Chapter 11 Drug consumption facilities in Europe and beyond
| Reports - EMCDDA Harm Reduction |
Drug Abuse
Chapter 11 Drug consumption facilities in Europe and beyond
Dagmar Hedrich, Thomas Kerr and Françoise Dubois-Arber
Abstract
Drug consumption rooms (DCRs) are professionally supervised healthcare facilities where
drug users can use drugs in safer and more hygienic conditions. Since 1986, more than
90 DCRs have been set up in Switzerland, the Netherlands, Germany, Spain,
Luxembourg, Norway, Canada and Australia. Consumption rooms aim to establish
contact with difficult-to-reach populations of drug users, provide an environment for
more hygienic drug use, reduce morbidity and mortality risks associated with drug use
— in particular street-based drug injecting — and promote drug users’ access to other
social, health and drug treatment services. They also aim to reduce public drug use and
improve public amenity near urban drug markets. At times, their establishment has been
controversial due to concerns that they may encourage drug use, delay treatment entry
or aggravate problems of local drug markets. As with evaluations of other public health
interventions, research on DCRs faces methodological challenges in taking account of the
effects of broader local policy or ecological changes. Despite these limitations, research
shows that the facilities reach their target population and provide immediate
improvements through better hygiene and safety conditions for injectors. At the same
time, the availability of safer injecting facilities does not increase levels of drug use or
risky patterns of consumption, nor does it result in higher rates of local drug acquisition
crime. There is consistent evidence that DCR use is associated with self-reported
reductions in injecting risk behaviour such as syringe sharing, and in public drug use.
Due to a lack of studies, as well as methodological problems such as isolating the effect
from other interventions or low coverage of the risk population, evidence regarding DCRs
— while encouraging — is insufficient for drawing conclusions with regard to their
effectiveness in reducing HIV or hepatitis C virus (HCV) incidence. However, use of the
facilities is associated with increased uptake of detoxification and treatment services.
While there is suggestive evidence from modelling studies that they may contribute to
reducing drug-related deaths at a city level where coverage is adequate, the review-level
evidence of this effect is still insufficient. Taken in sum, the available evidence does not
support the main concerns raised about this kind of intervention and points to generally
positive impacts in terms of increasing drug users’ access to health and social care, and
reducing public drug use and associated nuisance.
Keywords: injecting drug use, drug consumption rooms, safer injecting facilities, open drug
scenes, public nuisance, Europe.
Introduction
Drug consumption rooms (DCRs), also called safer injecting facilities, are professionally
supervised healthcare facilities providing safer and more hygienic conditions for drug users
to take drugs (Stöver, 2000). They comprise highly targeted services within wider networks of
drug services. While they often operate from separate areas located in existing facilities for
drug users or the homeless, some operate as stand-alone facilities.
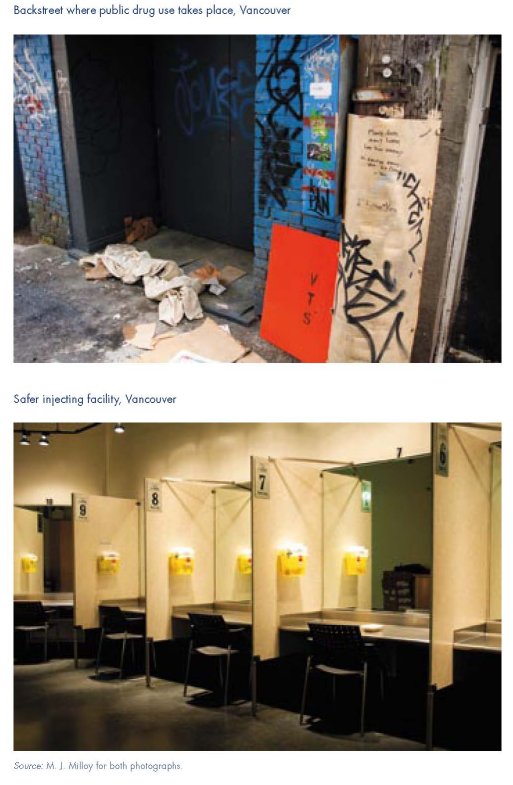
DCRs arose in specific local contexts in response to problems posed by public drug use,
especially by drug injecting in streets, railway stations or staircases of residential buildings,
that persisted despite the availability of a variety of drug treatment, harm reduction and
social services, and despite law enforcement efforts to disperse or contain public drug use.
The rationale for the establishment of DCRs was to address public health and community
problems associated with specific populations of drug users, especially injectors who
consume in public or other high-risk situations.
These groups have important unmet healthcare needs and contribute to public order
problems within local communities. A relationship between public injecting, elevated risk of
viral infections and socio-economic deprivation, especially precarious housing or
homelessness, has been long established by epidemiological research (for example, Latkin
et al., 1994; Klee and Morris, 1995; Galea and Vlahov, 2002; Navarro and Leonard,
2004; Corneil et al., 2006). Risk factors exogenous to the individual, including multiple
interacting physical, social and economic and policy factors, have been identified as
constituting a broader ‘risk environment’ affecting the health of injection drug users
(Rhodes, 2002; Rhodes et al., 2003). Qualitative research has shown that public injecting
is associated with reduced options to maintain safety and hygiene, often related to an
individual’s fear of interruption, feelings of shame and hasty injection (Small et al., 2007;
Rhodes et al., 2007).
DCRs aim to reduce high-risk and public drug use and to improve public amenity near
urban drug markets, by providing a hygienic and regulated environment for drug use off
the streets. They aim to create an acceptable situation for the public with regard to order
and safety concerns that arise from open drug scenes. As pragmatic ‘safer injecting
environment’ interventions, DCRs aim to minimise the likelihood of police and public
interference and enable individual and community risk reduction practices to occur
(Rhodes et al., 2006).
They further aim to reduce risk behaviour and improve health and social integration by:
providing clean injecting equipment (needles, syringes, spoons, filters, wipes), good light,
clean surfaces and sharps disposal; facilitating individually tailored health education, and
promoting access to healthcare and drug treatment. House rules prohibit violent and
threatening behaviour, alcohol use at the premises, drug dealing and the sharing of drugs
and any injecting equipment, and define requirements regarding hygiene and injecting
behaviour. Staff are trained to provide assistance and emergency care in cases of overdose
or other adverse events but do not assist clients to inject (see Dolan et al., 2000; Kimber et
al., 2005; Hedrich, 2004).
The first legally sanctioned DCR was established in Berne, Switzerland in 1986 (Hämmig,
1992). During the 1990s DCRs were set up in other Swiss cities, the Netherlands and
Germany; and from 2000 they were set up in Spain, Norway, Luxembourg, Australia
(Sydney) and Canada (Vancouver) (Stöver, 1991; Klee, 1991; Eastus, 2000; Zurhold et al.,
2001; Parliament of New South Wales, 1998; Health Canada, 2002). By the beginning of
2009 there were 92 operational DCRs in 61 cities, including in 16 cities in Germany, 30 cities
in the Netherlands and 8 cities in Switzerland.
In Europe, most DCRs are integrated components of local service networks offering a range
of social and health services. In Norway, and in Sydney and Vancouver, they are scientific
pilot projects, operating under legal exemptions, which focus on supervising drug
consumption and providing referral to other services (MSIC Evaluation Committee, 2001; van
Beek, 2003; Wood et al., 2003; Skretting and Olsen, 2008). While most target drug
injectors, some cater for heroin and crack smokers (Willen, 2002; Spreyermann and Willen,
2003; Simmedinger and Vogt, 2008). In all cases, the drugs used are pre-obtained and
prepared by the clients.
With objectives in public health and public order, DCRs operate within a triangle of
individual and public health interests and the public order interests of local communities
(Stöver, 2002). More than many other public services, they rely on acceptance by a wide
range of key actors: drug users, communities, other health and social agencies, police and
politicians.
The establishment of drug consumption rooms has led to some controversy and
disagreement between the International Narcotics Control Board (INCB) and some UN
Member States. This has centred on the interpretation of the international Drug
Conventions, in particular in relation to the basic provision of the Conventions obliging
States to limit the use of narcotic drugs strictly to medical and scientific purposes (INCB,
2008, p. 111).
This chapter does not address this debate; nor does it comment on the position of
consumption rooms in respect of international drug control treaties. Its purpose is to
summarise available evidence on the processes, outcomes and risks of DCRs, and also to
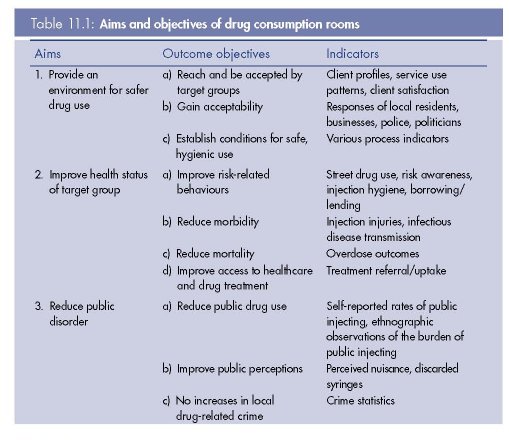
identify key challenges for their development as mechanisms of harm reduction. Our
review is structured according to the objectives of DCRs, as outlined in Table 11.1. The
balance of priorities attributed to DCRs varies, with some placing greater emphasis on
health goals, and others on public order. The main concerns expressed regarding the
establishment of DCRs is that such facilities may promote initiation to drug injecting,
conflict with treatment goals by encouraging users to continue injecting rather than enter
treatment, and increase local drug dealing and drug-related crime by attracting users
from other areas.
Methods
Experimental study designs, and in particular the randomised controlled trial, are considered
the gold standard for the generation of scientific level-1 evidence about the effects of
treatments (Ashcroft et al., 1997). Maher and Salmon (2007) discuss this imperative with
regard to the evaluation of the outcomes of DCRs, and conclude that ‘the scientific, practical
and ethical issues involved in applying this methodology to evaluating [such] complex public
health interventions (…) mean that the likelihood of obtaining this level of evidence is
negligible’ (Maher and Salmon, 2007, p. 351f). To inform public health decision-making, the
authors recommend the use of prospective observational studies (level 2 evidence) as a
feasible alternative (Maher and Salmon, 2007).
There have been relatively few rigorous evaluations of DCRs, with evidence reviews relying
primarily on analyses of descriptive data, cross-sectional survey data, and ecological
indicators from a larger number of less sophisticated studies. This is especially the case in
Europe, where DCRs emerged as a local service response with questions of evaluation arising
subsequently. However, the Sydney and Vancouver facilities were established as scientific
pilot studies, and thus incorporated more rigorous research designs (see below). The
Vancouver study is so far the only DCR evaluation to have used an elaborate prospective
cohort-based design (Wood et al., 2004a; Wood et al., 2006b).
As with any health service evaluation, a key methodological challenge is to establish causality.
It is difficult to attribute observed effects to DCRs since: (a) most users use these facilities only for
some consumption episodes and may otherwise continue to engage in risk behaviour (Dubois-
Arber et al., 2008a); and (b) other factors (typically unmeasured) in the local environment
influence levels of risk behaviour and public drug use, including policy or ecological changes
such as those related to availability of substitution treatment and other harm reduction services,
and changes in police operations or in the drug market (Maher and Dixon, 1999; Fischer et al.,
2002; Hall and Kimber, 2005). If, as in the case of evaluating syringe exchange programmes,
DCRs do succeed in attracting higher risk clients, then controlling for selection bias poses a
further challenge (Wood et al., 2007a; Schechter et al., 1999).
Cross-sectional studies have limitations regarding their interpretation, as they provide a
‘snapshot’ of the outcome and the characteristics associated with it at a specific point in time
(Bland, 2001). Repeated cross-sectional studies can be useful for tracking trends over time
(see an example in box on p. 317).
The level to which coverage of the most risky consumptions can be achieved plays an
important role in whether any impact of DCRs can be detected at community level (Kimber et
al., 2008a). For instance, in Frankfurt, in 1994 and 1995, the capacity of three DCRs with 22
places and a total of 100 coordinated opening hours per week was insufficient to cover the
demand of 300 to 400 highly problematic street injectors out of an estimated population of
6 000 to 8 000 drug users (Kemmesies, 1995). From 1996, when a fourth facility provided
13 additional places, opening hours were extended to a total of 300 per week and 4 000
injections were supervised each week. It was together with other measures and interventions,
including shelters, day-centres and treatment programmes, that a visible reduction of public
drug use in the city was achieved (Hedrich, 2004).
Further, population HIV (and perhaps HCV) incidence rates may be too low to identify
intervention effects. As a result, most outcomes can reliably only be observed at individual,
rather than at population level.
Review methods
The available evidence on DCRs was reviewed in 2004 (Hedrich, 2004), based mainly on
research published during the 1990s in the languages of countries where DCRs were
operating (German, Dutch, French and Spanish), and which were relatively inaccessible to
the English-speaking world.
The present chapter draws on this review, on research reports resulting from the evaluations
of a medically supervised injecting centre in Sydney (MSIC Evaluation Committee, 2003;
NCHECR, 2005, 2006, 2007a, 2007b) and of a safer injecting facility in Vancouver (Expert
Advisory Committee on Supervised Injection Site Research, 2008; BC Centre for Excellence in
HIV/AIDS, 2004; Wood et al., 2006b), as well as on peer-reviewed research articles on DCR
outcomes published between 2003 and 2009, and on other recent literature reviews
(Springer, 2003; Tyndall, 2003; Independent Working Group, 2006; Kerr et al., 2007a;
Fischer and Allard, 2007).
Relevant English language articles were identified using Medline. Further sources, especially
for the non-English scientific literature, which is under-represented in Medline, were identified
by reviewing reference lists, searching by author names, or through direct contact with
researchers in different countries.
Due to their scientific relevance, it is useful to note the research designs of the Sydney and
Vancouver studies. The Sydney evaluation used an observational design (MSIC Evaluation
Committee, 2001). The facility database provided data for process evaluation, including
client utilisation, referrals, overdoses, and client and staff attitudes to the service. Serial crosssectional
studies were conducted to determine impact on individual health outcomes. Using
ecological data, notifications of new infections and ambulance attendances at opioid-related
overdose events were compared between the DCR locality and control localities. Recently, the
Sydney evaluation incorporated a cohort-based element in its methodology, although only
limited data are available from this cohort (NCHECR, 2007a; Kimber et al., 2008a).
The Vancouver evaluation used a prospective cohort design (Wood et al., 2004a). A
randomly selected cohort of 1 000 users of the facility was monitored on a range of health
indicators and potential impacts including risk behaviour surveys, venous blood samples to
assess HIV and HCV incidence, overdose events, and health service use. For ethical reasons,
participation in the research was optional, although over 95 % of those invited agreed to
participate. The Vancouver evaluation’s greatest strength was the existence of a communityrecruited
cohort of over 1 500 injectors, the Vancouver Injection Drug Users Study, which
was initially recruited in 1996–97. This cohort consisted of individuals who did and did not
use the safer injecting facility, and therefore allowed for control-based comparisons, as well
as before and after analyses. As with the Sydney evaluation, the Vancouver design also
included a facility database to track all key service events (referrals, overdose, drugs used),
and data from both cohort studies were linked to a range of external databases
(detoxification programme databases, hospital databases).
Both the Sydney and Vancouver research projects included local resident surveys, qualitative
interviews with users, staff and key stakeholders, and standardised evaluations of public
order changes (discarded syringes, perceived nuisance, and crime data).
Feasibility
Objective 1a: reach and be accepted by target group
In all countries, studies have shown that the profiles of clients contacted reflect the target
groups and that DCRs generally succeed in attracting drug users who are at high risk of HIV
infection and overdose, as well as those who are likely to inject drugs in public (Hedrich,
2004; Wood et al, 2005b; Simmedinger and Vogt, 2008; Dubois-Arber et al., 2008a,
Scherbaum et al., 2009). In most of the recent studies, the majority of clients are male and
over 30 years old with long histories of drug use. According to current data from Frankfurt,
4 520 individuals used the four local DCRs at least once in 2007. These clients have an
average age of 34 years and are characterised by a high level of unemployment (65 %).
Many suffer from drug use-related infectious diseases (HCV: 53 %; HIV: 5.9 %). A majority of
DCR clients maintain regular contact with the local drug help system, and in particular make
use of low-threshold agencies (89 %), but also of outpatient drug counselling facilities (36 %).
More than half of clients (55 %) report being in medical treatment, which may include opioid
maintenance treatment (Simmedinger and Vogt, 2008). Similar sociodemographic data are
reported on 10 514 service users registered during the first seven years of operation at the
Medically Supervised Injecting Centre (MSIC) in Sydney: their average age is 33 years, 74 %
of service users are men, 61 % live mainly on social welfare benefits, and 24 % are homeless
(van Beek, 2007). A comparison of socio-demographic profiles of DRC users in Zürich
between 1997 and 2007 shows that current user populations are on average about a
decade older, have an improved housing situation (6.7 % homeless in 2007, compared to
13.8 % in 1997), and commit fewer crimes to generate income (9.4 % in 2007, compared to
30 % in 1997) (Gautschi et al., 2008).
Retention and attendance rates at the Vancouver DCR also indicate that the facility is
successful in gaining acceptance by its target group and that regular users of DCRs tend to
be more marginalised, with various health and social problems, such as those related to
unstable housing and public injecting (Wood et al., 2005b; Wood et al., 2006a). Client
surveys conducted at several facilities also show high levels of satisfaction with staff and the
services provided, as well as criticism of aspects such as opening hours (Benninghoff and
Dubois-Arber, 2002; Poschadel et al., 2003; NCHECR, 2005, 2007b; Petrar et al., 2007).
Objective 1b: gain acceptability
Surveys and qualitative research on residents, local businesses, police and other key actors
show mixed reactions to DCRs. On balance they are generally accepted by communities,
albeit with reservations. Although some police tend to be more sceptical (Zurhold et al.,
2003; Benninghoff et al., 2003; Zobel et al., 2003; BC Centre for Excellence in HIV/AIDS,
2004), there is also evidence that police in some settings are accepting of DCRs and actively
refer drug users to them (DeBeck et al., 2008).
Objective 1c: establish conditions for safe, hygienic consumption
Process evaluations indicate that DCRs provide hygienic facilities, sterile injecting equipment,
professional staffing and supervision, entrance criteria, safety rules, emergency procedures,
safer injecting instruction and health education (Ronco et al., 1996a, 1996b; Linssen et al.,
2001; Zurhold et al., 2001; Wolf et al., 2003; and Zobel and Dubois-Arber, 2004; Kimber et
al., 2005). Studies also indicate that hygiene and safety are important reasons why clients
use the facilities (Poschadel et al., 2003; Benninghoff et al., 2003). Despite millions of
injections occurring at DCRs over the past 20 years, there have been no reported overdose
fatalities (Poschadel et al., 2003; NCHECR, 2007b; Milloy et al., 2008; Expert Advisory
Committee on Supervised Injection Site Research, 2008).
The Canadian research in particular shows that concerns that DCRs delay entry into
treatment or even promote drug use are not substantiated. There were no observable
increases nor decreases in drug use in the community, and no measurable increases in rates
of relapse into injection drug use or initiation into injection drug use (Kerr et al., 2007b),
stopping injection drug use, or seeking treatment (Stoltz et al, 2007; Kerr et al., 2005,
2006a; Wood et al., 2005a). Available evidence from Sydney (MSIC Evaluation Committee,
2003; NCHECR, 2007b) and Europe (Ronco et al., 1996b; Poschadel et al., 2003;
Benninghoff et al., 2003) points to the same ‘neutral’ effect.
There are occasional reports of users making their first injection in a DCR (Benninghoff et al.,
2003; Solai et al., 2005; Kerr et al., 2007b). Whether these would have occurred in the
absence of the DCR is not known.
Conclusions on objective 1
DCRs reach and are accepted by their target populations, including marginalised street users
and those at higher risk of infectious diseases or overdose (objective 1a). They are generally
accepted by communities and key actors, or at least tolerated as the lesser of alternative evils
(objective 1b). Further, they provide conditions, especially for regular clients, that improve
hygiene and reduce exposure to health risks such as infectious diseases or overdoses
(objective 1c). The risk that some users initiate injecting at DCRs is low and there is no
evidence they increase levels of drug use or risky patterns of consumption. On the basis of
available evidence, consumption rooms achieve their immediate objective of providing an
environment away from the streets where high-risk or public drug users can consume their
drugs more safely and hygienically, and they don’t encourage drug use or injecting.
Impact on health outcomes
Objective 2a: reduce risk behaviours
The European Report on DCRs (Hedrich, 2004) identified 12 studies and one review of the impact
of DCRs in the Netherlands, Germany and Switzerland on risk behaviours. Although subject to
various methodological limitations, all European studies indicated positive effects. Staff also report
positive changes in many clients’ injecting hygiene. For example, several pre-post studies in the
Netherlands showed increased knowledge of injecting hygiene and safer drug use among DCR
users (Meijer et al., 2001; Linssen et al., 2001); cross-sectional surveys in Germany and in the
Netherlands showed self-reported improvements by large proportions of DCR clients in injectingrelated
risk behaviour, injecting practices and hygiene since using a DCR (Jacob et al., 1999;
Poschadel et al., 2003; van der Poel et al., 2003; Zurhold et al., 2001). Serial cross-sectional
surveys in Switzerland showed decreases in the proportion of DCR clients reporting syringe
sharing and sharing of other injecting equipment (Benninghoff et al., 2001, 2003; Benninghoff
and Dubois-Arber, 2002; Solai et al., 2004) as well as increases in the proportion saying they
would never accept used injecting equipment (Minder Nejedly and Bürki, 1999; Reyes Fuentes,
2003; Ronco et al., 1996a, 1996b). These earlier findings have been confirmed by Dubois-Arber
et al., 2008b and by a more recent study from Spain that also reports reduced borrowing of used
syringes among highly marginalised injecting drug users attending DCRs (Bravo et al., 2009).
Outside Europe, these results have been replicated by studies in Sydney, where DCR clients
were more likely than non-DCR clients to report using sterile syringes for all injections and
less likely to report sharing injecting equipment, and where staff also reported improved
hygiene and reduced sharing among DCR clients (MISC Evaluation Committee, 2003;
NCHECR 2007a, 2007b). Likewise in Vancouver, a prospective cohort study of injecting drug
users (IDUs) showed that syringe sharing decreased among DCR users but not among nonusers
of DCRs after the facility opened, and that the degree of reduction was associated with
greater use of the facility (Kerr et al., 2005; Wood et al, 2005a; Stoltz et al., 2007). A recent
meta-analysis shows highly similar effects of DCRs on the extent of syringe sharing across
sites, with frequent DCR use being associated with a 70 % reduced likelihood of reporting
syringe sharing (Milloy and Wood, 2009).
Collectively, these studies provide clear evidence that DCR use is associated with reduced
self-reported and observed injecting risk behaviour, including the risk of overdose, and
improvements in reported and observed injecting hygiene, especially among those who use
the facilities consistently.
Objective 2b: reduce morbidity
Few studies report on injection-related injuries, although such injuries may represent a
significant source of morbidity among people who inject drugs (Palepu et al., 2001;
Salmon et al., 2009a). In Sydney, a small decrease in the frequency of injection-related
problems over time was observed among DCR clients, including less bruising, scarring
and abscesses (NCHECR, 2007b). In Vancouver, the risk of injecting-related bacterial
infections decreased among DCR users, and the use of the facility was independently
associated with other safe injection practices, including decreased reuse of syringes,
increased use of sterile water and increased cleaning of injection sites with alcohol
swabs (Stoltz et al., 2007). There is further evidence from qualitative studies undertaken
in Vancouver of the potential impact of DCRs on reducing the incidence of soft tissue
infections (Small et al., 2008; Krüsi et al., 2009) and of the advantages of nursedelivered
safer injection education in reaching IDUs most at risk for injection-related
harm (Wood et al., 2008; Lloyd-Smith et al., 2009).
No conclusions can be drawn about the direct impact of DCRs on infectious disease
incidence, owing to a lack of studies as well as methodological problems, such as isolating
the effect of DCRs from other interventions (substitution treatment, needle exchange,
outreach), low rates of HIV/HCV incidence, or low coverage of the risk population. For
example, in Sydney, health authorities were notified of fewer newly diagnosed HCV, HIV and
HBV infections in the DCRs’ locality compared to other control localities (MSIC Evaluation
Committee, 2003). However, no evidence was found that any changes in the number of
notified cases were attributable to the DCR. Furthermore, the low incidence of HCV and HIV
among IDUs in Australia made it unlikely that the number of cases would be sufficient to
detect any statistically significant associations. Limited coverage of the facility was also
unlikely to produce a detectable community impact on incidence.
Objective 2c: reduce mortality (overdoses)
There is some evidence of the impact of DCRs on mortality, but this evidence is mostly indirect
and based on the outcome of emergencies occurring in the facilities (see box on p. 144). The
majority of emergencies among users of DCRs involve heroin injection-related overdoses,
with smaller proportions involving cocaine use. Emergency rates vary from 0.5 to 7 per
1 000 injections (see Hedrich, 2004, for Germany, Netherlands, Switzerland and Spain; Kerr
et al., 2006b, for Vancouver; NCHECR, 2007b, for Syndey; and Skretting and Olsen, 2008,
for Norway). As rapid intervention is available at DCRs, these events are less severe than
overdoses occurring elsewhere, and fewer ambulance attendances or hospitalisations are
needed (NCHCR, 2007b). In addition, DCRs located near open drug scenes may respond to
overdoses in the immediate vicinity (Hedrich, 2004). None of the overdoses recorded at
DCRs have resulted in death (the only known death at a DCR involved anaphylactic shock).
Furthermore, by providing immediate intervention following the first signs of overdose, other
impacts of non-fatal overdose-related events, including irreversible damage to the brain and
other vital organs due to hypoxia, can also be prevented (van Beek et al., 2004; Hämmig
and van Beek, 2005; NCHECR, 2007b).
Apart from potential fatalities prevented through supervised consumption among clients,
there are several estimates of the impact of DCRs on drug deaths at population or city
level. Based on utilisation data and expected mortality rates among the populations
reached by DCRs, it has been estimated that these facilities helped prevent 10 deaths per
year in Germany, and four per year in Sydney (Hedrich, 2004; MSIC Evaluation
Committee, 2003). In a comparison of overdose death trends in the vicinity of the DCR with
the rest of the region of New South Wales, no statistically significant impact of the Sydney
facility on opioid-related deaths in Kings Cross was found. Due to an approximate 70 %
decrease in overdose deaths following a heroin shortage in Australia, the researchers
argue that the assessment of the impact may have been hampered by small sample sizes
(NCHECR, 2007b, p. 29). In their simulation of the impact of the Vancouver DCR, Milloy
and colleagues (2008) concluded that the facility may have prevented between 1.9 and
11.7 overdose deaths per year.
An ecologically based time-series analysis involving four German cities from 1990–2001
concluded that statistically significantly reductions in overdose fatalities were observed in
Saarbrücken and Hannover six months after the opening of the DCR, and in Hamburg and
Frankfurt after the opening of the third and fourth rooms respectively (Poschadel et al.,
2003).
While it is impossible to ascertain how many emergencies would have occurred and been
fatal in the absence of DCRs, epidemiological and clinical data suggest that immediate staff
interventions at emergencies occurring at DCRs, where millions of drug consumptions have
taken place under supervision, has reduced the impact of overdose-related events, such as
morbidity and death. Where coverage and capacity are sufficient and opening hours
appropriate, DCRs may contribute to reducing drug-related deaths at a city level.
Objective 2d: improve access to healthcare and drug treatment
There are large variations between countries regarding services offered on-site, which make
comparisons difficult. Different policies towards accepting clients who are already in
substitution treatment also affect treatment referral rates. Regarding referrals to treatment,
only the Vancouver and Sydney studies measure actual uptake.
In most European DCRs a range of other services are usually delivered on-site alongside
supervision of drug consumption. Low-threshold medical care and psychosocial counselling
services are especially well used and contribute to the stabilisation and improvement of the
somatic and psychological health of users (Linssen et al., 2001; Poschadel et al., 2003;
Zurhold et al., 2001; van der Poel et al., 2003; Ronco et al., 1994). Clients are also referred
to drug treatment or other care, though proportions vary and uptake rates are often
unknown. For instance, in the survey of all German consumption rooms, over half of all
clients reported having received a referral by DCR staff to other drug or social services at
least once (Poschadel et al., 2003).
In both Vancouver and Sydney, use of the facility was associated with more exposure to safe
injecting education and access to healthcare (Wood et al., 2006a, 2007b; van Beek, 2003;
Tyndall et al., 2006; NCHECR, 2007a, 2007b; Kimber et al., 2008b). In Vancouver, a 30 %
increased uptake of detoxification and subsequent addiction treatment were noted. For
frequent attenders in particular, DCRs act as a link to the wider system of healthcare and
facilitate entry to treatment: in Vancouver, entering a detoxification programme was more
likely among IDUs who visited the facility at least weekly and among those who had contact
with onsite addiction counsellors (Wood et al., 2007b).
The above results suggest that DCRs complement rather than conflict with treatment goals. In
fact, with the exception of the initial years of DCR operation, current typical client populations
at DCRs are in (or have successfully been brought into) contact with other harm reduction
and treatment services, and many oscillate between those, or make parallel use of them. This
reflects the complementary role of DCRs within a comprehensive drug policy approach, such
as in Switzerland, where long-term behavioural trends and health-related impacts are
documented (see box on p. 317).
Studies assessing the effectiveness of treatment consistently show that opioid maintenance
treatment reduces the level of illicit opiate use and the frequency of injecting. Drug use and
injecting may, however, still occur among clients in opioid maintenance, and clients in
treatment may also use DCR facilities. For instance, during the first seven years of operation
of the MSIC in Sydney, 13 % of all clients registering at the facility indicated that they were in
methadone treatment (van Beek, 2007). Data from the first year of operation of the DCR in
Geneva (2002) show that a majority (61.1 %) of users declared at the time of enrolment that
they were in substitution treatment (Dubois-Arber, 2008a).
The question of whether clients in oral methadone treatment should use DCRs for injection is
dealt with in different ways. In Germany, and Luxembourg, methadone clients are formally
excluded from most consumption rooms. Elsewhere, however, the pragmatic view is taken
that if methadone clients are going to inject anyway it is better that they do so in hygienic
circumstances where there is also the opportunity for staff to talk with them.
|
Long-term behavioural trends and health-related impact of harm reduction facilities, In 1993, 1994, 1996, 2000 and 2006 repeated national cross-sectional surveys were Between 1993 and 2006, current injecting — in the last six months — decreased among those During the same period (1993–2006), the national monitoring of injecting equipment showed This overall evolution cannot be attributed exclusively to the availability of NSPs and DCRs. |
Conclusions on objective 2
DCRs help to improve the health status of the target population and contribute to
reductions in high-risk injecting behaviour. There is evidence that when coverage and
capacity are adequate, DCRs help to reduce overdose deaths. Available evidence does
not allow conclusions to be drawn on whether or not they have specific, attributable
impact on HIV and HCV infection rates, although fairly substantial reductions in HIV and
HCV risk behaviour have been associated with DCR use. DCRs do increase access for
specific ‘hard-to reach’ target populations of drug users to health, welfare and drug
treatment services.
Impact on public order and crime outcomes
Objective 3a: reduce public drug use
Direct evidence of the impact of DCRs on levels of public drug use is limited and sometimes
mixed. This is because of methodological limitations, restricted coverage, the difficulty of
knowing how many facility-based injections would otherwise have occurred in public, and
because other factors, such as police activity or changes in the drug market, also affect
public drug use.
Studies in the Netherlands, Germany, Switzerland, Sydney and Vancouver showed lower levels
of self-reported public drug use among clients (van der Poel et al., 2003; Zurhold et al., 2001;
Poschadel et al., 2003; Benninghoff and Dubois-Arber, 2002; Stoltz et al., 2007; NCHECR,
2007b). However, it was not always possible to attribute this effect to DCRs (Zobel and Dubois-
Arber, 2004). In Vancouver, the opening of the DCR was associated with a reduction of public
injection, discarded syringes and drug-related litter (Wood et al., 2006a). In this instance, these
effects were found independently of changes in police presence and weather patterns. In
Sydney there was a reduction in public drug use among regular clients and reduced community
visibility of injecting drug use (NCHECR, 2007b; Kimber et al., 2008b).
Among those who attended DCRs some report that they also continued to take their drugs in
public places, when the DCR had insufficient space, was located away from drug purchase
sites or when opening hours were restricted (Zurhold et al., 2001, 2003; Poschadel et al.,
2003). Public injecting in some DCR localities may increase as a result of police actions to
reduce drug markets in other areas (Benninghoff et al., 2003; Poschadel et al., 2003;
Hedrich, 2004).
Objective 3b: improve public perceptions
Evidence related to public perceptions is also mixed. Several German, Swiss and Dutch
studies have reported mostly acceptance of DCRs, at least as a preferable option to public
use (Linssen et al., 2001; Zurhold et al., 2003; Zobel et al., 2003). In Vancouver, a survey
among a random sample of 117 business owners located in the vicinity of the DCR found that
54 (46 %) were in favour of having a DCR, 23 were undecided and 40 were opposed to it.
Businesses located further away from the facility showed less support (BC Centre for
Excellence in HIV/AIDS, 2004). A five-year evaluation of the community perceptions of drugrelated
amenity before (year 2000) and after the opening of the Sydney DCR (surveys
conducted in 2002 and 2005) among local residents and businesses found a significant
decrease over time of those who reported recently witnessing public injection and improperly
discarded syringes (Salmon et al., 2007) and that community attitudes tended to become
more positive over time (Thein et al., 2005; MSIC Evaluation Committee, 2003). However,
attributing these improvements to the DCR was complicated by a concurrent heroin shortage
and rise in stimulant use. In Germany and Switzerland some DCRs have encountered strong
opposition from local residents, which diminished with experience of the DCR in operation.
Generally, fewer nuisance problems are reported in cities where a political consensus or
cooperation between police and drugs services exists (Hedrich, 2004).
Effects on local crime
No increase in acquisitive crime has been observed after the opening of DCRs in the
Netherlands and Switzerland (Linssen et al., 2001; Meijer et al., 2001; Spreyermann and
Willen, 2003; Benninghoff et al., 2003).
The impact of the safer injecting facility in Vancouver on public disorder and drug-related
crime has been studied extensively, including through follow-up studies comparing the
situation before and after the opening of the facility (see box below). Furthermore, no
evidence of negative impacts of the operation of the facility on community drug use patterns
has been found (Kerr et al., 2006a).
|
The impact of the Vancouver DCR on crime, nuisance, safety and police referrals The Vancouver DCR, known as ‘Insite’, is situated in a large open drug scene. The area is |
In Sydney, an evaluation of the crime statistics in the relevant neighbourhoods
documented that operation of the MSIC DCR did not lead to increases in crime or social
disturbance in its immediate vicinity. There was no evidence of any positive or negative
impact on rates of drug-related crime, drug-related loitering, and no increase in the
proportion of supply offences following the opening of the MSIC (NCHECR, 2007b;
Freeman et al., 2005).
Most European reports show a similar picture. However, there have been reports from a few
European facilities of increases in drug dealing around the facility (Geense, 1997; Zurhold et
al., 2001), as well as aggressive incidents outside the premises, increases in petty crime and
resentment from local residents (Kimber et al., 2005).
Conclusions on public order and crime outcomes
Consumption rooms can reduce the level of drug use in public. The extent to which this is
achieved depends on their accessibility, opening hours and capacity. There is no evidence
that the operation of consumption rooms leads to more acquisitive crime. There is small-scale
drug dealing in the vicinity of many services, which is not surprising given their location.
Nuisance is more likely when capacity or location of the facility does not meet local needs
and waiting times are long. In some instances, these problems can be addressed by an
adjustment of service capacity, aided by police cooperation and the involvement of the DCR
in local order maintenance. However, facilities near illicit drug markets are not able to solve
wider nuisance problems that result from these markets. Consumption rooms have greater
impact where there is a political consensus that they are part of a comprehensive local
strategy to respond to drug use-related problems that acknowledges public and individual
health objectives as well as the need to maintain an acceptable situation with regard to order
and safety in the community.
Challenges
The evidence reviewed in this chapter indicates that DCRs may contribute to reducing drugrelated
harms in settings where public drug use and injecting pose serious public health and
social problems. For the future, these types of interventions face a number of challenges. The
first set of challenges arises from changing patterns of drug use and drug using contexts and
the new configurations of harms that these may imply. The second set of challenges concerns
creating the environmental conditions that enable the reach and impact of existing DCRs and
the development of new projects where there is a demonstrated need.
Targeting interventions in a changing world of drug use
Changing drug use situations present challenges for harm reduction interventions, calling for
the capacity of responses to adapt rapidly to shifts in drug use, risks, target groups and
needs (see also Hartnoll et al., 2010). Such changes may impact on: the prevalence or
frequency of injecting; modes of drug administration (such as inhaling or smoking); patterns
of drug use (for example, the injecting of crack cocaine, cocaine or amphetamine, or
‘speedball’); and risk environments.
Operational data collected at European DCRs shows that there is a cumulative ‘revolving
door’ client group of ageing injectors (Simmedinger and Vogt, 2008), but also that there
are new groups of service users, in some cases young, for whom differentiated responses
regarding safer use education are needed (Sozialdepartement der Stadt Zürich, 2008).
Additionally, increases in cocaine injecting observed in several European countries
(EMCDDA, 2009) may imply increased frequency of injecting and associated health
harms, including vein damage, bacterial and viral infections (see also Grund et al., 2010).
The use of DCRs by clients in opioid maintenance treatment may also point to ineffective
treatment regimes or to clients for whom methadone is unsuitable. In one case, a small
subgroup (4 % of DCR clients) who mainly injected cocaine, were among the most
frequent users of the facility, accounting for almost two-fifths of all injections observed in
the year of study (2002) (Dubois-Arber et al., 2008a). Most of this group (65 %) were in
methadone treatment at the time they had registered at the facility. Differentiated
intervention emphasis should therefore be tailored to different and changing client needs,
including through integrating referral and service delivery as part of a wider local system
response to drug treatment and care (Dubois-Arber et al., 2008a). Studies also show that
frequent DCR users may use the room as a place of socialisation and support
(Benninghoff et al., 2003).
Most DCRs target drug injectors, with the exception of the Netherlands, where the
majority of places are for smoking, reflecting the low proportion of injectors in the
problem drug use population. Limited facilities for smoking have been added to some
DCRs in Germany and Switzerland, and a room has been opened specifically for crack
users in Frankfurt and for heroin smokers in Hamburg. Although smoking is generally
seen as less risky than injecting, there may still be health risks, for example of transmitting
HCV through sharing crack smoking paraphernalia (Fischer et al., 2008; Macías et al.,
2008; Neaigus et al., 2007; Grund et al., 2010), as well as problems associated with
public drug use. The expected benefits of implementing facilities for smoking at DCRs
include contact with recent or younger users with the possibility of facilitating early
treatment and reducing the risk of HCV infection.
Given the increased prevalence of both heroin smoking and the use of crack cocaine in a
number of EU countries, assessment of the advantages and disadvantages of providing
facilities for non-injectors, and the manner in which such services are best delivered merits
further research.
The examples given above suggest that DCRs can play a wider and more proactive role
than originally envisaged, in particular with regard to transmitting tailored health
education messages to individual clients and to developing realistic prevention and safer
use messages for the wider population of problem drug users. Because DCRs are for most
clients not the main place of drug use (Dubois-Arber et al., 2008a; MSIC Evaluation
Committee, 2003; Hedrich, 2004), learning to consume drugs safely in other contexts is
an important individual outcome to be achieved. From this perspective, DCRs could be a
basis from which to extend peer education and community-oriented projects to modify
local risk environments (Pretil, 2007). In this regard, as frontline services, DCRs have the
potential to constitute a sensitive and timely early warning system about drug use trends
and effects of market changes (Degenhardt et al., 2008); they can help to gain in-depth
knowledge of risky drug use practices and risk-increasing aspects of the local environment
(Salmon et al., 2009a; 2009b).
Creating an enabling environment for intervention
Where DCRs are ‘normative’ as part of established harm reduction policy (Switzerland,
Germany, the Netherlands, Luxembourg, Norway, parts of Spain), they are likely to continue
and evolve. In this situation they face the challenges outlined above. In other countries, the
situation is different. In some, there is a polarisation of public debate leading to the rejection
of proposals, in others there is ambivalence resulting in a deadlock of new initiatives. The
role of DCRs in the future has to be seen in the context of developments regarding public
drug use and accessibility, as well as quality of drug treatment, including the existence of real
reintegration options, funding and sustained political commitment.
If DCRs are to have an impact at community level it is necessary to provide sufficient
capacity relative to the estimated size of the target population, to locate rooms on sites that
are easily accessible, and to ensure that opening hours are long enough to meet demand,
especially in the evenings and on weekends. Staffing and modus operandi are also
important. Assessing the cost-effectiveness and impact of different service models at
different levels of population coverage in different epidemiological settings is a key
research question for the future.
In settings where there is a demonstrable need for DCRs, their development and the extent to
which they can achieve their objectives is tempered by the broader social and policy context.
A qualitative assessment of the literature suggests that DCRs can only be effective if they are:
• integrated into a wider public policy framework as part of a network of services aiming to
reduce individual and social harms arising from problem drug use;
• based on consensus, support and active cooperation among key local actors, especially
health, police, local authorities, local communities and consumers themselves;
• seen for what they are — specific services aiming to reduce problems of health and social
harm involving particular high-risk populations of problematic drug users and addressing
needs that other responses have failed to meet.
Conclusion
This chapter has focused on scientific evidence regarding whether DCRs, as a specific
intervention, have achieved their stated objectives. Despite some limitations of the available
evidence, the broad conclusion is that DCRs do bring benefits on specific aspects of
individual and public health and social order without incurring serious risks. To achieve
this, adequate coverage is essential, as is political support and consensus between key
actors.
Expectations towards DCRs thus need to be realistic, as they cannot address all the key
variables of drug-related harms. They do not change the fact that users buy their drugs
in illicit markets, nor can they aim to change the drug market itself. They are, however,
an effective public health intervention providing a ‘safer environment’ to reduce risks
inherent in public drug use; they are unique in their capacity to develop individually
tailored health education that achieves sustainable behavioural change among the most
vulnerable populations; and the facilities provide clear benefits by increasing drug users’
access to health and social care, and in reducing public drug use and associated
nuisance.
|
DCRs — implications for practice Drug consumption rooms can only be effective if they are: • integrated into a wider public policy framework as part of a network of services aiming to |
References
Ashcroft, R. E., Chadwick, D. W., Clark, S. R. L., et al. (1997), ‘Implications of socio-cultural contexts for the
ethics of clinical trials’, Health Technology Assessment I (9). Available at http://www.hta.ac.uk/project/htapubs.
asp (accessed 23 October 2009).
BC Centre for Excellence in HIV/AIDS (2004), Evaluation of the supervised injection site: year one summary, BC
Centre for Excellence in HIV/AIDS, Vancouver. Available at http://www.vch.ca/sis/docs/sis_year_one_sept16.
pdf (accessed 3 June 2009).
Benninghoff, F. and Dubois-Arber, F. (2002), Résultats de l’étude de la clientèle du Cactus BIEL/BIENNE 2001, Institut
universitaire de médecine sociale et préventive, Lausanne.
Benninghoff, F., Geense, R. and Dubois-Arber, F. (2001), Resultats de l’étude ‘La clientèle des structures à bas seuil
d’accessibilité en Suisse’, Institut universitaire de médecine sociale et préventive, Lausanne.
Benninghoff, F., Solai, S., Huissoud, T. and Dubois-Arber, F. (2003), Evaluation de Quai 9 ‘Espace d’acceuil et
d’injection’ à Genéve: période 12/2001–12/2000, Raisons de santé 103, Institut universitaire de médecine sociale et
préventive, Lausanne.
Bland, M. (2001), An introduction to medical statistics, 3rd edition, Oxford University Press, Oxford.
Bravo, M. J., Royuela, L., De la Fuente, L., et al. (2009), ‘Use of supervised injection facilities and injection risk
behaviours among young drug injectors’, Addiction 104 (4), pp. 6124–9.
Corneil, T. A., Kuyper L. M., Shoveller, J., et al. (2006), ‘Unstable housing, associated risk behaviour, and
increased risk for HIV among injection drug users’, Health Place 12, pp. 79–85.
DeBeck, K., Wood, E., Zhang, R., Tyndall, M., Montaner, J. and Kerr, T. (2008), ‘Police and public health
partnerships: evidence from the evaluation of Vancouver’s supervised injection facility’, Substance Abuse
Treatment Prevention Policy 7 May, 3, p. 11 (DOI:10.1186/1747-597X-3-11).
Degenhardt, L., Roxburgh, A., van Beek, I., et al. (2008), ‘The effects of the market withdrawal of temazepam gel
capsules on benzodiazepine injecting in Sydney, Australia’, Drug and Alcohol Review 27 (2), pp. 145–51.
Dolan, K., Kimber, J., Fry, C., et al. (2000), ‘Drug consumption facilities in Europe and the establishment of
supervised injecting centers in Australia’, Drug and Alcohol Review — Harm Reduction Digest 10 (19), pp. 337–46.
Dubois-Arber, F., Benninghoff, F. and Jeannin, A. (2008a), ‘Typology of injection profiles of clients of a
supervised drug consumption facility in Geneva, Switzerland’, European Addiction Research 14, pp. 1–10.
Dubois-Arber, F., Balthasar, H., Huissoud, T., et al. (2008b), ‘Trends in drug consumption and risk of transmission
of HIV and hepatitis C virus among injecting drug users in Switzerland, 1993–2006’, Eurosurveillance 22 May,
13 (21).
Eastus, C. (2000), ‘Die Entwicklung von Gesundheitsräumen in der Schweiz’, Akzeptanz -Zeitschrift für
akzeptierende Drogenarbeit und humane Drogenpolitik 8 (1), pp. 10–12.
EMCDDA (2009), Annual report on the state of the drugs problem in the European Union, 2009, European
Monitoring Centre for Drugs and Drug Addiction, Lisbon.
Expert Advisory Committee on Supervised Injection Site Research (2008), Vancouver’s Insite service and other
supervised injection sites: what has been learned from the research? Final report, 31 March 2008, Health Canada,
Ottawa, Ontario. Available at http://www.hc-sc.gc.ca/ahc-asc/pubs/_sites-lieux/insite/index-eng.php (accessed
3 June 2009).
Fischer, B. and Allard, C. (2007), Feasibility study on ‘supervised drug consumption’ options in the City of Victoria,
Centre for Addictions Research of British Columbia (CARBC), University of Victoria, Victoria. Available at http://
www.viha.ca/NR/rdonlyres/9C3846B7-4836-4F1C-8CE2-952273E3A439/0/carbc_feasibility_study.pdf
(accessed 15 January 2010).
Fischer, B., Rehm, J., Kim, G. and Robins, A. (2002), ‘Safer injecting facilities (SIFs) for injection drug users (IDUs)
in Canada: a review and call for an evidence-focused pilot trial’, Canadian Journal of Public Health 93 (5), pp.
336–8.
Fischer, B., Powis, J., Firestone Cruz, M., Rudzinski, K. and Rehm, J. (2008), ‘Hepatitis C virus transmission among
oral crack users: viral detection on crack paraphernalia’, European Journal of Gastroenterology & Hepatology
January, 20 (1), pp. 29–32.
Freeman, K., Jones, C. G., Weatherburn, D. J., et al. (2005), ‘The impact of the Sydney MSIC on crime’, Drug and
Alcohol Review 24 (2), pp. 173–84.
Galea, S. and Vlahov, D. (2002), ‘Social determinants and the health of drug users: socioeconomic status,
homelessness, and incarceration’, Public Health Reports 117 (Supplement 1), pp. S135–S145.
Gautschi, T., Hangartner, D. and Magnin, C. (2008), ‚Kontakt- und Anlaufstellen der Stadt Zürich. Eine Analyse
der Bedürfnisse Ihrer Benützerinnen und Benützer‘, in Stadt Zürich — Sozialdepartement (ed.), „Ein Ort wo man
sein kann“. Die Zukunft der „Harm Reduction“ am Beispiel der Kontakt- und Anlaufstellen der Stadt Zürich, Edition
Sozialpraxis Nr.3, Zürich, pp. 13–57.
Geense, R. (1997), ‘Evaluation of the federal measures to reduce problems related to drug use. To have or have
not: that’s the question. A qualitative study on four low-threshold needle exchange services for drug users in
Switzerland’, Cah Rech Doc IUMSP, no. 111.11, University of Social and Preventive Medicine, Prevention
Programmes Evaluation Unit, Lausanne.
Gervasoni, J-P. and Dubois-Arber, F. (2009), Indicateurs de résultats du Promedro III, situation en 2008 : rapport
final, Raisons de santé 147, Institut universitaire de médecine sociale et préventive, Lausanne.
Grund, J-P., Coffin, P., Jauffret-Roustide, M., et al. (2010), ‘The fast and furious: cocaine, amphetamines and harm
reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm reduction: evidence,
impacts and challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications
Office of the European Union, Luxembourg.
Hämmig, R.B. (1992), ‘The streetcorner agency with shooting room (Fixerstübli)’, in O’Hare, P. A., Newcombe, R.,
Matthews, A., Buning E. C., and Drucker, E. (eds), The reduction of drug related harm, Routledge, London, pp.
181–5.
Hämmig, R. and van Beek, I. (2005), ‘Supervised injecting rooms’, in Pates, R., McBride, A. and Arnold, K. (eds),
Injecting illicit drugs, Wiley-Blackwell, Chichester.
Hall, W. and Kimber, J. (2005), ‘Being realistic about benefits of supervised injecting facilities’, Lancet 23–29
July, 366 (9482), pp. 271–2.
Hartnoll, R., Gyarmarthy, A. and Zabransky, T. (2010), ‘Variations in problem drug use patterns and their
implications for harm reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), Harm
reduction: evidence, impacts and challenges, Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.
10, Publications Office of the European Union, Luxembourg.
Health Canada (2002), ‘Application for an exemption under section 56 of the Controlled Drugs and Substances
Act for a scientific purpose for a pilot supervised injection site research project: interim guidance document’, Drug
Strategy and Controlled Substances Programme, Healthy Environments and Consumer Safety Branch, Health
Canada, Ottawa.
Hedrich, D. (2004), European report on drug consumption rooms, EMCDDA, Lisbon.
INCB (International Narcotics Control Board) (2008), Report of the International Narcotics Control Board for 2007,
E/INCB/2007/1, United Nations, New York. Available at http://www.incb.org/incb/en/annual-report-2007.html
(accessed 11 January 2010).
Independent Working Group (2006), The report of the Independent Working Group on Drug Consumption Rooms,
Joseph Rowntree Foundation, York. Available at http://www.jrf.org.uk/publications/drug-consumption-roomssummary-
report-independent-working-group (accessed 3 June 2009).
Jacob, J., Rottmann, J. and Stöver, H. (1999), Entstehung und Praxis eines Gesundheitsraumangebotes für
Drogenkonsumierende. Abschlußbericht der einjährigen Evaluation des ‘drop-in Fixpunkt’ in Hannover, Schriftenreihe
Sucht- und Drogenforschung, Vol. 2., BIS-Verlag, Universität Oldenburg, Oldenburg.
Kemmesies, U. (1995), Szenebefragung 1995. Die offene Drogenszene und das Gesundheitsraumangebot in
Frankfurt am Main – ein erster Erfahrungsbericht, Indro, Münster (English version: Kemmesies, U. (1999), The open
drug scene and the safe injection room offers in Frankfurt am Main 1995, Indro, Münster). Available at http://www.
indro-online.de/injection_room.htm (accessed 27 August 2009).
Kerr, T., Tyndall, M., Li, K., Montaner, J. and Wood, E. (2005), ‘Safer injecting facility use and syringe sharing in
IDUs’, Lancet 23–29 July, 366 (9482), pp. 316–18.
Kerr, T., Stoltz, J. A., Tyndall, M., et al. (2006a), ‘Impact of a medically supervised safer injection facility on
community drug use patterns: a before and after study’, BMJ 28 January, 332 (7535), pp. 220–2.
Kerr, T., Tyndall, M., Lai, C., Montaner, J. and Wood, E. (2006b), ‘Drug-related overdoses within a medically
supervised safer injection facility’, International Journal of Drug Policy 17 (5), pp. 436–41.
Kerr, T., Kimber, J., Debeck, K. and Wood, E. (2007a), ‘The role of safer injection facilities in the response to HIV/
AIDS among injection drug users’, Current HIV/AIDS Reports 4 (4), pp. 158–64.
Kerr, T., Tyndall, M. W., Zhang, R., et al. (2007b), ‘Circumstances of first injection among illicit drug users
accessing a medically supervised safer injection facility’, American Journal of Public Health 97 (7), pp. 1228–30.
Kimber, J., Dolan, K., van Beek, I., Hedrich, D. and Zurhold, H. (2003a), ‘Drug consumption facilities: an update
since 2000’, Drug and Alcohol Review/Harm Reduction Digest 21, 22 (2), pp. 227–33.
Kimber, J., MacDonald, M., van Beek, I., et al. (2003b), ‘The Sydney Medically Supervised Injecting Centre:
client characteristics and predictors of frequent attendance during the first 12 months of operation’, Journal of
Drug Issues 33, pp. 639–48.
Kimber, J., Dolan, K. and Wodak, A. (2005), ‘Survey of drug consumption rooms: service delivery and perceived
public health and amenity impact’, Drug and Alcohol Review 24, pp. 21–4.
Kimber, J., Hickman, M., Degenhardt, L., Coulson, T., and van Beek, I. (2008a), ‘Estimating the size and
dynamics of an injecting drug user population and implications for health service coverage: comparison of
indirect prevalence estimation methods’, Addiction 103 (10), pp. 1604–13.
Kimber, J., Mattick, R. P., Kaldor, J., et al. (2008b), ‘Process and predictors of treatment referral and uptake’, Drug
and Alcohol Review 27, pp. 602–12.
Kimber, J., Palmateer, N., Hutchinson, S., Hickman, M., Goldberg, D. and Rhodes, T. (2010), ‘Harm reduction
among injecting drug users: Evidence of effectiveness’, in European Monitoring Centre for Drugs and Drug
Addiction (EMCDDA) Harm reduction: evidence, impacts and challenges, Rhodes, T. and Hedrich, D. (eds),
Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.
Klee, J. (ed.) (1991), Akzeptanzorientierte Angebote in der Drogen- und AIDS-Selbsthilfe: Gesundheitsräume in der
aktuellen Debatte, Deutsche Aidshilfe (DAH), Berlin.
Klee, H. and Morris, J. (1995), ‘Factors that characterize street injectors’, Addiction 90 (6), pp. 837–41.
Krüsi, A., Small, W., Wood, E. and Kerr, T. (2009), ‘An integrated supervised injecting program within a care
facility for HIV-positive individuals: a qualitative evaluation’, AIDS Care 21 (5), pp. 638–44.
Latkin C., Mandell, W, Vlahov, D., et al. (1994), ‘My place, your place and no place: behaviour settings as a risk
factor for HIV-related injection practices of drug users in Baltimore, Maryland’, American Journal of Community
Psychology 22, pp. 415–30.
Linssen, L., de Jong, W. and Wolf, J. (2001), Gebruiksruimten. Een systematisch overzicht van de voorziening en de
effecten ervan. Series: Resultaten Scoren, Trimbos Instituut, Utrecht. Available at www.ggznederland.nl/scrivo/
asset.php?id=306955 (accessed 3 June 2009).
Lloyd, C. and Hunt, N. (2007), ‘Drug consumption rooms: an overdue extension to harm reduction policy in the
UK?’, International Journal of Drug Policy 18, pp. 5–7.
Lloyd-Smith, E., Wood, E., Zhang, R., et al. (2009), ‘Determinants of cutaneous injection-related care at a
supervised injecting facility’, Annals of Epidemiology 19, pp. 404–09.
Maher, L. and Dixon, D. (1999), ‘Policing and public health: harm minimization and law enforcement in a streetlevel
drug market’, British Journal of Criminology 39, pp. 488–512.
Maher, L. and Salmon, A. (2007), ‘Supervised injecting facilities: how much evidence is enough?’, Drug and
Alcohol Review July 26 (4), pp. 351–3.
Macías, J., Palacios, R. B., Claro, E., et al. (2008), ‘High prevalence of hepatitis C virus infection among
noninjecting drug users: association with sharing the inhalation implements of crack, Liver International July, 28
(6), pp. 781–6.
McKnight, I., Maas, B., Wood, E., et al. (2007), ‘Factors associated with public injecting among users of
Vancouver’s supervised injection facility’, American Journal of Drug and Alcohol Abuse 33 (2), pp. 319–25.
Meijer, G., de Jong, A., Koeter, M. and Bieleman, B. (2001), Gebruik van de straat. Evaluatie gebruiksruimnte
Binnenstad-Zuid Groningen, Amsterdam Institute for Addiction Research (AIAR)/Intraval, Amsterdam/Groningen.
Abstract in Dutch available at http://blowkwartet.nl/default4597.html?back=1 (accessed 15 January 2010).
Milloy, M. J. and Wood, E. (2009), ‘Emerging role of supervised injecting facilities in human immunodeficiency
virus prevention’, Addiction 104 (4), pp. 620–1.
Milloy, M. J., Kerr, T., Tyndall, M., Montaner, J. and Wood, E. (2008), ‘Estimated drug overdose deaths averted
by North America’s first medically-supervised safer injection facility’, PLoS ONE 3 (10), p. e3351.
Minder Nejedly, M and Bürki, C. M. (1999), ‘Monitoring HIV risk behaviours in a street agency with injection
room in Switzerland’, dissertation, Medical Faculty of the University in Berne, Berne.
MSIC Evaluation Committee (2001), Evaluation Protocol for the trial of a Medically Supervised Injecting Centre in
Kings Cross, NSW Parliament, Standing Committee on Social Issues, Sydney. Available at http://www.worldcat.
org/oclc/223407460&referer=brief_results (accessed 23 October 2009).
MSIC Evaluation Committee (2003), Final report of the evaluation of the Sydney Medically Supervised Injecting
Centre, Authors, Sydney. Available at http://www.druginfo.nsw.gov.au/__data/page/1229/NDARC_final_
evaluation_report4.pdf (accessed 3 June 2009).
Navarro, C. and Leonard, L. (2004), ‘Prevalence and factors related to public injecting in Ottawa, Canada:
implications for the development of a trial safer injecting facility’, International Journal of Drug Policy, 15, pp.
275–84.
NCHECR (National Centre in HIV Epidemiology and Clinical Research) (ed.) (2005), Sydney Medically Supervised
Injecting Centre evaluation report no. 1: operations and service delivery (November 2002 to December 2004),
University of New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/
resources/Interim_eval_Rep1/$file/INT_EVAL_REP_+1_SYD_+MSIC.pdf (accessed 3 June 2009).
NCHECR (ed.) (2006), Sydney Medically Supervised Injecting Centre evaluation report no. 2: evaluation of
community attitudes towards the Sydney MSIC, University of New South Wales, Sydney. Available at http://www.
nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_eval_Rep1/$file/IntRep2SurveyMSICJul06.pdf
(accessed 3 June 2009).
NCHECR (ed.) (2007a), Sydney Medically Supervised Injecting Centre evaluation report no. 3: evaluation of client
referral and health issues, University of New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/
NCHECRweb.nsf/resources/Interim_eval_rep_2/$file/EvalRep4SMSIC.pdf (accessed 3 June 2009).
NCHECR (ed.) (2007b), Sydney Medically Supervised Injecting Centre evaluation report no. 4: evaluation of service
operation and overdose-related events, National Centre in HIV Epidemiology and Clinical Research, University of
New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_
eval_rep_2/$file/EvalRep4SMSIC.pdf (accessed 3 June 2009).
Neaigus, A., Gyarmathy, V. A., Miller, M., et al. (2007), ‘Sexual and other noninjecting risks for HBV and HCV
seroconversions among noninjecting heroin users’, Journal of Infectious Diseases 195 (7), pp. 1052–61.
Palepu, A., Tyndall, M. W., Leon, H., et al. (2001), ‘Hospital utilization and costs in a cohort of injection drug
users’, Canadian Medical Association Journal 165, pp. 415–20.
Parliament of New South Wales (1998), Joint Select Committee into Safe Injecting Rooms report on the establishment
or trial of safe injecting rooms, Parliament of New South Wales, Sydney. Available at http://www.parliament.nsw.
gov.au/safeinjectingrooms (accessed 3 June 2009).
Petrar, S., Kerr, T., Tyndall, M. W., et al. (2007), ‘Injection drug users’ perceptions regarding use of a medically
supervised safer injecting facility’, Addictive Behaviours 32 (5), pp. 1088–93.
Pretil, X. S. (2007), ‘En qué sentido deberían evolucionar las salas de consumo supervisado?’ Mesa redonda, ddz
cdd, October 2007, 144, p. 10.
Poschadel, S., Höger, R., Schnitzler, J. and Schreckenberger, J. (2003), Evaluation der Arbeit der
Drogenkonsumräume in der Bundesrepublik Deutschland: Endbericht im Auftrag des Bundesministeriums für
Gesundheit, Das Bundesministerium für Gesundheit und Soziale Sicherung (Schriftenreihe Bd 149), Nomos-
Verlags-Gesellschaft, Baden-Baden.
Reyes Fuentes, V. C. (2003), ‘15 Jahre Fixerraum Bern. Auswirkungen auf soziale und medizinische Aspekte bei
Drogenabhängigen’, dissertation at the Medical Faculty of the University of Berne.
Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,
International Journal of Drug Policy 13, pp. 85–94.
Rhodes, T., Lilly, R., Fernández, C., et al. (2003), ‘Risk factors associated with drug use: importance of “risk
environment”’, Drugs: education, prevention, and policy, 10 (4), pp. 303–29.
Rhodes, T., Kimber, J., Small, W., et al. (2006), ‘Public injecting and the need for “safer environment
interventions” in the reduction of drug-related harm’, Addiction 101, pp. 1384–93.
Rhodes, T., Watts, L., Davies, S., et al. (2007), ‘Risk, shame and the public injector’, Social Science and Medicine
65, pp. 572–85.
Ronco, C., Spuler, G., Coda, P. and Schöpfer, R. (1994), Evaluation der Gassenzimmer I, II und III in Basel (full
report), Institut für Sozial- und Präventivmedizin der Universität Basel, Basel.
Ronco, C., Spuler, G., Coda, P. and Schöpfer, R. (1996a), ‘Evaluation der Gassenzimmer I, II und III in Basel
[Evaluation of street facilities I, II and III in Basel]’, Sozial- und Präventivmedizin, 41 (Supplement 1), pp. S58–S68.
Abstract in English available at http://www.ncbi.nlm.nih.gov/pubmed/8693818.
Ronco, C., Spuhler, G. and Kaiser, R. (1996b), ‘Evaluation des “Aufenthalts- und Betreuungsraums für
Drogenabhängige” in Luzern [Evaluation of a stay and care center for drug addicts in Lucerne]’, Sozial- und
Präventivmedizin, 41 (Supplement 1), pp. S45–S57. Abstract in English available at http://www.ncbi.nlm.nih.gov/
pubmed/8693816.
Salmon, A., Thein, R., Kimber, J., Kaldor, J. and Maher, L. (2007), ‘Five years on: what are the community
perceptions of drug-related public amenity following the establishment of the Sydney Medically Supervised
Injecting Centre?’, International Journal of Drug Policy 18 (1), pp. 46–53.
Salmon, A. M., Dwyer, R., Jauncey, M., et al. (2009a), ‘Injecting-related injury and disease among clients of a
supervised injecting facility’, Drug Alcohol Dependence 101 (1–2), pp. 132–6.
Salmon, A. M., van Beek, I., Amin, J., Grulich, A. and Maher, L. (2009b), ‘High HIV testing and low HIV
prevalence among injecting drug users attending the Sydney Medically Supervised Injecting Centre’, Australian
and New Zealand Journal of Public Health 33 (3), pp. 280–3.
Schechter, M. T., Strathdee, S. A., Cornelisse, P. G., et al. (1999), ‘Do needle exchange programmes increase the
spread of HIV among injection drug users? An investigation of the Vancouver outbreak’, AIDS 16 April, 13 (6),
pp. F45–F51.
Scherbaum, N., Specka, M., Bombeck, J. and Marziniak, B. (2009), ‘Drug consumption facility as part of a
primary health care centre for problem drug users: which clients are attracted?’, International Journal of Drug
Policy 20 (5), pp. 447–9.
Simmedinger, R. and Vogt, I. (2008), Auswertung der Frankfurter Konsumraumdokumentation 2007. Endbericht,
ISFF, Frankfurt am Main.
Skretting, A. and Olsen H. (2008), ‘The Norwegian injection room trial: politics and controversies’, Nordic Studies
on Alcohol and Drugs 25 (4), pp. 269–83.
Small, W., Rhodes, T., Wood, E. and Kerr, T. (2007), ‘Public injecting settings in Vancouver: physical
environment, social context and risk’, International Journal of Drug Policy 18, pp. 27–36.
Small, W., Wood, E., Lloyd-Smith, E., Tyndall, M. and Kerr, T. (2008), ‘Accessing care for injection-related
infections through a medically supervised injecting facility: a qualitative study’, Drug and Alcohol Dependence 98
(1–2), pp. 159–62.
Solai, S., Benninghoff, B., Meystre-Agustoni, G., Jeannin, A. and Dubois-Arber, F. (2004), ‘Evaluation de l’espace
d’accueil et d’injection “Quai 9” à Genève: deuxième phase 2003’, Raisons de santé, 102, Institut universitaire de
médecine sociale et préventive, Lausanne. Available at http://www.iumsp.ch/Unites/uepp/files/Quai9GE_2.pdf
(accessed 3 June 2009).
Solai, S., Dubois-Arber, F., Benninghoff, F. and Benaroyo, L. (2006), ‘Ethical reflections emerging during the
activity of a low threshold facility with supervised drug consumption room in Geneva, Switzerland’, International
Journal of Drug Policy 17 (1), pp. 17–22.
Sozialdepartement der Stadt Zürich (ed.) (2008), „Ein Ort wo man sein kann“. Die Zukunft der „Harm Reduction“
am Beispiel der Kontakt- und Anlaufstellen der Stadt Zürich, Edition Sozialpraxis Nr. 3, Zürich.
Spreyermann, C. and Willen, C. (2003), Evaluationsbericht Öffnung der Kontakt- und Anlaufstellen für risikoärmere
Konsumformen. Evaluation der Inhalationsräume der Kontakt- und Anlaufstellen Selnau und Seilergraben der
Ambulanten Drogenhilfe Zürich, Sfinx, Berne. Available at http://www.sfinx.ch/siteman/file/innovation/
Evaluationsbericht.pdf (accessed 3 June 2009).
Springer, A. (2003), Konsumräume. Expertise im Auftrag des Fonds Soziales Wien, Ludwig-Boltzmann-Institut für
Suchtforschung, Anton-Proksch-Institut, Wien. Available at http://www.api.or.at/lbi/pdf/040622_expertise_
konsumraeume.pdf (accessed 3 June 2009).
Stoltz, J. A., Wood, E., Small, W., et al. (2007), ‘Changes in injecting practices associated with the use of a
medically supervised safer injection facility’, Journal of Public Health 29 (1), pp. 35–9.
Stöver, H. (ed.) (1991), Der tolerierte intravenöse Drogengebrauch in den Angeboten der Drogen- und AIDS-Hilfe.
Ein Sammelband, AIDS-Forum der Deutschen AIDS-Hilfe, Vol. VI, DAH, Berlin.
Stöver, H. (2000), ‘Konsumräume als professionelles Angebot der Suchtkrankenhilfe - Internationale Konferenz
zur Erarbeitung von Leitlinien’, Bundesgesundheitsblatt — Gesundheitsforschung — Gesundheitsschutz, 43, pp.
290–2.
Stöver, H. (2002), ‘Consumption rooms: a middle ground between health and public order concerns’, Journal of
Drug Issues 32 (2), pp. 597–606.
Thein, H. H., Kimber, J., Maher, L., MacDonald, M. and Kaldor, J. M. (2005), ‘Public opinion towards supervised
injecting centres and the Sydney Medically Supervised Injecting Centre’, International Journal of Drug Policy 16
(4), pp. 275–80.
Tyndall, M. (2003), ‘Impact of supervised injection facilities on community HIV levels: a public health
perspective’, Expert Review of Anti-Infective Therapy 1 (4), pp. 543–9.
Tyndall, M., Kerr, T., Zhang, R., et al. (2006), ‘Attendance, drug use patterns and referrals made from North
America’s first supervised injection facility’, Drug and Alcohol Dependence 83, pp. 193–8.
van Beek, I. (2003), ‘The Sydney Medically Supervised Injecting Centre: a clinical model’, Journal of Drug Issues
33, pp. 625–38.
van Beek, I. (2007), The Medically Supervised Injecting Centre: the first 7 years, Clinical Activity Data. Available at
www.sydneymsic.com (MSIC_NDARC_07.ppt) (accessed 27 August 2009).
van Beek, I., Kimber, J., Dakin, A and Gilmour, S. (2004), ‘The Sydney Medically Supervised Injecting Centre:
reducing harm associated with heroin overdose’, Critical Public Health 14 (4), pp. 391–406.
van der Poel, A., Barendregt, C. and van de Mheen, D. (2003), ‘Drug consumption rooms in Rotterdam: an
explorative description’, European Addiction Research, 9, pp. 94–100.
Willen, C. (2002), Evaluation Inhalationsraum. Pilotprojekt der Anlaufstelle Rötzmatt, Suchthilfe Region Olten (SHO),
Sfinx, Berne. Available at http://www.sfinx.ch/html/portfolio_act.html (accessed 3 June 2009).
Wolf, J., Linssen, L. and de Graaf, I., assisted by van Dam, T. (2003), ‘Drug consumption facilities in the
Netherlands’, Journal of Drug Issues 33, pp. 649–61.
Wood, E., Kerr, T., Spittal, P. M., et al. (2003), ‘The potential public health and community impacts of safer
injecting facilities: evidence from a cohort of injecting drug users’, Journal of Acquired Immune Deficiency
Syndrome 32 (1), pp. 2–8.
Wood, E., Kerr, T., Lloyd-Smith, E., et al. (2004a), ‘Methodology for evaluating Insite: Canada’s first medically
supervised safer injection facility for injection drug users’, Harm Reduction Journal 1 (1), p. 9. Available at http://
www.harmreductionjournal.com/content/1/1/9 (accessed 3 June 2009).
Wood, E., Kerr, T., Montaner, J. S., et al. (2004b), ‘Rationale for evaluating North America’s first medically
supervised safer-injecting facility’, Lancet Infectious Diseases 4, pp. 301–06.
Wood, E., Kerr, T., Small, W., et al. (2004c), ‘Changes in public order after the opening of a medically
supervised safer injecting facility for illicit injection drug users’, Canadian Medical Association Journal, 171 (7),
pp. 731–4.
Wood, E., Tyndall, M. W., Stoltz J. A., et al. (2005a), ‘Factors associated with syringe sharing among users of a
medically supervised safer injecting facility’, American Journal of Infectious Diseases 1 (1), pp. 50–4.
Wood, E., Tyndall, M.W., Li, K., et al. (2005b), ‘Do supervised injecting facilities attract higher-risk injection drug
users?’, American Journal of Preventive Medicine, 29 (2), pp. 126–30.
Wood, E., Tyndall, M. W., Qui, Z., et al. (2006a), ‘Service uptake and characteristics of injection drug users
utilizing North America’s first medically supervised safer injecting facility’, American Journal of Public Health, 96,
pp. 770–3.
Wood, E., Tyndall, M. W., Montaner, J. S. and Kerr, T. (2006b), ‘Summary of findings from the evaluation of a
pilot medically supervised safer injecting facility’, Canadian Medical Association Journal, 175 (11), pp. 1399–404.
Wood, E., Tyndall, M. W., Lai, C., Montaner, J. S. and Kerr, T. (2006c), ‘Impact of a medically supervised safer
injecting facility on drug dealing and other drug-related crime’, Substance Abuse Treatment, Prevention, and Policy,
1 (13). Published online 8 May 2006. DOI: 10.1186/1747-597X-1-13.
Wood, E., Lloyd-Smith, E., Li, K., et al. (2007a), ‘Frequent needle exchange use and HIV incidence in Vancouver,
Canada’, American Journal of Medicine 120 (2), pp. 172–9.
Wood, E., Tyndall, M. W., Zhang, R., Montaner, J. S. and Kerr, T. (2007b), ‘Rate of detoxification service use
and its impact among a cohort of supervised injecting facility users’, Addiction 102 (6), pp. 916–19.
Wood, R. A., Wood, E., Lai, C., et al. (2008), ‘Nurse-delivered safer injection education among a cohort of
injection drug users: evidence from the evaluation of Vancouver’s supervised injection facility’, International
Journal of Drug Policy 19 (3), pp. 183–8.
Zobel, F. and Dubois-Arber, F. (2004), Short appraisal of the role and usefulness of drug consumption facilities (DCF)
in the reduction of drug-related problems in Switzerland: produced at the request of the Swiss Federal Office of Public
Health, Institut universitaire de médecine sociale et préventive, Lausanne. Available at http://www.bag.admin.ch/
evaluation/01759/02066/02343/index.html?lang=en (accessed 3 June 2009).
Zobel, F., Thomas, R., Arnaud, S., et al. (2003), Global evaluation of the Confederation’s measures to reduce drugrelated
problems (ProMeDro): fourth synthesis report 1999–200, Institut universitaire de médecine sociale et
préventive, Lausanne. Available at http://www.iumsp.ch/Unites/uepp/files/tox4_en.pdf (accessed 3 June 2009).
Zurhold, H., Kreuzfeld, N., Degkwitz, P. and Verthein, U. (2001), Drogenkonsumräume. Gesundheitsförderung und
Minderung öffentlicher Belastungen in europäischen Grossstädten, Lambertus, Freiburg.
Zurhold, H., Degkwitz, P., Verthein, U. and Haasen, C. (2003), ‘Drug consumption rooms in Hamburg, Germany:
evaluation of the effects on harm reduction and the reduction of public nuisance’, Journal of Drug Issues 33, pp.
663–88.
| < Prev | Next > |
|---|












