SAFER DRUG USE IN PRISONS
Drug Abuse
6 SAFER DRUG USE IN PRISONS Based on Trautmann / Barendregt ‘European Peer Support Manual’ (see References)
Because of the scarcity of injecting equipment, those inmates who continue to inject while in custody are likely to engage in very high-risk behaviours for transmission of blood-borne viruses, many of which they would not countenance outside prison. Because they have easy access to sterile syringes outside prison from drug services in most EU countries, many inmates experience a ‘hygiene relapse’ while in prison.
Injecting equipment may be obtained in prison by:
Bringing in ‘sawn off’ syringes, often anally or vaginally
Borrowing previously used equipment
Hiring previously used equipment
Stealing equipment from prison hospitals or clinics
Smuggling by visitors
Manufacturing injecting equipment from available materials
It is evident that using these devices can involve various health risks. Anecdotal evidence shows that this equipment sometimes may serve all drug-using inmates on a whole wing or even a whole prison. Injection equipment is sometimes used as currency and has a high price when in short supply. So why do prisoners use them? Because they are addicted and lack control, ignoring any precautionary measures for the time being.
Two additional answers may be:
To many prisoners the term ‘sharing’ is not clear. Many prison injectors only class using previously used equipment as sharing if it has been used very recently, or at the same time as they use it.
Inmates trust each other in reporting the status of their infections. HIV-infected prisoners use the syringe at last.
There is a need to reduce the incidence of sharing of injecting equipment in prison. Current and past policies to control drug use in prisons clash with the new public health imperative of preventing the spread of blood-borne viruses.
The World Health Organisation guidelines for prison HIV services (WHO 1993) say:
“All prisoners have the right to receive health care, including preventive measures, equivalent to those available in the community, without discrimination and in particular with respect to legal status or nationality.”
The guidelines go on to say:
“Preventive measures for HIV/AIDS in prison should be complementary to and compatible with those in the community. Preventive measures should also be based on risk behaviours actually occurring in prisons, notably needle sharing among injecting drug users and unprotected sexual intercourse.”
6.1 Syringes *8
Most heroin users in Europe take their drug by means of injection. There are also other drugs (e.g. cocaine, amphetamines, methadone) which are taken by injection. The HIV epidemic has stressed the importance of using clean injecting equipment. The best option therefore is:
Always use a new needle and syringe for each injection.
As the best option of prevention - always using a new needle and syringe - is generally not a realistic option in prisons, the next best or ‘better than nothing’ options will have to be applied. In the following procedures for cleaning needles and syringes are described that can be applied in these circumstances. Besides this, prison adopted procedures are also described, as there is limited access to cleaning materials or heater and boiling water in the prison setting.
Cleaning does not guarantee 100% safety. Syringes are especially difficult to clean so take your time.
The second best option that one can use is boiling the works.
Other alternatives are:
The bleach procedure
The iodine procedure
The alcohol procedure
Finally: even rinsing with cold water is better than doing nothing
Boiling injection equipment
This is the most time-consuming procedure but the safest as well. As a hotplate is available and use is allowed in many prisons this is a realistic procedure:
Material required: Hotplate, a pan, water.
Duration: If all equipment is at hand, boiling injection equipment takes around 15 - 20 minutes.
Procedure:
First rinse the needle with syringe with cold water twice by pulling up water through the needle and flushing it into the gutter or the toilet.
Detach (if possible) the needle from barrel, and pull out the plunger. Make sure no air bubbles are left. Put needle and syringe into boiling water for at least 15 minutes.
Let the parts cool down and put them back together again.
Before using, rinse the complete syringe again with cold water.
Advantages:
Required equipment is simple and harmless.
This is the only way of cleaning which protects against most infections (HIV, hepatitis B and C but also bacteria and moulds. Whether it also kills the hepatitis C virus is yet not clear.)
A spoon can also be disinfected by boiling it together with the syringe.
Disadvantages:
People think that putting the syringe in hot water for a minute is good enough. This is not true.
In Europe most drug users inject using disposable syringes. These syringes can only be boiled between one and three times. After that, the vacuum-seal of the syringe becomes deficient.
Some syringes will not stand being boiled for 15 to 20 minutes.
The bleach procedure
Only in a few countries do national recommendations and provisions exist regarding the use of disinfectants. Whilst the introduction of bleaching agents would be welcome in all prisons - since proper bleaching is better than doing nothing at all - experience of bleaching practices outside prison shows that they are idiosyncratic even when optimum conditions exist. The nature of the prison environment means that cleaning and bleaching of injecting equipment will often be unsatisfactory, simply because the resources and opportunity will not be available. It is recommended not to use ‘Natriumhypochlorit’ (NaHCIO) because of its chemical instability, so jodophore disinfectants are more effective (see next chapter). But using Natriumhypochlorit seems to be better than nothing at all. Dispensing bleach should also be accompanied with specific information during the reception phase of admission to the prison.
In Scotland, sterilising tablets are given to prisoners with instructions on how to use them for sterilising mugs, cutlery, razors, chamber pots and injecting equipment.
Material required: Use bleach (Natriumhypochlorid in household bleach) in the highest available concentration, cup or bowl.
Duration: If all equipment is at hand the bleach proce-
dure takes about 5 minutes.
Procedure: 2 x water ¨ 2 x bleach ¨2 x water.
Pre-rinsing: draw up cold clean water through the needle until the syringe is completely filled and then squirt it out in the gutter or toilet. Repeat this.
Draw up bleach through the needle into the syringe, add some air and shake for 30 seconds, then squirt it out. Repeat this and don’t forget to shake again for 30 seconds.
Rinsing: draw up cold clean water through the needle until the syringe is completely filled and squirt it out in the gutter or toilet. Repeat this.
Splashes: If your eyes or face are splashed with the liquid, rinse it off with fresh tap water to minimise irritation
Mixing: Mixing the liquid or tablets with other cleaning products may reduce their effectiveness
Advantage:
The bleach procedure is inexpensive and quick (about 5 min.).
Disadvantage:
The larger the amount of blood in the syringe, the greater the chance that the bleach procedure will not be safe. So pre-rinse well with water and do not forget to shake the syringe filled with bleach, thoroughly.
The limited tenability of bleach. As it reacts with oxygen, bleach loses its disinfecting quality after three to four weeks.
Bleach is not accessible in all European prisons and is not accepted as a substance for disinfection in all European countries. This is an indication that bleaching is not 100% safe.
Bleach can damage some types of syringes.
For maximum safety:
Take the syringe into parts after the disinfection and rinsing, and put it in a bath of bleach for one hour.
Shaking a syringe for 30 seconds does not seem very long, but in fact it is, especially when one is withdrawing and in need of drugs. It is instructive to shake a syringe for 30 seconds when one is not in need to get a sense of the timescale involved.
The iodine procedure
Material required: Iodine dilution.
This is used medically for the disinfection of hands, surgical materials and disinfection in surgery treatment. A suitable 100 gram ilu tion contains: 7.5g poly (1- vinyl-2 pyrro lidine) iodine complex with 10% available iodine (Mw 40000). A cup or bowl.
Duration: If all the equipment is at hand, the iodine procedure takes about 6 minutes.
Procedure: 2 x water ¨ 2 x bleach ¨2 x water.
Pre-rinsing: draw up cold clean water through the needle until the syringe is completely filled and then squirt it out in the gutter or toilet. Repeat this.
Draw up the iodine/alcohol dilution through the needle and let it work for at least 2 minutes and then shake well before squirting it out. Repeat this.
Rinsing: draw up cold clean water through the needle until the syringe is completely filled and then squirt it out in the gutter or toilet. Repeat this.
Advantages:
Relatively cheap and quick procedure
Iodine is a well-known and accepted substance for disinfection in surgical treatment
Little loss of quality of the syringe
Disadvantages:
The more blood that rests in the syringe the greater the chance that the iodine procedure will not be save.
People suffering from iodine allergy or malfunctioning of the thyroid (gland), should use this method only after additional thorough rinsing when disinfection is carried out.
Iodine produces yellow stains on skin and clothes.
For maximum safety:
Take the syringe to pieces after the disinfection and rinsing, and put it in a bath of iodine for one hour.
The iodine procedure is not as commonly used as the bleach procedure. The iodine solution mentioned above is approved in Germany as an appropriate substance to disinfect surgical material. A Dutch literature study by the RIVM (National Institute of Public Health and Environmental Hygiene) shows that there is no research data opposing the use of iodine. Iodine is handed out in some Austrian and Swiss prisons as part of a first aid kit and used to clean syringes.
The alcohol procedure Based on ‘The Safer Injecting Briefing’, (see Useful Websites, chapter 5.1)
Material required: Medical alcohol (ethanol, isopropanol or n-propanol). Alcohol for consumption is not suitable. Alcohol should at least be 70 to 80% strong (preferably clear spirits). A cup or bowl.
Duration: If all equipment is at hand, the alcohol procedure takes about 6 minutes.
Procedure:
Pre-rinsing: draw up the cold clean water through the needle until the syringe is completely filled and then squirt it out in the gutter or toilet. Repeat this.
Draw up the alcohol through the needle and let it work for at least 2 minutes. Shake it well before squirting it out in the gutter or toilet. Repeat this.
Rinsing: draw up cold clean water through the needle until the syringe is completely filled and then squirt it out into the gutter or toilet. Repeat this.
Advantages:
Quick procedure. Alcohol is tenable for a very long time.
Disadvantages:
Alcohol doesn’t completely disinfect everything 100%.
Alcohol severely affects the protection layer on the inside of the syringe. The plunger will therefore begin to stick and run less smoothly.
For maximum safety:
Take the syringe to pieces after the disinfection and rinsing, and put it in a bath of alcohol for one hour.
6.2 Injecting paraphernalia *9
The preparation and sharing of drugs tend to be overlooked as potential points of transmission for blood-borne disease. The exclusive focus on needles and syringes in the messages given to drug injectors has also encouraged the erroneous belief amongst users that, as long as needles and syringes are not directly shared, then they are safe. The infective amount of blood for getting infected with hepatitis B for instance may be 0.00004ml of blood, i.e. less than one five hundredth of a drop of blood. hepatitis B+C and HIV can potentially be passed on by any equipment which has been in contact with an infected person’s blood.
Due to the high risk of getting infected with hepatitis, all prison workers who are in contact with drug injectors should know about the details of the injecting process, in order to enable inmates to make changes to protect themselves. There is also a need to understand the ease with which any of the equipment involved in the preparation of an injection (including lighters, knives, etc.) may transmit for instance hepatitis C. Simple changes to the practice of preparation, such as using a personal area and washing hands before and after injecting, will significantly lower the risk of bacterial and viral infection.
Drug workers and prison health staff need to discuss all types of paraphernalia and the environment in which they are used, with injectors. Many of these are dealt with in detail in the following pages.
This section describes in detail the injecting equipment used, and infection risks through these injecting paraphernalia and cleaning processes. It also addresses the risks that are specific to particular substances.
In detention the paraphernalia needed to consume drugs are frequently in short supply because these items are seized during searches of cells as potential drug-consuming material. In general two or more prisoners consume drugs jointly so that there is a high risk of using - unintentionally or deliberately - materials that have already been used by one or several other persons and so may therefore be infected with bacteria or viruses. The trainings that have been held in prisons so far revealed that most of the participants have been unaware of this potential chain of infections and therefore have not taken any precautions. In the following section, the use of various materials and the risks involved are outlined:
Paraphernalia regularly used for injecting drugs include:
Spoons or other containers (for mixing drugs with water, etc.)
Water
Water containers
Alcohol swabs
Filters
The preparation surface
Acidifiers
Tourniquets
Other utensils, such as lighters, knives, etc.
All these paraphernalia are associated with the transmission of blood-borne viruses, most notably hepatitis B and C, although HIV transmission is a possibility.
The risk of infection from one separate injecting event is likely to be low, but repeated exposure to low-risk events may result in infection.
Spoons
Spoons are often used as a receptacle in which drugs are mixed (e.g. dissolved in water) prior to injection. Lending and borrowing of spoons amongst injectors appears to be a common behaviour.
Contact of the spoon with a needle previously used by another person (e.g. by drawing up the substance from the spoon together), may be enough to transmit some infections, such as hepatitis C.
Injectors should be encouraged to mark their spoons for easier identification and keep them for their sole personal use in a place to which other injectors do not have access.
For cleaning, spoons should be boiled, or cleaned with bleach, iodine or alcohol and rinsed thoroughly before use (see cleaning procedure for syringes). Similar precautions should be taken with other receptacles used for drug preparation, such as the base of emptied and dried soft drink cans.
Water/water container
In many cases water is used to prepare heroin for consumption and frequently the same water is used that was previously used for tentatively cleaning or rinsing syringes and needles to remove any blood residues, pollutants or obstructions. If the water used for dissolving the heroin was previously used to clean the virus-contaminated (due to protein residues) equipment of a drug consumer, the circle of infection is unintentionally closed. Drawing up from a common pot of water represents a risk for the transmission of hepatitis and HIV as another person’s used needle and syringe might have come into contact with the water source. Very small amounts of blood which will not be visible can transmit infection.
Sterile water for injection is the ideal option where it is available. This should be for personal use only and discarded afterwards. The bottle or container, once it has been opened, should not be kept for subsequent injection, as it will contain bacteria from the air, and may have been used by another person.
Water drawn straight from the tap is better than bottled water, distilled water or ‘pure bottled water’ which may have been exposed to bacteria in the air and kept warm for some time, and so are therefore likely to contain far more organisms.
If in the context of intravenous drug use a common water pot - e.g. for cleaning - is used and the water shall be disinfected, the water has to be boiled for fifteen minutes. HIV is killed sooner, but with 15 minutes you are on the safe side for hepatitis B and/or C.
Filter
Filters are generally used by injecting drug users to minimise the risks associated with injecting undissolved particles which may be contained in the drug solution.
In practice filters represent a considerable risk. In most cases, small pieces of (sometimes used) cigarette filter tips are used (or more rarely: cotton fabric, bandaging material, cotton wool, toilet paper, tampons, paper handkerchiefs). By means of these provisional filters the dissolved heroin is drawn up from the spoon into a syringe. In this way drug consumers want to avoid the risk from dirt particles, which become visible when the drug was boiled up but which are unrelated to the heroin, getting into the veins. Using a filter is meaningful considering that the heroin offered is generally diluted, a process which involves great risks. If no filters were used, the number of abscesses and damage to veins would rise significantly as would the number of cases of bacterially-induced endocarditis, a disease which - if untreated - rapidly develops into a life-threatening inflammation of the heart and which is supposed to cause early invalidity among injecting drug users.
Analyses carried out in Dutch institutes have shown that the residue that ‘sticks’ to each of these provisional filters, i.e. does not reach the syringe, amounts to about 0,0046 grams of heroin. Most of the drug consumers are aware of these residues and when the drug is in short supply, the more sparingly it must be used. Hence some drug consumers save the filters for further use. If they have run out of heroin, 10 or more of these filters - the emergency supply - may once again be boiled up in a spoon so that most of the drug residue contained in the filters can be used.
Health risks related to filters include:
The filters might be saved after injecting as they will contain a small amount of drug residue and then be reused later by the original injector or by others. This might spread blood- borne viruses and/or serious bacterial infection. This is especially true when filters are stored in a moist place as then they are - in a negative sense - an excellent breeding ground for bacteria: within 6 hours up to 8 million bacteria will ‘grow’ which later on contaminate the consumer´s veins, tissue, heart, etc. .
The reused filters are carriers of viruses if only one of the filters stored was contaminated by blood residues containing viruses. In moist conditions particularly hepatitis viruses survive for some time. Hence, if a prisoner reuses their own filters along with those of others to consume the heroin residues, they could unintentionally start a chain of (hepatitis) infections.
Filters may also have been in contact with needles used by different persons if more than one injector draws up from the same spoon
Loose fibres can be drawn up into the syringe, causing circulatory problems if injected. This is most likely to happen when cotton wool or clothing fibres are used.
Clean, unused cigarette filters, especially those intended for hand rolling, are probably the best option for provisional filters, but even these can cause problems if broken apart. The worst option is readily soluble filters, sometimes made out of toilet paper, paper handkerchiefs or tampons.
The only possibility for minimizing health hazards in the use of these provisional filters (e.g. cotton wool) is to dry the used filters for several days before boiling them up again. In this way the possibility of viral contamination can be reduced.
There are different types of commercial syringe filters on the market. Some of these are designed to filter out the bacteria which may cause skin infections and abscesses.
Although these filters may prove to be valuable, they should be viewed and employed with caution as they may:
Create a false sense of safety among injectors, wrongly believing that they will filter out all blood-borne infections - they won’t: viruses cannot be filtered out as they are inside blood cells
Be reused or shared in a similar way to home-made filters
Be so ‘fine-meshed’ that injectors consider them to be either too slow or so effective that they are removing too much of the drug from the solution
Block and burst under pressure because of the very small pore size.
Since 1997 a new kind of syringe is available on the market: the Swiss company Compet AG developed a new filter and prepared it for series production together with Braun. A membrane in the filter optimally filters all dirt particles bigger than 15 micron. The filter material is hard, i.e. it cannot dissolve and get into the veins. Its most important benefit, however, is that the filter is completely permeable by heroin. Therefore there is no reason for any drug users to collect (used) cigarette filters, boil them up and pass them on to others for drug consumption. By using the new filters at least one of several possible chains of infection can be eliminated.
Alcohol swabs
Alcohol swabs are used to clean the skin at the spot where drugs will be injected. Frequently drug users are careless about the use of swabs and several drug consumers use the same swab to clean the puncture spot before injecting the drug. Frequently the swabs are contaminated with blood from a previous user so that an open wound is easily infected. Whether or not the swabs’ alcohol content is sufficient to disinfect the blood material absorbed cannot always be clearly determined. This is particularly doubtful if the swab’s vacuum wrapping was opened a long time before use so that the swab dried out. There is no sterilising effect anymore because the alcohol in the swab volatilised.
This means alcohol swabs should only be used by one person, cleaning the skin spot in one go.
Another important issue is whether alcohol swabs are used accurately. This means that the skin is disinfected for at least 30 seconds. Even nurses and doctors often use them for less than 30 sec. In order to kill bacteria and virus on the skin it is absolutely necessary to disinfect the skin adequately. Alcohol swabs used to clean the spoons mean they are just cleaned rather than disinfected - but this is better than nothing!
Surfaces
If a surface on which substances are prepared for injection is contaminated with blood or with water from flushing out syringes, there is a risk of transmission of infection. Ideally, surfaces should be cleaned with bleach or detergent before injecting. If this is impossible under prison circumstances it would still be better than nothing to prepare an injection on something disposable, such as a newspaper or magazine. This will also serve to mark out a ‘personal area’ for injecting.
Acidifiers
Acidifiers are used to enable heroin base - which is manufactured principally for smoking, as opposed to heroin salt which is made for injecting - to be more easily dissolved into a solution for injecting.
They do not need to be used with the more refined hydrochloride form of heroin, i.e. heroin salt, as it is highly soluble in water. Nor need they be used in the preparation of other drugs such as cocaine hydrochloride, i.e. cocaine salt (although not in the form of crack, i.e. base cocaine) or amphetamine for injection.
Various acids such as lemon juice and vinegar are used for heroin preparation. Any acid already in liquid form may contain bacteria or become contaminated with hepatitis or HIV viruses.
Lemon juice, whether fresh or bottled, has been associated with thrush and other fungal infections within the body, which have been reported to cause loss of vision and blindness due to retinal damage (candidal endophthalmitis). It has also been associated with endocarditis and other conditions.
Powders such as ascorbic acid (vitamin C) or citric acid are thought to be the safest options. These however can cause irritation to veins and tissues, so the smallest amount possible should be used. The more acid the solution, the more irritant it will be. Ascorbic acid is probably less caustic than citric acid and may therefore cause less irritation
Tourniquets
Tourniquets should only be used if they are really needed. Many injectors, at least early in their injecting careers, will be able to easily access superficial veins without using tourniquets. If left in place for too long they can cause a limb to be deprived of its blood supply not loosening the tourniquet before injecting can also lead to dying off (through necrosis or gangrene) of the part of the body which is tied off in cases where the user loses consciousness due to overdosing.
If a tourniquet is not loosened prior to injection, excess pressure has to be used to get the solution into the vein, which can lead to leakage of the drug into the tissues or to rupture of the vein. If an injector is frequently complaining of ‘missed hits’, check that they are releasing the tourniquet before injecting.
If tourniquets are contaminated with blood and subsequently shared, they represent a hepatitis C transmission risk.
Various techniques can be used to help superficial veins become more accessible, including:
Clenching and re-clenching the fist
‘Windmilling’ the arm
Any vigorous exercise
Letting the limb hang down
Bathing the arm in warm water.
Environment
The environment in which injecting takes place can be a factor in the transmission of blood-borne viruses.
The risks associated with injecting will be reduced if there is adequate:
Privacy
Time
Lighting
Running water
Sterile injecting equipment.
For inmate injectors, few, if any of these may be available. For these injectors at least, some of the points mentioned can be obtained (in the cell, toilet or another room). Injecting with another person present lowers the risks of an undetected overdose, but will increase the risk of viral transmission if any equipment is shared.
One basic piece of advice is to wash your hands over an empty sink before starting to prepare a shot.
6.3 Preparing a shot *8 (Based on instructions given by L. Synn Stern.)
The next instruction is written from the perspective of the ideal situation. The conditions in prisons are far from that, so where possible alternatives are given.
Clean the spoon (or the bottom of a coke can) following the instructions under 6.1, with water.
Use clean water. Cold water from the tap is cleaner than warm water and running water is cleaner than still (dead) water. Cold water from the tap does basically have the same qualities as water taken out of a bottle (this is not true when the tap is giving water with particular qualities, e.g. high degree of iron or nitrate in it). Water in a bottle may have already been used and it should not be carbonated.
Make a new filter (from a cigarette filter, tampax etc.) with clean material and with clean hands for every shot. The most suitable filters are the specially manufactured type for infusion.
Ensure that the liquid in the syringe is transparent and without ‘dirt’. If not, cook, shake and filter once again. Dirt can cause serious problems, such as ‘the shakes’, cardiac diseases, abscesses and embolisms. Check that there are no air bubbles in the syringe.
For heroin base injectors, ascorbic acid (Vitamin C) is preferable to lemon juice.
6.4 Self-injecting *10 (Based on instructions given by L. Synn Stern.)
Use a new needle and syringe each time. At least use a new needle to avoid clogged or broken needles and infections (hepatitis B/C, HIV, bacteria)
Choose a different injection site each time, to avoid scars, bruises, abscesses, swellings, sunken veins or problems with blood circulation.
Find the biggest veins and switch veins each time. If this is impossible, find a new spot a least 2.5 cm (1 inch) from the spot you used last.
Clean the injection site with an alcohol swab and wait till the alcohol has evaporated. Then it is effective and doesn’t hurt when the needle is being inserted.
A tourniquet helps the veins to dilate. Use an elastic band which is easy to loosen e.g. knicker elastic. If you inject in your arm, first let it hang down to fill with blood and then tie off. Don’t tie off too tight or for too long.
If you do not succeed in finding a vein, untie the tourniquet, do some physical exercise and tie off once again. Make sure you can open the tourniquet before pulling the needle out. For instance: keep the pulled end of the tourniquet in your mouth. If you become too stoned your mouth will fall open and automatically the tourniquet unties.
Do not forget to remove the air from the syringe. Keep the syringe upright, if necessary flick any air bubbles out and push the piston carefully until no air is left).
It is safer to untie the tourniquet before pushing the plunger, because if you overdose (lose consciousness) with a tight tourniquet you will almost certainly lose that part of the body which is tied off. For many people this is not possible because if they untie the tourniquet they also ‘lose’ their vein. It is always useful to have someone with you, just in case.
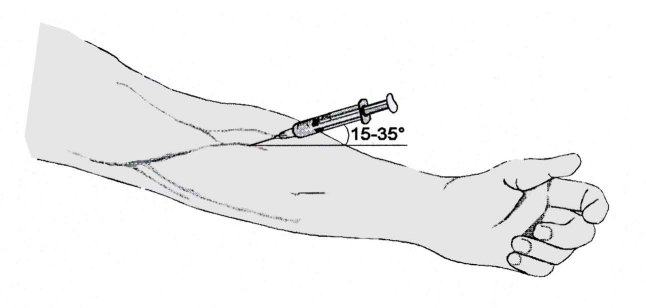
Insert the needle at an angle of 15° - 35° in the direction of your heart with the point of the needle pointing down. In this way the needle slides easily into the vein.
Veins don’t roll away if you pull them tight with a finger or the side of your hand: the needle is now between the tourniquet and the finger that holds your vein tight.
If you see dark red blood when you pull back the plunger, you are in a vein. If the blood is pink or the plunger is pushed back by itself, you have hit an artery.
When this happens immediately untie the tourniquet and pull out the needle. Press on the spot with a bandage for at least 5 minutes until you are sure it has stopped bleeding. Hitting an artery can cause serious problems, so medical help is advicable.
When you know you are in a vein push the plunger home slowly. Check several times if you are still in the vein by pulling back the plunger a little. With cocaine you may not notice if you are next to a vein. If the needle slips out of the vein during injecting, untie the tourniquet and choose another spot. The needle won’t clog easy if you draw up a little extra cold water. Don’t forget to remove the air.
When you are finished, and you did not yet, do it now, untie the tourniquet and remove the syringe in the oppo site direction to the way you have inserted it. Apply pressure to keep the injection site closed for a short while (for most people till the rush has finished), preferably with your arm or leg held up to prevent possible bleeding underneath the skin.
If you miss the vein or have subcutaneous bleeding, put on some ointment, (heparin/herodoid) or salted water and cover it with pressure bandages. Missed hits and subcutaneous bleeding can lead to abscesses.
Don’t forget to dispose of your used syringe in a safe way or exchange it for a clean one.
6.5. Alternative routes of administration *11 Based on Trautmann / Barendregt ‘European Peer Support Manual’ (see References)
Chasing the dragon
In some countries this route of administration has become more and more popular for using heroin. At first sight it seems a simple technique, but in fact it requires some practice to do it effectively.
Some heroin base is put on a strip of aluminium foil
The foil is heated under the heroin with a modest flame from a lighter
The heroin melts and the vapours which come off are inhaled through a little tube in the mouth
Advantages:
Material required is cheap and easy to obtain
Minimal risk of overdose
No risk for HIV infection. Small risks of other infection (only by sharing the tube one risks a hepatitis infection)
Disadvantages:
Requires good quality heroin
Only brown heroin, i.e. heroin base is suitable
Needs some practice to learn to use effectively. Errors can be expensive
Some adulterants of heroin can cause irritation of the air passages
The effectiveness of chasing the dragon works best when the heroin is diluted with caffeine.
Snorting and smoking
Due to bad quality of heroin (generally between 2 and 20% purity) and due to the relatively isolated position of the drug culture, chasing the dragon is not widespread in most European countries. In these countries the most common alternative to injecting heroin is snorting.
Prepare a tube of strong paper or take a straw
Chop the substance to a fine powder (using a razor blade on a mirror)
Make a fine line of the powder
Sniff it through the tube into the nose
Advantages:
Only requires cheap and easy to obtain materials u Less risky than injecting in terms of infections and overdoses
Disadvantages:
The drugs and possible adulterants can cause irritation of the nose
Also smoking heroin in cigarettes is not uncommon in several countries. The big disadvantage with this mode is the serious loss of heroin while smoking. Again, adulteration of the drug can cause health problems.
6.6 Syringe distribution in prison
Many objections have been put forward against the development of prison syringe exchange. These include arguments that:
It is condoning an activity that the prison does not allow
Needles could be used as weapons against either staff or other inmates
That it will increase the incidence of injecting
That those not currently injecting or using drugs at all will start to inject
Pilot prison syringe exchange programs operating in Switzerland, Germany and Spain demonstrated these projects to be successful: no threatening scenarios occurred, and the rate of needle sharing and the number of abscesses dropped significantly. Similar concerns about needle exchange were voiced initially about community projects yet were overcome. However, in talking about the prison population, politicians are usually very keen on being seen to be ‘tough on crime’ and relaxing the prison rules would, no doubt, be seized upon by sections of the media as ‘going soft on crime’.
It is clear that even many of the second-best solutions listed above are probably not realistic or pragmatic. The commonly voiced view that if injecting equipment was supplied, then needles would be used as weapons ignores the fact that many potentially infected syringes and needles are already circulating in most, if not all prisons. Many individual prisons and prison workers are committed to helping to limit the spread of blood-borne viruses. This work should be supported and assisted by the introduction of realistic resources and policies to help control the spread of viruses within prisons.
QUIZ- PLAY IT SAFE’
‘Safe sex’ and ‘safe drug use’ are inevitable in the prevention of HIV and other infections. What do you know about safe condom use and the cleaning of syringes? What do you know about accidents with used needles? Test your knowledge with this quiz.
1. Cleaning syringes with bleach and iodine is one hundred percent safe?
A. Correct
B. Incorrect
2. If you are afraid that the condom might tear, it is better to use two condoms over each other?
A. Correct
B. Incorrect
3. Bleach that is older than two years is no longer safe for cleaning syringes?
A. Correct
B. Incorrect
4. When cleaning syringes with bleach, the syringe must be shaken once and the bleach squeezed out through the needle?
A. Correct
B. Incorrect
5. If you accidentally prick yourself on a used needle, the wound must be sucked out?
A. Correct
B. Incorrect
6. When boiling syringes, only the needle needs to be boiled?
A. Correct
B. Incorrect
7. During foreplay, the use of a condom is not necessary?
A. Correct
B. Incorrect
8. When boiling syringes, the water must boil for at least 15 minutes?
A. Correct
B. Incorrect
9. When a condom is used, the penis must be withdrawn immediately after ejaculation?
A. Correct
B. Incorrect
10. With anal sex, where the penis penetrates the anus, an extra-strong condom is necessary?
A. Correct
B. Incorrect
QUIZ
RESULTS
Add up the figures from the answers that you gave.
1. A-0 B-1
2. A-0 B-1
3. A-1 B-0
4. A-0 B-1
5. A-0 B-1
6. A-0 B-1
7. A-0 B-1
8. A-1 B-0
9. A-1 B-0
10. A-1 B-0
0-5 points
Your knowledge is inadequate.
6-8 points
Your knowledge is pretty good but still needs improving.
9-10 points
You are well informed.
The correct answers to ‘Play it safe’ quiz:
1. Cleaning syringes with bleach and iodine is one hundred percent safe?
B - Incorrect. Just as with boiling, the cleaning of syringes with bleach and iodine is not one hundred percent safe. The only really safe way of injecting, is fixing with brand new equipment.
2. If you are afraid that the condom might tear, best use two condoms over each other?
B - Incorrect. Do not do this! The use of two condoms on top of each other increases the chances of tearing as the two condoms rub against each other.
3. Bleach which is older than two years is no longer safe for cleaning syringes?
A - Correct. When cleaning syringes with bleach the concentration must be at least five percent. After two years, the concentration will have decreased too much to be viable.
4. When cleaning syringes with bleach, the syringe must be shaken once and the bleach squeezed out through the needle?
B - Incorrect. The syringe should be filled with bleach two times, shaken, and the bleach then squirted out through the needle. Both times it is important that the syringe is shaken for at least thirty seconds.
5. If you accidentally prick yourself on a used needle, the wound must be sucked out?
B - Incorrect. Don’t ever do this! Do not suck out the wound but thoroughly let it bleed out. Afterwards, rinse with plenty of water and then disinfect with 70% alcohol. Contact the medical service after a ‘needle stick accident’ and also if an open wound has been in contact with blood, semen or vaginal secretion: an injection with antibodies within 48 hours can prevent an infection with hepatitis.
QUIZ
The chance of infection is very small, (less than 1 percent). However, lt a doctor if an AIDS test or treatment is necessary.
Tips: when picking up stray syringes, wear heavy gloves, and do not touch the needle.
6. When boiling syringes, only the needle needs to be boiled?
B - Incorrect. Not just the needle but also the syringe barrel and plunger could contain blood residue. Therefore, rinse everything first with cold water. In addition, everything has to be boiled. The best way is to place needle, syringe and plunger separately in a pan with boiling water. Make sure that no air bubbles are left behind.
7. During foreplay, the use of a condom is not necessary?
B - Incorrect. A condom is also essential during foreplay, since the HIV virus, together with semen, can also be transmitted by pre-ejaculate.
8. When boiling syringes, the water must boil for at least 15 minutes? A - Correct.
9. When a condom is used, the penis must be withdrawn immediately after ‘coming’?
A - Correct. When the penis gets soft, the condom may slide off. While withdrawing the penis, always hold on to the base of the condom and after use, tie a knot in it.
10. With anal sex, where the penis penetrates the anus, an extra-strong condom is necessary?
A - Correct. Because condoms tear faster with anal sex, extra-strong condoms with extra water-based lubricant are a ‘must’. Oil-based lubricants can damage the rubber of the condom and so lead to tearing.
6.8 High risk situations in a high risk environment
Overdosing on heroin or other sedatives
The most widespread drug in prison after tobacco and cannabis is heroin or other opiates. These are sedatives that effect the central nervous system (brain). The central nervous system regulates breathing and pulse. When overdosing on opiates the central nervous system reduces or stops the breathing functions and eventually the heart functions. Other sedatives, such as barbiturates, benzodiazepines and alcohol, produce similar symptoms.
High risk situations are:
The use of drugs when quality and purity are unknown. First try a small dose.
Purchasing drugs from unknown inmates.
The use of heroin after having taken excessive quantities of alcohol and/or tranquillisers. In these circumstances, one may easily lose consciousness and throw up. If this happens, the vomit can block the throat (see above).
Using the amount you were used to in the period before incarceration, after a clean period, or a period of reduced drug use in prison.
Using drugs alone. Nobody can give first aid in this situation.
Using heroin after treatment with an opiate antagonist (see below).
The following symptoms of overdosing on downers are:
Unconsciousness
Slow breathing
Slow pulse
What can you do?
Check if someone is really unconscious by screaming and shaking the person.
If not, try to wake them up any way you can.
The moment the person shows first signs of consciousness, keep them awake by forcing them to walk, talking, squeezing etc.
If the person does not regain consciousness or slips back into unconsciousness again, keep him alive with the kiss of life and, if necessary, heart massage (see following chapter). Have someone call a doctor or a (trustfworthy) prison officer. A doctor will probably give the person an injection with an opiate antagonist (Narcanti etc).
Fatal dilutions, mixing drugs and choking
Here are some additional risk factors:
Fatal dilutions
In order to maximize profits, illegal drugs are often cut with other substances. This is particularly true in prison-conditions. Sometimes the cut can be more dangerous than the drug itself and may leads to casualties.
Mixing drugs
Mixing drugs can be dangerous. A mix of opiates, tranquillisers and alcohol is common on the prison opiates scene. This combination frequently leads to dangerous situations such as overdosing.
Choking
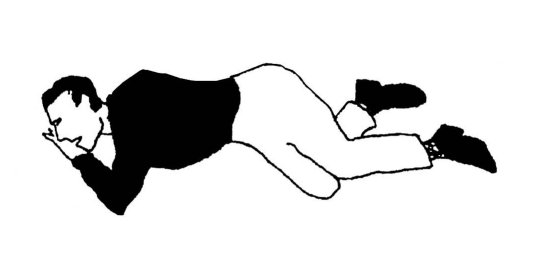
Choking can be one of the consequences of mixings drugs as mentioned above. If people fall unconscious they will sometimes throw up. To avoid choking, clear the mouth and throat (with a handkerchief, for example) and when their breathing and pulse is stable, put them into the recovery position.
6.9 First aid
Keeping people awake
If someone starts dozing off after having used drugs, you should try to keep that person awake to prevent unconsciousness. What can help is fresh air, making the person walk around, putting wet, cold towels on the neck and talking to the person. A good ‘fellow user’ should also protect his buddy from getting robbed to boot.
Keeping things calm
The proverb ‘’too many cooks spoil the broth” also applies here. No more than two people should take care of the person in distress.
In an emergency it is not important what substance and/or precisely how much of it was used, as first aid is always aimed at the symptoms. In other words, it doesn’t matter if it was an overdose from heroin, cocaine, or tablets, the emergency procedure is always the same.
Check vital functions
The vital functions are:
Breathing
Heart beat / blood circulation and u Consciousness
The other vital functions such as regulating the body’s metabolism or temperature cannot be influenced without medical help.
Check breathing
Hold your hand over the nose and mouth of the ‘patient’ and see if you can feel his breath, (maybe moisten your hand first), place your other hand on the chest and feel if it rises. An adult has to breathe 12 - 17 times per minute. Blue lips or strange sounds while breathing, similar to snoring, are cause for alarm.
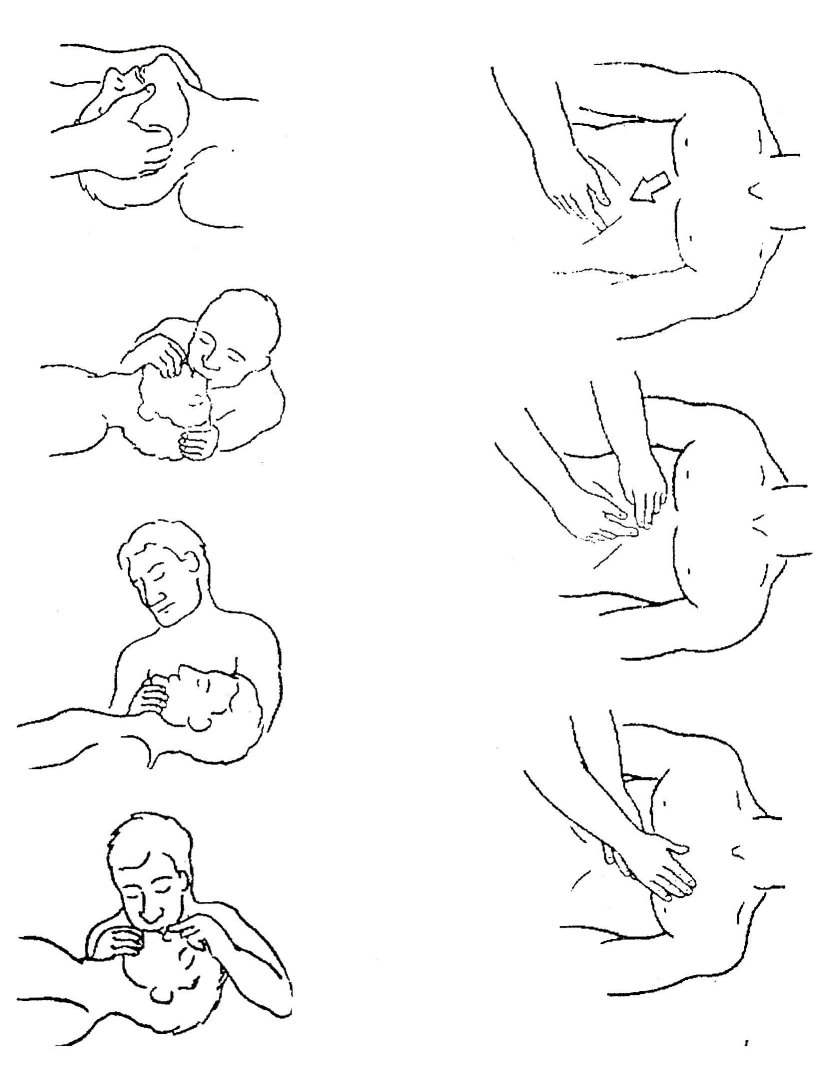
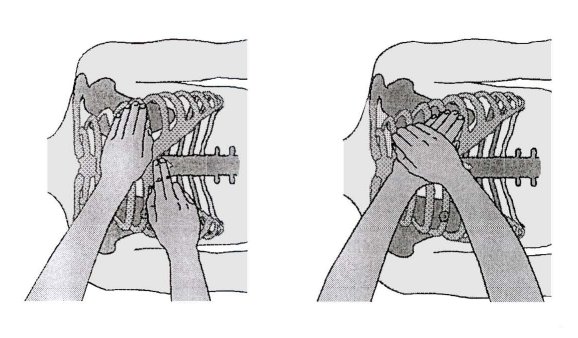
Clear the airways
First of all, tilt the person’s head back as far as possible (see illustration). This prevents that the tongue blocks the windpipe. Then check for any foreign objects (dentures), blood or vomit inside the mouth. If there is something inside the mouth, turn the person’s head sideways and clean mouth and mouth cavity with a handkerchief as well as you possibly can. Afterwards, immediately reposition the head to the position shown in the illustration.
Artificial respiration
If the person still does not breathe, breathe into him 3 times. Tilt the person’s head back even further, cover his mouth, take a deep breath and slowly breathe the air into his nose. If the nose is bloody or blocked in any other way, breathe your air into the person’s mouth.
Check the pulse
You can feel the pulse on the wrist, but more efficiently on the neck (at the side of the neck, next to the thyroid gland). An adult has an average pulse rate of 60 to 80 beats per minute.
Alternate between artificial respiration and heart massage (CPR)
If you can’t detect breathing or pulse, artificial respiration and heart massage will have to be administered in turn. Always begin with artificial respiration (to get oxygen into the blood) and then alternately breathe into the person’s mouth twice and administer heart massage (chest compression) 15 times.
Emergency drill
In an emergency, everybody tends to be excited. Therefore it is useful to practice your first aids skills every now and then, based on the following routine.
Check breathing
Breathing is adequate ? â yes â stable side position
ä
no
ä
Clear airways
Place body in flat position. Remove any objects from mouth (cavity), tilt head back as far as possible, lift lower jaw.
Breathing is adequate ? â yes â stable side position
ä
no
ä
Breathe into him 3 - 5 times
Breathing adequate now? â yes â stable side position
ä
no
ä
Check pulse
Pulse present ? â Yes â continue art. respiration
ä
no
ä
Continue artificial respiration and external heart massage (CPR)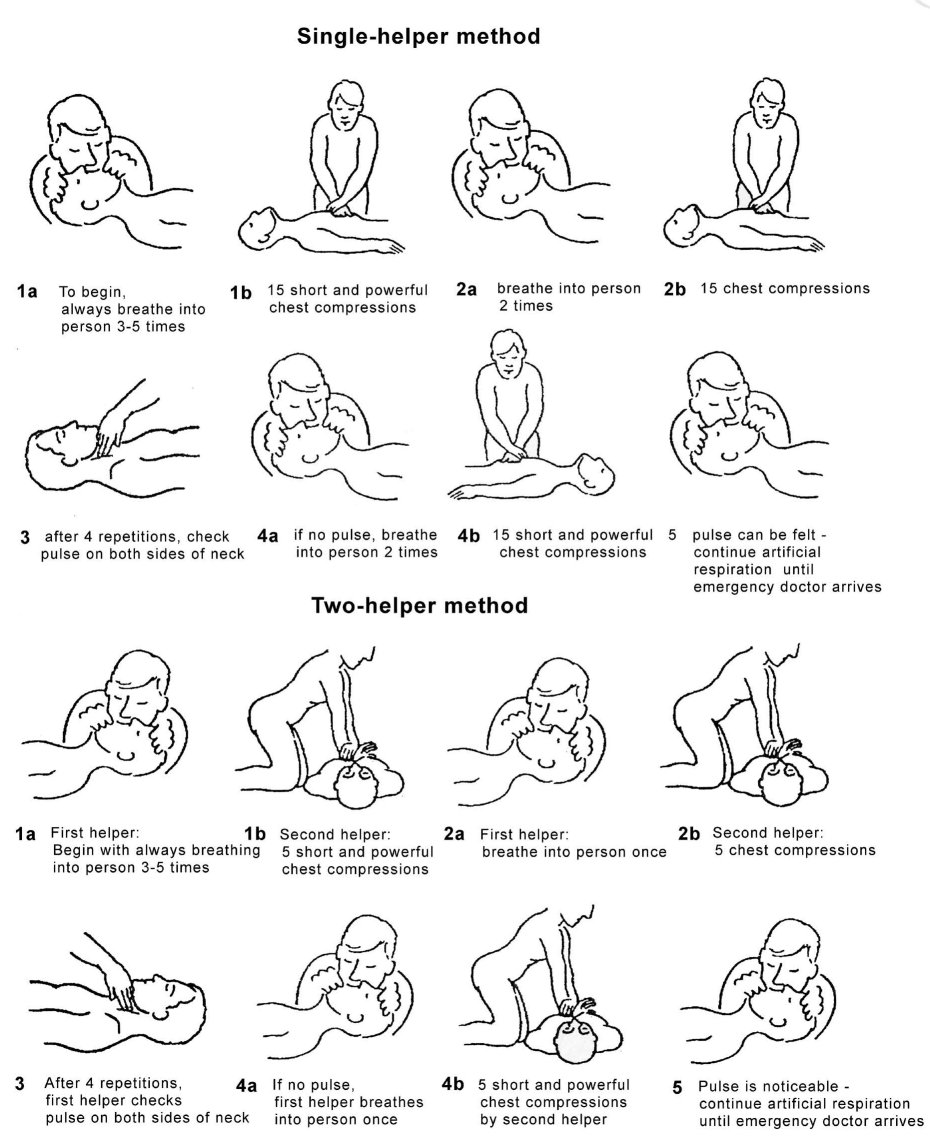
Heart massage
Lay the overdose victim on their back on a hard surface.
Put the forefinger on the solar plexus and the other forefinger close above it.
Then put the ball of the first hand next to ‘second’ forefinger on the chest. This is the correct spot. Next, lay the ‘second’ hand over the first one.
Bend vertically over the victim with your arms stretched.
The chest is now pushed in short, firm strokes (4cm) towards the spinal column. Release pressure on the chest immediately but the keep hands in the same position.
Repeat the pushes from 60 to 80 times per minute.
If victim still has no pulse and is not breathing and you are alone:
Start with 3 to 5 breaths into the victims lungs,
then, give 15 pushes on the chest, 2 more breaths, then 15 more pushes.
Check the pulse on the artery in the neck after 1 minute. Remember to check both sides!
If there is still no pulse, continue the heart massage. If there is a pulse, continue the breathing until help arrives.
Tip: The kiss of life and heart massage should be practiced before doing it for real. This exercise could well be organised as part of a peer support initiative, for example by inviting somebody from the emergency room or a medical doctor from a drug service.
QUIZ WHAT DO YOU KNOW ABOUT OVERDOSE?’
This chapter regularly mentions the word ‘overdose’. What is an overdose? And what must be done in the case of a heroin or cocaine overdose? Test your knowledge with this quiz.
1. A heroin overdose is always fatal within minutes?
A. Correct
B. Incorrect
2. Giving a shot of salt water helps to combat a heroin overdose?
A. Correct
B. Incorrect
3. For someone not used to heroin, 0.2 gram of heroin can be deadly.
A. Correct
B. Incorrect
4. In case of a cocaine overdose, the best thing to do is to swallow sleeping pills or tranquillizers as quickly as possible?
A. Correct
B. Incorrect
5. When dying from a heroin overdose, the user eventually dies from suffocation?
A. Correct
B. Incorrect
6. Taking sleeping pills or tranquillizers can increase the risk of a heroin overdose?
A. Correct
B. Incorrect
7. A heroin overdose does not lead to death as often as a cocaine overdose?
A. Correct
B. Incorrect
8. A cocaine overdose can cause a heart attack?
A. Correct
B. Incorrect
9. During an epileptic seizure due to a cocaine overdose, you must try to keep open the mouth by inserting an object?
A. Correct
B. Incorrect
10. The combination of heroin and benzodiazepines increases the chance of a cocaine overdose?
A. Correct
B. Incorrect
QUIZ
RESULTS
Add up the figures behind the answers you gave.
1. A-0 B-1
2. A-0 B-1
3. A-1 B-0
4. A-0 B-1
5. A-1 B-0
6. A-1 B-0
7. A-0 B-1
8. A-1 B-0
9. A-0 B-1
10. A-1 B-0
0-5 points
When an overdose occurs, quick, precise, correct action is important. Knowing what to do can be a matter of life and death. Unfortunately, your knowledge is inadequate.
6-8 points
You are quite well informed but need further improvement.
9-10 points
You are well informed.
The correct answers to ‘What do you know about overdose?’ quiz:
1. A heroin overdose is always fatal within minutes?
B - Incorrect. A heroin overdose can be fatal quite quickly (in a few minutes) but most of the time it takes longer for actual death to set in. In any case, action always needs to be taken quickly.
2. Giving a shot of salt water helps to combat a heroin overdose?
B - Incorrect. That administering a shot of salt water helps, is a myth.
Individuals suffering from overdose must be woken up and kept awake. This might be achieved by slapping them in the face, pinching them hard below the collar bone or splashing cold water in their face. If you do not succeed in your wake-up attempts, call an emergency number as quickly as possible.
3. For someone not used to heroin, just 0.2 gram of heroin can be deadly?
A - Correct. 0.2 gram can indeed be deadly for someone who normally does not use heroin. This is also true in individuals who have been ‘clean’ for a while, when a relatively small amount of heroin can induce an overdose.
4. In case of a cocaine overdose, the user should swallow sleeping medicines or tranquillizers as quickly as possible?
B - Incorrect. The agitation that follows an overdose of cocaine could indeed be combated with benzodiazepines, but the individual should not self-medicate. Due to the slow absorption by the blood, the effect of sleeping medicines and tranquillizers is delayed. In a panic situation, the person could easily take too many pills and suppress their breathing.
5. With a heroin overdose, the user eventually dies of suffocation?
A - Correct. During a heroin overdose the brain gradually stops functioning. This suppresses breathing and allows moisture to enter and collect in the lungs, resulting in an even smaller supply of oxygen. As a result, suffocation is the greatest danger with a heroin overdose.
6. Taking sleeping medicines or tranquillizers can increase the risk of a heroin overdose?
A - Correct. When heroin is used together with benzodiazepines and tranquillizers, one can fall into a coma more rapidly.
7. A heroin overdose does not lead to death as often as a cocaine overdose?
B - Incorrect. It is precisely the other way round: A cocaine overdose is less likely to be fatal than a heroin overdose. This does not mean however, that in case of a cocaine overdose, speedy action is not necessary.
8. A cocaine overdose can cause a heart attack?
A - Correct. An overdose of cocaine can manifest itself in two ways:
1. chest pains and 2. epileptic seizures. In the first case, the heartbeat and blood pressure rise rapidly, which can lead to a heart attack.
9. During an epileptic attack due to a cocaine overdose, you must try to keep open the mouth by inserting an object?
B - Incorrect. Putting something in the mouth does not help and might cost the helper a few fingers. It is also not good for the teeth of the victim. Much better to call an emergency number and protect the heavily convulsing victim by laying them somewhere on the ground where they cannot get hurt. Put a pillow or jacket under their head.
When the convulsions have stopped, put them onto their side in the recovery position with the upper leg bent and the lower leg straight, and the head straight or bent slightly backward.
10. The combination of heroin and benzodiazepines increases the chance of a cocaine overdose?
A - Correct. With heroin and benzodiaepines in the blood, the cocaine user feels very relaxed, which makes a second helping of cocaine seem very tempting. This sense of relaxation, however, is false. In reality, the heart is working overtime and the next ‘line’ could well be the last.
6.10 Drug use after release - health warning
An English study found out that 86% of interviewed drug users report some form of drug use within four months after release, so the impact of prison does not end at the time of release. The first two-weeks post-release is particularly dangerous, with death from drug overdose being eight to eighty times that of community
levels (Seaman / brettle 1998). The reason is that drug users in prison use drugs less frequently and in smaller quantities than they do outside.
Very few prisons respond to these health risks during their preparation for release. The reason is a fear of being too pro-active in talking about relapse after release. For many prisoners, however, we know that this is the case. There are some good examples of talking about this - and this example from Scotland shows one way to deal with it.
Congratulations!
Getting out of a jail probably feels like the best thing that’s happened to you for a long time. You may be thinking about having a party. If so, for your own sake, and that of your family, read on.
Drugs
In the last few years, users have been dying shortly after release from jail. The chances are that drugs outside are available in greater quantity and better purity than any that you may have had recently. Reducing drug use, even for a short time, means your body can’t cope so well with drugs anymore. This means that if you use drugs after release you may be in danger of overdosing, losing control, suffering brain damage or even death. You must use less on release
What should I do?
Ideally, get a life and stop using drugs, but if you must use drugs then:
Use less: which will also save your money
Use carefully and take care of your health and safety
Use with a friend who can watch out for you if things go bad tell them what this leaflet says
What if I overdose?
Before it is too late and you slip into a coma:
Get to a phone, ask for an ambulance. Tell them were you are and what you have taken
If you are with a friend, make sure they know what to do
Get yourself into the recovery position
Drugs from a doctor
If you are taking prescription drugs such as methadone or Valium®, your GP should give you less than before to reduce the risk of overdosing. Remember, prescribed drugs can be just as dangerous as street drugs if used incorrectly. Don’t ‘top up’ other drugs - the mixture could kill you.
Alcohol
If you haven’t had a drink for a while, it is like having your first ever drink again, so take care. Mixing drugs and alcohol could be fatal, so leave the cocktails to James Bond!
If you stopped injecting inside, do yourself a favour and don’t start again. If you can’t stop, seek advice from your GP or a drugs information service.
Remember: sharing works can kill you, so:
Do get clean needles from a needle exchange
Don’t share works
Don’t share cleaning water, filters, spoons, mixing liquids, etc.
Don’t share by back or front loading
Do remember other users may be infected, so avoid unprotected sex, blood spills, razors, etc.
Do use a smaller amount if you must s
Last Updated (Thursday, 06 January 2011 20:52)












