes to a
significant reduction in serious drug charges and in behaviour related to activities in the drug
subculture. Offenders participating in MMT also had lower readmission rates and were
readmitted at a slower rate than non-MMT patients. For example, a 2001 evaluative study of
the methadone programme of the Correctional Service of Canada (CSC) concluded that
participation in methadone programmes had positive post-release outcomes. The study found
that opiate users accessing MMT during their incarceration were less likely to be readmitted to
prison following their release — and were less likely to have committed new offences — than
were those not accessing methadone. These findings have been supported by a more recent
randomised trial from the United States. It showed that prisoners who started methadone
treatment before release and continued after it were significantly more likely to stay away from
illicit drugs in the first year after release. Their outcomes were better than those achieved by
similar prisoners who received only counselling in the prison, than if they were transferred to
methadone programmes on release (Kinlock et al. 2009; Stöver and Marteau 2010; Stöver and
Michels, 2010).
Studies have shown that prison staff tend to support the introduction of OST to a higher
degree than they support other harm reduction measures, such as syringe exchange (Allen,
2001). Greater knowledge of substitution programmes is directly associated with more
positive attitudes towards it (McMillan and Lapham, 2005). This suggests that training for
staff on all levels may decrease resistance to substitution programmes and contribute to
patient-oriented, confidential and ethical service delivery. Institutional constraints can also be
overcome by highlighting the benefits of a substitution programme for the prison itself (Stöver
and Marteau, 2010).
Provision of bleach and disinfectants
Many prison systems have adopted programmes that provide disinfectants such as bleach to
prisoners who inject drugs, as a means to clean injecting equipment before re-using it (see
box on p. 389). According to UNAIDS in 1997, the provision of full-strength bleach to
prisoners as a measure had been successfully adopted in prisons in Europe, Australia, Africa,
and Central America (UNAIDS, 1997). The WHO further reported that concerns that bleach
might be used as a weapon proved unfounded, and that this has not happened in any prison
where bleach distribution has been tried (WHO, 2007).
However, disinfection with bleach as a means of HIV prevention is of varying efficiency, and
therefore regarded only as a secondary strategy to syringe exchange programmes (WHO,
2005). The effectiveness of disinfection procedures is also largely dependent upon the
method used. Before 1993, guidelines for syringe cleaning stipulated a method known as the
‘2x2x2’ method. This method involved flushing injecting equipment twice with water, twice
with bleach and twice with water. Research in 1993 raised doubts about the effectiveness of
this method in the decontamination of used injecting equipment, and recommended new
cleaning guidelines where injecting equipment should be soaked in fresh full-strength bleach
(5 % sodium hypochlorite) for a minimum of 30 seconds (Shapshank et al., 1993).
All of these developments further complicate the effective use of bleach and disinfectants in
prison settings, where fear of detection by prison staff and lack of time often means that
hygienic preparation of equipment and drug use happens quickly, and that prisoners will
often not take the time to practise optimal disinfection techniques (WHO, 2005). Furthermore,
bleach is effective in killing the HIV virus, but may be less effective for the hepatitis C virus.
Training drug users to clean syringes with bleach may provide the user with false reassurance
regarding the risk of re-using injecting equipment. Despite these limitations, provision of
disinfectants to prisoners remains an important option to reduce the risk of HIV transmission,
particularly where access to sterile syringes is not available. The Royal College of General
Practitioners concluded that ‘[o]n current evidence it would be difficult to support a policy of
not distributing bleach’ (2007, p. 13).
By August 2001, bleach was provided in 11 of 23 pre-expansion EU prison systems (Stöver et al.,
2004). Disinfectants are also made available to prisoners in Canada, England and Wales, Iran,
Kyrgyzstan, Moldova, Turkmenistan, Switzerland, and some parts of the Russian Federation.
|
Provision of bleach in Austrian prisons
|
Provision of condoms, dental dams, and water-based lubricants
Many prisons globally provide condoms to prisoners as part of their institutional health and
STI prevention policies. This is in keeping with the recommendation of the WHO Guidelines,
‘Since penetrative sexual intercourse occurs in prison, even when prohibited, condoms should
be made available to prisoners throughout their period of detention. They should also be
made available prior to any form of leave or release’ (WHO, 1993
Multiple barriers exist to the use of condoms in many prisons, and there is often poor
knowledge among prisoners of sexual risk behaviour and risk reduction (MacDonald, 2005;
Todts et al., 1997; UNODC et al., 2006). These barriers include prison rape, the social stigma
attached to homosexuality and same-sex activities, and insufficient privacy to enable safer
sex. Furthermore, condoms, dental dams, and water-based lubricants are often theoretically
available but often not easily and discreetly accessible, at least not available on a 24-hour
basis. Prisoners may be reluctant to access safer sex measures for fear of identifying
themselves as engaging in such activities.
Evidence suggests that the provision of condoms is feasible in a wide range of prison
settings (WHO et al., 2007). No prison system enabling condom distribution has reversed
this policy, and none have reported security problems or any major negative
consequences. Research also demonstrates the importance of identifying the factors
shaping resistance among stakeholders and prison officials to introducing harm reduction
measures in custodial settings, including condom distribution (Jürgens et al., 2009; Stöver
et al., 2007). The orientation of ministries of justice, public opinion, and prison system
financial constraints are all factors shaping staff acceptance or resistance to implementing
harm reduction, and it is important to develop tailor-made strategies to address these
(Marteau and Stöver 2010; Stöver et al., 2009).
Through-care and aftercare
Prison may be the place where drug-related harms are most visible and acute, but the vast
majority of prisoners will one day be released. According to Williamson (Williamson, 2006)
the major challenge for prison healthcare is:
to enable continuity of care, within, between, on admission and upon release. Using the prisoner
journey from pre-arrest to post release as a template it will be possible for local health and social
care, and criminal justice communities to better plan continuity of health and social care,
alternatives to imprisonment and long term support services.
(Williamson, 2006, p.5)
Several studies have shown that effective and rapid access to aftercare for drug-using
prisoners is essential to maintain gains made in prison-based treatment (e.g. Zurhold et al.,
2005; Inciardi et al., 1997; Department of Health/National Offender Management Service,
2009). Prisoners are marginalised in society and tend to fall into the gaps between care
systems and structures, which find it hard to deal with multiple needs. Care should be taken
to overcome this tendency. From previous studies on recidivism following in-prison
treatment (e.g. Inciardi et al., 1997), maintaining therapeutic relationships initiated in the
prison into the post-release period would be likely to reduce recidivism and improve health
outcomes. Prisons can be places of relative safety and health promotion for prisoners.
Many people slip back into less healthy habits when they leave this structured environment.
The box on p. 391 gives an example of a promising programme that seeks to avoid this
danger.
The ‘Through the Gates’ service
Many prisoners, including a high proportion of those with drug problems, leave prison with no
home to go to. This increases the likelihood that they will continue risky patterns of drug use and
offending. In response to this problem, the St Giles Trust (a non-governmental organisation
based in London) set up the ‘Through the Gates’ service. This service employs a team of
caseworkers (half of whom are themselves ex-offenders) to work with individual prisoners. The
caseworkers go to meet prisoners before they are released in order to assess their housing and
other needs. They then meet the prisoner at the gate of the prison on the day of their release.
The worker accompanies the client to initial meetings with the housing service, with probation
officers and, when necessary, drug treatment services. In the first year of this service, 70 % of
the homeless clients it worked with were successfully placed in temporary or permanent
accommodation. Probation officers reported that the service dramatically increased the chances
of successful resettlement. Some clients reported that it was the first time that they had been
helped to step off the repetitive treadmill of imprisonment, drug use and crime.
The following conclusions were drawn by a multi-country survey of key informants on
aftercare programmes for drug-using prisoners in several European countries (Fox, 2000):
• Aftercare for drug-using prisoners significantly decreases recidivism and relapse rates and
saves lives.
• Interagency cooperation is essential for effective aftercare. Prisons, probation services,
drug treatment agencies and health, employment and social welfare services must join up
to meet the varied needs of drug-using offenders.
• Short-sentence prisoners are the most poorly placed to receive aftercare and most likely to
re-offend. These prisoners need to be fast-tracked into release planning and encouraged
into treatment.
• Ex-prisoners need choice in aftercare. One size does not fit all in drug treatment.
• Aftercare that starts in the last phase of a sentence appears to increase motivation and uptake.
• In aftercare, housing and employment should be partnered with treatment programmes.
Unemployed and homeless ex-prisoners are most likely to relapse and re-offend.
• Drug treatment workers must have access to prisoners during their sentence to encourage
participation in treatment and to plan release.
As the mortality risks due to overdose are most critical in the first week after release
(Singleton et al., 2003; Farrell and Marsden, 2008), all harm reduction measures to prevent
overdose or drug-related infections should be available and accessible.
Earlier stages of the criminal justice system
As with prisons and through-care, the practice and policy of the police with regard to harm
reduction varies throughout Europe, dependent on different legal backgrounds. What can be
found all over Europe is a high level of formal or informal discretion (EMCDDA, 2002). The
police on the street can simply turn a blind eye towards illicit behaviour, or the official
strategy of the police might pro-actively support harm reduction. The basis for these choices
is a growing awareness of the adverse effects of control and custody with regard to the
health of drug users and thus an increasing acknowledgment of all forms of support,
assistance, counselling and treatment for this target group.
The introduction of policing practices that are more open to harm reduction interventions can
contribute substantially to reducing some of the negative consequences of police patrolling,
such as a reluctance to carry syringes and unsafe disposal, hurried and unsafe preparation
of injection, and the potential for police attention to deter drug users from going to treatment
centres (MacDonald et al., 2008). The availability of an injection location that is safe from
police interference is a significant harm reduction measure (Kerr et al., 2008). Drug
consumption rooms are an interesting model of accepting an unlawful behaviour (possession
and consumption of drugs) for the sake of the health of the drug users. In most countries
where they operate, these facilities are not only tolerated, but also demanded and supported
by the police, who also facilitate their use (DeBeck et al., 2008). Furthermore, the police
mostly see drug consumption rooms as a ‘win–win’ situation, as they spend less of their time
dealing with users, and therefore have more resources available to target dealers. In
addition, drug consumption is no longer taking place in the local area and causing public
nuisance, but is taking place under hygienic and less visible circumstances (Stöver, 2002;
Hedrich et al., 2010). The success of drug consumption rooms depends on the police
agreeing not to target drug users within and around them.
There are other examples in Europe of structured combinations of harm reduction and crime
prevention approaches. Arrest referral programmes, which first appeared in the United
Kingdom in the 1980s and were expanded at national level by the Home Office Circular in
1999, are an example of a criminal justice-based programme that can introduce drug users
to treatment and harm reduction services (Seeling et al., 2001). Arrest referral places
specially trained substance use assessment workers in police stations to counsel and refer
drug-using arrestees who voluntarily request assistance with their drug-related problems.
Arrest referral schemes provide an access point for new entrants to services. Data from the
national monitoring programme in England and Wales showed that half (51 %) of all those
screened by an arrest referral worker had never accessed specialist drug treatment services
(Sondhi et al., 2002). This implies that arrest referral is successful in contacting problem drugusing
offenders at an earlier point than they might have otherwise considered using services.
Outcomes of the arrest referral schemes included consistent reductions in drug use and
offending behaviour among problem drug-using offenders who have been engaged in the
scheme (Sondhi et al., 2002).
However, arrest referral often suffers from low rates of retention, with large proportions of the
contacted drug users not going on to contact services (Edmunds et al., 1998). In England and
Wales, the Drug Intervention Programme was supplemented by a system of case
management of drug-using offenders and, since 2005, testing on arrest and required
assessments in order to address this problem. These latter measures enable the police to
require a person arrested for any one of a specific list of offences to undergo a drug test. If
the test is positive for cocaine or heroin, the person can then be ordered to attend an
assessment with a drug treatment worker. The effect of these measures has not been
evaluated. They have brought more drug users into treatment assessments, but many of them
have been recreational users of cocaine who see no need to enter treatment.
At the stage of arrest, many drug users face risks associated with the seizure of their injecting
equipment, as this increases the risks of syringe sharing the next time they use drugs. The
provision of syringe exchange within police custody could reduce this risk. The revised 2007
ACPO Drug Strategy for Scotland, as well as reaffirming the support of police forces for
harm reduction interventions, also acknowledges the role of the introduction of syringe
exchange schemes in custody suites. As MacDonald et al. (2008) have stated:
Research has demonstrated that the police can have a role in harm reduction provision, without
necessarily compromising their legal and moral values. For example, they can encourage users
in detention to make use of local needle exchange sites and provide information on their location,
and they can use discretion in not arresting users at such sites, while consulting with the community
on the need for such methods.
(MacDonald et al., 2008, p. 6)
Early interventions have been implemented in many European states to avoid the negative
impact of both continuous untreated drug addiction and conviction and possibly
incarceration. ‘FreD goes net’ is a European network of such early intervention projects,
which are diverting young drug users from police to counselling agencies to avoid adverse
effects of the criminal justice system (LWL, 2009).
In a number of European countries legislation expands the options available to the courts for
the diversion of drug-related offenders away from the criminal justice system to treatment, or
for court-mandated treatment to form part of a sentence (EMCDDA, n.d.). Although data on
usage of these options remain rare (European Commission, 2008), it seems they have
historically been under-used (Turnbull and Webster, 1997). Few have been formally evaluated
(Hough et al., 2003). Those that have been evaluated have tended to show that treatment that
is entered through the legal system can be as effective as when people enter through other
modes (McSweeney et al., 2007; Stevens et al., 2005). The under-exploitation of opportunities
to divert drug users from the criminal justice system through alternative measures to
imprisonment remains a major problem — particularly in new Member States of the European
Union — which demands further investigation and action. In Cyprus in 2008, for example, a
law had existed since 1992 that enabled drug-using offenders to be diverted into treatment, but
no suitable treatments were in place and so the law was not used (Fotsiou, 2008).
Conclusion
The evidence and examples provided in this chapter have shown that it is possible to
negotiate the tensions between law enforcement and harm reduction. Services have been
successfully implemented that have reduced the harms experienced by drug users in the
criminal justice system. However, implementation in many countries remains at the level
of discussion, or small pilot projects. It is rare that countries actually practice the principle
of equivalence between services inside and outside prisons to which they have signed
up. And the chances of rapid extension of harm reduction in criminal justice systems may
seem to be low, given the current scale of economic uncertainty and strains on the public
purse.
Nevertheless, given the frequent contact between drug users and criminal justice systems,
and ongoing epidemics of blood-borne viruses linked to problem drug use, there is an urgent
need for harm reduction services to be scaled-up. Reducing the numbers of drug users in
prison will be the least costly means of increasing the proportion of prisoners who have
access to harm reduction. It would reduce demand for drug services in prison and would free
up resources to spend on harm reduction and other services, assuming that these resources
are not diverted away from working with drug users.
Additional challenges remain. These include the need to develop and expand services for
non-opiate users (such as methamphetamine users in parts of Eastern Europe, and cocaine/
crack users in the United Kingdom; see Decorte, 2008; Hartnoll et al., 2010), as well as the
challenge of involving drug users themselves in the design and delivery of harm reduction
services (see Hunt et al., 2010), which are especially severe when those drug users are
subject to the criminal justice system.
All elements of the criminal justice system have roles to play in the reduction of drug-related
harm, including police officers, prosecutors, courts, prisons, probation services and nongovernmental
organisations that work with offenders. Harm reduction is a challenge for law
enforcement, and law enforcement is a challenge for harm reduction. The contradictions
between the aims of these two approaches cannot be wished away. However, we can protect
both public health and individual rights to healthcare by acknowledging these tensions and
finding ways to move beyond them to provide high-quality harm reduction services to all
who need them.
Acknowledgements
The authors’ gratitude goes to the various reviewers of this chapter who helped us to improve
it and to the EMCDDA for providing useful information.
References
Acín García, E. J. (2008), ‘Un enfoque global sobre la prevención y el control del VIH en las prisiones de España’,
Secretaría General de instituciones Penitenciarias, Ministerio del Interior, Gobierno de España, presentation at
the Internacional Harm Reduction Conference, Bangkok 2008.
Allen, A-M. (2001), Drug-related knowledge and attitudes of prison officers in Dublin prisons, Thesis submitted for
the degree of M.Sc. in Community Health, Department of Community Health and General Practice, Trinity
College, Dublin, October.
Allwright, S., Bradley, F., Long, J., et al. (2000), ‘Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and
risk factors in Irish prisoners: results of a national cross sectional survey’, British Medical Journal 321 (7253), pp.
78–82.
Bean, P. (2008), Drugs and crime, 3rd edition, Willan Publishing, Cullompton.
Bertrand, D. and Niveau, G. (eds) (2006), Médecine, santé et prison, Editions Medecine & Hygiene, Chene-Bourg.
Bravo, M. J., de la Fuente, L., Pulido, J., et al. (2009), ‘Spanish HIV/AIDS epidemic among IDUs and the policy
response from an historical perspective’, Presentation at the 5th European Conference on Clinical and Social
Research on AIDS and Drugs, Vilnius, 28–30 April 2009.
Carter, A. and Hall, W. (2010, in press), ‘The rights of individuals treated for drug, alcohol and tobacco
addiction’, in Dudley, M., Silove, D. and Gale, F. (eds) (2010), Mental health and human rights, Oxford University
Press, Oxford.
Caulkins, J. P. and Reuter, P. (2009), ‘Towards a harm-reduction approach to enforcement’, Safer Communities 8
(1), pp. 9–23.
Christie, N. (1982), Limits to pain, Martin Robertson, Oxford.
Cook, C. (2009), Harm reduction policy and practice worldwide: an overview of national support for harm reduction
in policy and practice, International Harm Reduction Association, Victoria and London. Available at http://www.
ihra.net/HRWorldwide.
Cook, C., Bridge, J. and Stimson, G. V. (2010), ‘The diffusion of harm reduction in Europe and beyond’, in
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm reduction: evidence, impacts and
challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of the
European Union, Luxembourg.
Commission on Narcotic Drugs (2002), Preventing the transmission of HIV among drug abusers: a position paper of
the United Nations system, endorsed on behalf of ACC by the High-Level Committee on Programme (HLCP) at its first
regular session of 2001, Vienna, 26–27 February 2001, document E/CN.7/2002/CRP.5 for participants at the
Forty-fifth session, Vienna, 11–15 March 2002. Available at http://www.cicad.oas.org/en/Resources/
UNHIVaids.pdf.
Crawley, D. (2007), Good practice in prison health, Department of Health, London.
DeBeck, K., Wood, E., Zhang, R., et al. (2008), ‘Police and public health partnerships: evidence from the
evaluation of Vancouver’s supervised injection facility’, Substance Abuse Treatment Prevention Policy May, 7 (3),
p. 11. DOI: 10.1186/1747-597X-3-11.
Decorte, T. (2008), ‘Problems, needs and service provision related to stimulant use in European prisons’,
International Journal of Prisoner Health 3 (1), pp. 29–42. Available at http://dx.doi.
org/10.1080/17449200601149122.
Department of Health/National Offender Management Service (2009), Guidance notes: prison health
performance and quality indicators, Department of Health, London. Available at http://www.hpa.nhs.uk/web/
HPAwebFile/HPAweb_C/1232006593707.
Dolan, K. and Wodak, A. (1999), ‘HIV transmission in a prison system in an Australian State’, Medical Journal of
Australia 171 (1), pp. 14–17.
Dolan, K. A., Wodak, A. D. and Hall, W. D. (1998), ‘Methadone maintenance treatment reduces heroin injection
in New South Wales prisons’, Drug and Alcohol Review June, 17 (2), pp. 153–8.
Dolan, K., Shearer, J., White, B. and Wodak, A. (2002), A randomised controlled trial of methadone maintenance
treatment in NSW prisons, National Drug and Alcohol Research Centre, Sydney.
Dolan, K., Khoei, E. M., Brentari, C. and Stevens, A. (2007) Prisons and drugs: a global review of incarceration,
drug use and drug services. Report 12. Discussion paper, The Beckley Foundation, Oxford. Available at http://kar.
kent.ac.uk/13324/.
Dorn, N. and South, N. (1990), ‘Drug markets and law enforcement’, British Journal of Criminology 30 (2), pp.
171–88.
Dublin Declaration on HIV/AIDS in Prisons in Europe and Central Asia (2004), Prison health is public health, Irish
Penal Reform Trust, Dublin.
Duke, K. (2003), Drugs, prisons and policy-making, Palgrave, Basingstoke.
ECOSOC (United Nations Economic and Social Council) (2009), Political declaration and plan of action on
international cooperation towards an integrated and balanced strategy to counter the world drug problem, United
Nations, Vienna.
Edmunds, M., May, T., Hearnden, I. and Hough, M. (1998), Arrest referral: emerging lessons from research, Home
Office, London.
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (n.d.), Treatment as an alternative to
prosecution or imprisonment for adults, ELDD Topic overview, European Monitoring Centre for Drugs and Drug
Addiction, Lisbon. Available at http://eldd.emcdda.europa.eu/html.cfm/index13223EN.html (accessed 3
December 2009).
EMCDDA (2002), Prosecution of drug users in Europe: varying pathways to similar objectives, Insights series number
5, European Monitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.
eu/html.cfm/index33988EN.html.
EMCDDA (2005), Alternatives to imprisonment: targeting offending problem drug users in the EU, Selected issue,
European Monitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/
html.cfm/index34889EN.html.
EMCDDA (2009a), Annual report 2009: the state of the drugs problem in Europe, European Monitoring Centre for
Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/publications/annualreport/
2009.
EMCDDA (2009b), Statistical bulletin 2009, Table HSR-7: availability and level of provision of selected health
responses to prisoners in 26 EU countries, Norway and Turkey (expert ratings), European Monitoring Centre for
Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab7.
EMCDDA (2009c), Statistical bulletin 2009, Table HSR-4: year of introduction of needle and syringe programmes
and types of programmes (NSP) available in 2007, European Monitoring Centre for Drugs and Drug Addiction,
Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab4.
EMCDDA (2009d), Statistical bulletin 2009, Figure HSR-2: provision of substitution/maintenance treatment (OST)
in the community and availability of OST programmes in the prison system in 2007 (expert rating), European
Monitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/stats09/
hsrfig2.
European Commission (2007), ‘Report from the Commission to the European Parliament and the Council on the
implementation of the Council Recommendation of 18 June 2003 on the prevention and reduction of healthrelated
harm associated with drug dependence’, COM (2007) 199 final. Available at http://eur-lex.europa.eu/
LexUriServ/site/en/com/2007/com2007_0199en01.pdf.
European Commission (2008), Commission staff working document: accompanying document to the communication
from the Commission to the Council and the European Parliament on an EU drugs action plan 2009–2012. Report of
the final evaluation of the EU drugs action plan (2005–2008), COM(2008) 567, SEC(2008) 2455, SEC(2008)
2454, European Community, Brussels. Available at http://eur-lex.europa.eu/SECMonth.
do?year=2008&month=09.
Farrell, M. and Marsden, J. (2008), ‘Acute risk of drug-related death among newly released prisoners in England
and Wales’, Addiction February 103 (2), pp. 251–5.
Farrell, M., Gowing, L. R., Marsden, J. and Ali, R. L. (2001), ‘Substitution treatment for opioid dependence: a
review of the evidence and the impact’, in Council of Europe (ed.), Development and improvement of substitution
programmes: proceedings of a seminar organized by the Cooperation Group to combat Drug Abuse and Illicit
Trafficking in Drugs (Pompidou Group), Strasbourg, France, 8–9 October 2001, pp. 27–54.
Fazel, S., Bains, P. and Doll, H. (2006), ‘Substance abuse and dependence in prisoners:
a systematic review’, Addiction 101 (2), pp. 181–91.
Fotsiou, N. (2008), Personal communication, Cyprus Anti-Drugs Council, Nicosia.
Fox, A. (2000), Prisoners’ aftercare in Europe: a four countries study, European Network of Drug and HIV/AIDS
Services in Prison (ENDHASP), Cranstoun Drug Services, London.
Gendreau, P., Goggin, C. and Cullen, F. T. (1999), The effects of prison sentences on recidivism, Solicitor General
Canada, Public Works and Government Services Canada, Ottawa. Available at http://www.prisonpolicy.org/
scans/gendreau.pdf.
Greenwald, G. (2009), Drug decriminalization in Portugal: lessons for creating fair and successful drug policies,
Cato Institute, Washington, DC. Available at http://www.cato.org/pub_display.php?pub_id=10080.
Hagan, H. (2003), ‘The relevance of attributable risk measures to HIV prevention planning’, AIDS 17, pp. 911–13.
Hartnoll, R., Gyarmarthy, A. and Zabransky, T. (2010), ‘Variations in problem drug use patterns and their
implications for harm reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm
reduction: evidence, impacts and challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.
10, Publications Office of the European Union, Luxembourg.
Hassim, A. (2006), ‘The “5 star” prison hotel: the right of access to ARV treatment for HIV positive prisoners in
South Africa’, International Journal of Prisoner Health 2 (3), pp. 157–72.
Hedrich, D. (2004), European report on drug consumption rooms, European Monitoring Centre for Drugs and Drug
Addiction, Lisbon. Available at http://www.emcdda.europa.eu/html.cfm/index54125EN.html.
Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, in
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm reduction: evidence, impacts and
challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of the
European Union, Luxembourg.
Heimer, R., Catania, H., Zambrano, J. A., et al. (2005), ‘Methadone maintenance in a men’s prison in Puerto
Rico: a pilot program’, Journal of Correctional Health Care, The Official Journal of the National Commission on
Correctional Health Care 11 (3), pp. 295–306.
Hough, M., Clancy, A., McSweeney, T. and Turnbull, P. J. (2003), ‘The impact of drug treatment and testing
orders on offending: two year reconviction results’, Home Office Research Findings No. 184, Home Office,
London.
Hughes, C. and Stevens, A. (2007), The effects of the decriminalization of drug use in Portugal, Beckley
Foundation, Oxford. Available at http://www.idpc.net/php-bin/documents/BFDPP_BP_14_
EffectsOfDecriminalisation_EN.pdf.pdf.
Hunt, N. (2003), A review of the evidence-base for harm reduction approaches to drug use, Forward Thinking on
Drugs, London. Available at http://www.iprt.ie/contents/1328.
Hunt, N., Albert, E. and Montañés Sánchez, V. (2010), ‘User involvement and user organising in harm reduction’,
in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm reduction: evidence, impacts and
challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of the
European Union, Luxembourg.
IDT (Instituto da Droga e da Toxicodependência) (2005), Relatório anual 2004 — A situação do país em matéria
de drogas e toxicodependências. Volume I - Informação estatística, Instituto da Droga e da Toxicodependência,
Lisbon. Available at http://www.idt.pt.
IDT (2006), Relatório anual 2005 — A situação do país em matéria de drogas e toxicodependências. Volume I -
Informação estatística, Instituto da Droga e da Toxicodependência, Lisbon. Available at http://www.idt.pt.
IDT (2007), Portugal: new developments, trends and in-depth information on selected issues: 2006 National report
(2005 data) to the EMCDDA by the Reitox National Focal Point, Instituto da Droga e da Toxicodependência, Lisbon.
Available at http://www.idt.pt.
Inciardi, J. A., Martin, S. S., Butzin, C. A., Hooper, R. M. and Harrison, L. D. (1997), ‘An effective model of
prison-based treatment for drug-involved offenders’, Journal of Drug Issues, 27 (2), pp. 261–78.
Jürgens, R., Ball, A. and Verster, A. (2009), ‘Interventions to reduce HIV transmission related to injecting drug use
in prison’, Lancet Infectious Diseases 9, pp. 57–66.
Kastelic, A., Pont, J. and Stöver, H. (2008), Opioid substitution treatment in custodial settings: a practical guide,
BIS-Verlag, Oldenburg. Available at http://www.unodc.org/documents/baltics/OST%20in%20Custodial%20
Settings.pdf.
Keppler, K., Nolte, F. and Stöver, H. (1996), ‘Übertragungen von Infektionskrankheiten im Strafvollzug —
Ergebnisse einer Untersuchung in der JVA für Frauen in Vechta [Transmission of infectious diseases in prison:
results of a study in the prison for women in Vechta]’, Sucht 42 (2), pp. 98–107. Available at http://www.neuland.
com/index.php?s=sxt&s2=inh&s3=1996204.
Kerr, T., Macpherson, D. and Wood, E. (2008), ‘Establishing North America’s first safer injection facility: lessons
from the Vancouver experience’, in Stevens, A. (ed.), Crossing frontiers: international developments in the treatment
of drug dependence, Pavilion Publishing, Brighton, pp. 109–29.
Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence of
effectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm reduction:
evidence, impacts and challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,
Publications Office of the European Union, Luxembourg.
Kinlock, T. W., Gordon, M. S., Schwartz, R. P., Fitzgerald, T. T. and O’Grady, K. E. (2009), ‘A randomized
clinical trial of methadone maintenance for prisoners: results at 12 months postrelease’, Journal of Substance
Abuse Treatment 37, pp. 277–85
Kovandzic, T. V. and Vieraitis, L. M. (2006), ‘The effect of county-level prison population growth on crime rates’,
Criminology and Public Policy 5 (2), pp. 213–44.
Larney, S. and Dolan, K. (2009), ‘A literature review of international implementation of opioid substitution
treatment in prisons: equivalence of care?’, European Addiction Research 15, pp. 107–12.
Lind, B., Chen, S., Weatherburn, D. and Mattick, R. (2005), ‘The effectiveness of methadone maintenance
treatment in controlling crime: an Australian aggregate-level analysis’, British Journal of Criminology 45 (2), pp.
201–11.
Lines, R. (2008), ‘The right to health of prisoners in international human rights law’, International Journal of
Prisoner Health 4 (1), pp. 3–53.
Lines, R., Jürgens, R., Betteridge, G., et al. (2006), Prison needle exchange: lessons from a comprehensive review of
international evidence and experience, 2nd edition, Canadian HIV/AIDS Legal Network, Toronto. Available at
http://www.aidslaw.ca/publications/publicationsdocEN.php?ref=184.
LWL (Landschaftsverband Westfalen-Lippe) (2009), Fred goes net: Early intervention for young drug users,
Landschaftsverband Westfalen-Lippe, Münster. Available at http://www.lwl.org/LWL/Jugend/lwl_ks/Projekte_
KS1/Fgn-english/.
MacCoun, R. J. and Reuter, P. (2001), Drug war heresies: learning from other vices, times, and places, Cambridge
University Press, Cambridge.
MacDonald, M. (2005), A study of health care provision, existing drug services and strategies operating in prisons in
ten countries from central and eastern Europe, Heuni, Helsinki. Available at http://www.heuni.fi/12542.htm.
MacDonald, M., Atherton, S., Berto, D., et al. (2008), Service provision for detainees with problematic drug and
alcohol use in police detention: a comparative study of selected countries in the European Union, Paper No. 27,
European Institute for Crime Prevention and Control, affiliated with the United Nations (HEUNI), Helsinki.
McMillan, G. P. and Lapham, S. C. (2005), ‘Staff perspectives on methadone maintenance therapy (MMT) in a
large southwestern jail’, Addiction Research and Theory 13 (1), pp. 53–63.
McSweeney, T., Stevens, A., Hunt, N. and Turnbull, P. (2007), ‘Twisting arms or a helping hand? Assessing the
impact of “coerced” and comparable “voluntary” drug treatment options’, British Journal of Criminology 47 (3),
pp. 470–90.
Marteau, D. and Stöver, H. (2010, in press), ‘The introduction of the prisons “Integrated Drug Treatment System
(IDTS)” in England’, International Journal of Prisoner Health.
Mathiesen, T. (2006), Prison on trial, 3rd edition, Waterside Press, Winchester.
Matic, S., Lazarus, J. V., Nielsen, S. and Laukamm-Josten, U. (eds) (2008), Progress on implementing the Dublin
Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia, WHO Regional Office for Europe,
Copenhagen. Available at http://www.euro.who.int/document/e92606.pdf.
Meyenberg, R., Stöver, H., Jacob, J. and Pospeschill, M. (1999), Infektionsprophylaxe im Niedersächsischen
Justizvollzug — Abschlußbericht, BIS-Verlag, Oldenburg.
Michel, L. (2005), ‘Substitutive treatments for major opionic dependance adapted to prison life’, Information
Psychiatrique 81 (5), pp. 417–22.
Michel, L. and Maguet, O. (2003), L’organisation des soins en matière de traitements de substitution en milieu
carcéral, Rapport pour la Commisssion nationale consultative des traitements de substitution, Centre Régional
d’Information et de Prévention du Sida Ile-de-France, Paris.
Michel, L., Carrieri, P. and Wodak, A. (2008), ‘Harm reduction and equity of access to care for French prisoners:
a review’, Harm Reduction Journal 5, p. 17. DOI: 10.1186/1477-7517-5-17.
Ministry of Labour and Social Security (2002), Instruction 101/2002 of the Directorate General on Labour Inspection
and Social Security on criteria of action in connection with the implementation in a number of prisons of the needle
exchange program for injecting drug users, 23. August 2002, Ministry of Labour and Social Security, Madrid.
Møller, L, Stöver, H., Jürgens, R., Gatherer, A. and Nikogosian, H. (eds) (2007), Health in prisons: a WHO guide
to the essentials in prison health, WHO Regional Office for Europe, Copenhagen.
Offender Health Research Network (2009), Website. Available at http://www.ohrn.nhs.uk (accessed 19 August
2009).
Parliamentary Assembly of the Council of Europe (1988), Recommendation 1080 on a co-ordinated European
health policy to prevent the spread of AIDS in prison, Council of Europe, Strasbourg. Available at http://assembly.
coe.int/documents/AdoptedText/ta88/erec1080.htm.
Pont, J. (2008), ‘Ethics in research involving prisoners’, International Journal of Prisoner Health 4 (4), pp. 184–97.
Radcliffe, P. and Stevens, A. (2008), ‘Are drug treatment services only for “thieving junkie scumbags”? Drug users
and the management of stigmatised identities’, Social Science and Medicine 67 (7), pp. 1065–73.
Reiner, R. (2000), ‘Crime and control in Britain’, Sociology: The Journal of the British Sociological Association, 34
(1), pp. 71–94.
Ritter, A. and Cameron, J. (2005), Monograph no. 06: a systematic review of harm reduction, DPMP Monograph
Series, Turning Point Alcohol and Drug Centre. Fitzroy.
Rolles, S. and Kushlick, D. (2004), After the war on drugs, Transform, Bristol.
Rotily, M., Weilandt, C., Bird, S. M., et al. (2001), ‘Surveillance of HIV infection and related risk behaviour in
European prisons: A multicentre pilot study’, European Journal of Public Health 11 (3), 243–50.
Royal College of General Practitioners (2007), Guidance for the prevention, testing, treatment and management of
hepatitis C in primary care, Royal College of General Practitioners, London. Available at http://www.smmgp.org.
uk/download/guidance/guidance003.pdf.
Seeling, C., King, C., Metcalfe, E., Tober, G. and Bates, S. (2001), ‘Arrest referral: a proactive multi-agency
approach’, Drugs: Education, Prevention and Policy 8, pp. 327–33.
Shapshank, P., McCoy, C., Rivers, J. , et al. (1993), ‘Inactivation of Human Immunodeficiency Virus-1 at short time
intervals using undiluted bleach’, Journal of Acquired Immune Deficiency Syndromes 6, pp. 218–19.
Singleton, N., Meltzer, H. and Gatward, R. (1997), Psychiatric morbidity among prisoners: summary report,
National Statistics, London. Available at http://www.statistics.gov.uk/downloads/theme_health/Prisoners_
PsycMorb.pdf.
Singleton, N., Pendry, E., Taylor, C., Farrell, M. and Marsden, J. (2003), ‘Drug-related mortality among newly
released offenders’, Findings 187, Home Office, London. Available at http://www.homeoffice.gov.uk/rds/pdfs2/
r187.pdf.
Sondhi, A., O’Shea, J. and Williams, T. (2002), ‘Arrest referral: emerging findings from the national monitoring
and evaluation programme’, DPAS Briefing Paper 18, Home Office Drug Prevention Advisory Service, London.
Stallwitz, A. and Stöver, H. (2007), ‘The impact of substitution treatment in prisons: a literature review’,
International Journal of Drug Policy 18, pp. 464–74.
Stevens, A. (2008), ‘Alternatives to what? Drug treatment alternatives as a response to prison expansion and
overcrowding’, Presentation at the 2nd Annual Conference of the International Society for the Study of Drug
Policy, 3–4 April 2008, Lisbon.
Stevens, A. (forthcoming), ‘Treatment sentences for drug users: contexts, mechanisms and outcomes’, in
Hucklesby, A. and Wincup, E. (eds), Drug interventions and criminal justice, Milton Keynes.
Stevens, A., Berto, D., Heckmann, W., et al. (2005), ‘Quasi-compulsory treatment of drug dependent offenders:
an international literature review’, Substance Use and Misuse 40, pp. 269–83.
Stevens, A., Bewley-Taylor, D. and Dreyfus, P. (2009), Drug markets and urban violence: can tackling one reduce
the other?, Beckley Foundation, Oxford.
Stöver, H. (1994), ‘Infektionsprophylaxe im Strafvollzug’, in Stöver, H. (ed.), Infektionsprophylaxe im Strafvollzug.
Eine Übersicht über Theorie und Praxis (Vol. XIV), Deutsche AIDS-Hilfe, Berlin, pp. 13–40.
Stöver, H. (2001), An overview study: assistance to drug users in European Union prisons, EMCDDA, Lisbon.
Stöver, H. (2002), ‘Consumption rooms: a middle ground between health and public order concern’, Journal of
Drug Issues 32 (2), pp. 597–606.
Stöver, H. (ed.) (2008), Evaluation of national responses to HIV/AIDS in prison settings in Estonia: evaluation carried
out on behalf of the UNODC Regional project ‘HIV/AIDS prevention and care among injecting drug users and in
prison settings in Estonia, Latvia and Lithuania’, UNODC, New York. Available at http://www.unodc.org/
documents/baltics/Report_Evaluation_Prisons_2008_Estonia.pdf.
Stöver, H. and Marteau, D. (2010, in press), ‘Scaling-up of opioid substitution treatment in custodial settings:
evidence and experiences’, International Journal of Prisoner Health.
Stöver, H. and Michels, I. I. (2010, in press), ‘Drug use and opioid substitution treatment for prisoners’, Addiction.
Stöver, H., and Nelles, J. (2003), ‘10 years of experience with needle and syringe exchange programmes in
European prisons: a review of different evaluation studies’, International Journal of Drug Policy, 14 (5–6), 437–44.
Stöver, H., Hennebel, L. and Casselman, J. (2004), Substitution treatment in European prisons: a study of policies
and practices of substitution treatment in prisons in 18 European countries, Cranstoun Drug Services, London.
Stöver, H., Casselman, J. and Hennebel, L. (2006), ‘Substitution treatment in European prisons: a study of policies
and practices in 18 European countries’, International Journal of Prisoner Health 2 (1), pp. 3–12.
Stöver, H., MacDonald, M. and Atherton, S. (2007), Harm reduction for drug users in European prisons, BISVerlag,
Oldenburg.
Stöver, H., Weilandt, C., Zurhold, H., Hartwig, C. and Thane, K. (2008a), Final report on prevention, treatment,
and harm reduction services in prison, on reintegration services on release from prison and methods to monitor/
analyse drug use among prisoners (Drug policy and harm reduction, SANCO/2006/C4/02), European Commission,
Directorate – General for Health and Consumers. Available at http://ec.europa.eu/health/ph_determinants/
life_style/drug/documents/drug_frep1.pdf .
Stöver, H., Weilandt, C., Huisman, A., et al. (2008b), Reduction of drug-related crime in prison: the impact of
opioid substitution treatment on the manageability of opioid dependent prisoners, BISDRO, University of Bremen,
Bremen.
Stöver, H., Lines, R. and Thane, K. (2009), ‘Harm reduction in European prisons: looking for champions and ways
to put evidence-based approaches into practice’, in Demetrovics, Z., Fountain, J. and Kraus, L. (eds), Old and new
policies, theories, research methods and drug users across Europe, European Society for Social Drug Research
(ESSD), pp. 34–49. Available at http://www.essd-research.eu/en/publications.html.
Sykes, G. M. (1958), The society of captives, Princeton University Press, Princeton, NJ.
Taylor, A., Goldberg, D., Emslie, J., et al. (1995), ‘Outbreak of HIV infection in a Scottish prison’, British Medical
Journal 310 (6975), pp. 289–92.
Tilson, H., Aramrattana, A., Bozzette, S., et al. (2007), Preventing HIV infection among injecting drug users in high
risk countries: an assessment of the evidence, Institute of Medicine, Washington, DC. Available at http://www.nap.
edu/catalog.php?record_id=11731.
Todts, S., Fonck, R., Colebunders, R., et al. (1997), ‘Tuberculosis, HIV hepatitis B and risk behaviour in a Belgian
prison’, Archives of Public Health 55, pp. 87–97.
Tonry, M. (2004), Punishment and politics: evidence and emulation in the making of English crime control policy,
Willan Publishing, Cullompton.
Torres, A. C., Maciel, D., Sousa, D. and Cruz, R. (2009), Drogas e Prisões — Portugal 2007, CIES/ISCTE, Lisbon.
Turnbull, P. J. and Webster, R. (1997), Demand reduction activities in the criminal justice system in the European
Union, Final Report, EMCDDA, Lisbon.
UNAIDS (Joint United Nations Programme on HIV/AIDS) (1997), Prisons and AIDS: UNAIDS technical update,
UNAIDS Best Practice Collection, United Nations, Geneva.
UNODC (United Nations Office on Drugs and Crime) and UNAIDS (2008), Women and HIV in prison settings,
United Nations, Geneva/Vienna.
UNODC, WHO and UNAIDS (2006), HIV/AIDS prevention, care, treatment and support in prison settings: a
framework for an effective national response, United Nations Office on Drugs and Crime, World Health
Organization and the Joint United Nations Programme on HIV/AIDS, Vienna and New York.
van der Gouwe, D., Gallà, M., van Gageldonk, A., et al. (2006), Prevention and reduction of health-related harm
associated with drug dependence: an inventory of policies, evidence and practices in the EU relevant to the implementation
of the Council Recommendation of 18 June 2003. Synthesis report, Contract nr. SI2.397049, Trimbos Instituut, Utrecht.
Available at http://ec.europa.eu/health/ph_determinants/life_style/drug/documents/drug_report_en.pdf.
WHO (World Health Organization) (1993), WHO guidelines on HIV infection and AIDS in prisons, WHO, Geneva.
WHO (2005), Effectiveness of drug dependence treatment in preventing HIV among injecting drug users, Evidence
for action technical papers, WHO, Geneva.
WHO (2007), Effectiveness of interventions to manage HIV in prisons: needle and syringe programmes and bleach
and decontamination strategies, Evidence for action technical papers, WHO, Geneva.
WHO (2005), WHO model list of essential medicines, 14th revision (March 2005), WHO, Geneva. Available at
http://www.who.int/medicines/publications/essentialmedicines/en/index.html.
WHO Regional Office for Europe (2005), Status paper on prisons, drugs and harm reduction, WHO Office for
Europe, Copenhagen.
WHO Regional Office for Europe (2007), ‘WHO health in prisons project’, Newsletter December, WHO Office for
Europe, Copenhagen. Available at http://www.euro.who.int/Document/HIPP/WHO_HIPP-Newsletter-dec07.pdf.
WHO, UNAIDS and UNODC (2007), Effectiveness of interventions to manage HIV in prisons: provision of condoms
and other measures to decrease sexual transmission, Evidence for action technical papers, World Health
Organization, Geneva.
Williamson, M. (2006), Improving the health and social outcomes of people recently released from prisons in the UK:
a perspective from primary care, The Sainsbury Centre for Mental Health, London. Available at http://www.scmh.
org.uk/pdfs/scmh_health_care_after_prison.pdf.
Zurhold, H., Haasen, C. and Stöver, H. (2005), Female drug users in European prisons: a European study of prison
policies, prison drug services and the women’s perspectives, BIS-Verlag, Oldenburg.
| < Prev | Next > |
|---|