4.2 Bhutan
| Reports - Rapid Situation and Response Assessment South Asia |
Drug Abuse
4.2 Bhutan
4.2.1 Sample description
In Bhutan, 200 drug users ( 2% of the total sample of 9,465 drug users from South Asian countries) participated in the rapid assessment. Table 8 describes the socio-demographic characteristics of the drug users from Bhutan.
Half of the drug users (50°/0) who participated in the survey were in the age group of 21-30 years with a median age of 22 years (range 12-47). Only a small proportion of female drug users (6%) were recruited for the assessment. Sixteen percent of the drug users were married, a small number of them (3%) illiterate and nearly a fourth (24%) of the users were employed.
4.2.2 Drug use and risk behaviours
Table 9 describes the types of drugs used by the ever and current users. In terms of ever use, alcohol and cannabis were the most commonly used drugs. Majority of drug users were currently using alcohol (75%, followed by cannabis (67%) and heroin (11%. Users were initiated to alcohol and cannabis before the age of 17 years and the age of onset for opioids like heroin, propoxphene and buprenorphine was after 20 years.
Of the 200 drug users that participated in the assessment in Bhutan, 174 (87%) used drugs always or at times in groups. A third of the drug users (34%) used drugs with more than five friends. Changing drug using groups was common and was reported by 45% of the drug users. The median frequency of drug use in the sample was three (range: 1-24).
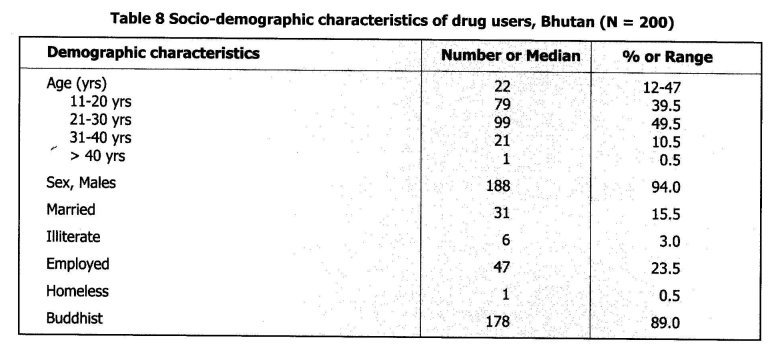
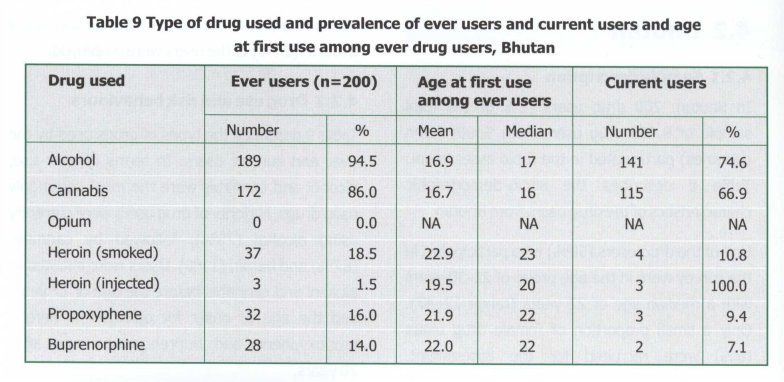
Table 10 describes the drug use related characteristics of the injecting drug users (N = 37). About a fifth (19%) of the drug users injected cocktail of drugs and there are no current drug injectors. Most (89°/0) of the drug users switched to injecting from non-injecting methods of drug administration. Lending of syringes and needles was common and reported by 43% of the participants during the last injection episode. Nearly three-fourths (73°/o) of the drug users reported cleaning their injection equipment before using with others during the last time they injected with others. Indirect sharing like sharing injection related paraphernalia (cooker, cotton, water and ampoules) was reported by 45°/o of the drug users. Nearly a fifth (19°/0) of the drug users reported abscesses during the past 6 months. Eighty-four percent of the drug users have stopped injecting and reverted back to non-injecting method of administration of drugs.
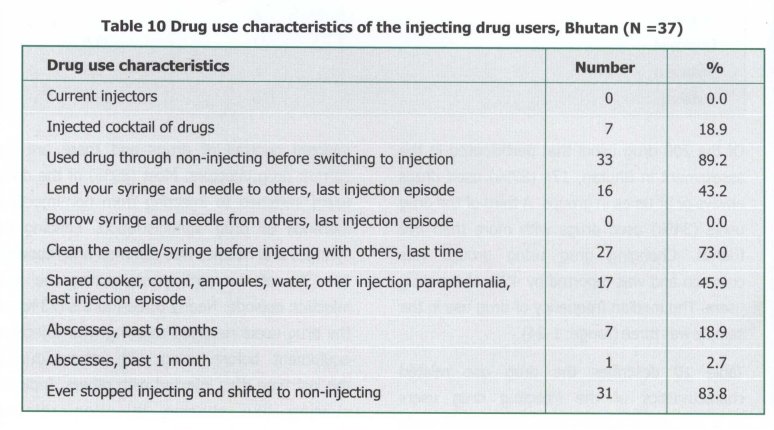
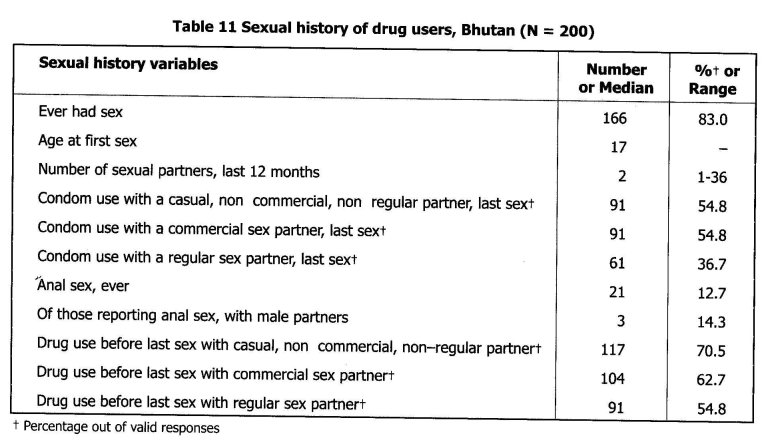
Table 11 describes the sexual history behaviour of the drug users who participated in the assessment. Most (83%) of the participants had sexual experience and the median age at first sex was 17. During the past year, the participants had a median number of two sexual partners (range 1-36). The proportion of participants reporting condom use with different sex partners during the last sexual act were: casual, non-commercial, non-regular partners (55% commercial sex partners (55°%; and, regular sex partners (37°%. Thirteen percent of the drug users reported anal sex and 15% of the drug users reporting anal sex had a male partner. Drug use before the last sex with casual, non-commercial, non-regular partners was common (71%), followed by with commercial sex partners (63%) and regular sex partners (55%).
4.2.3 Adverse health consequences
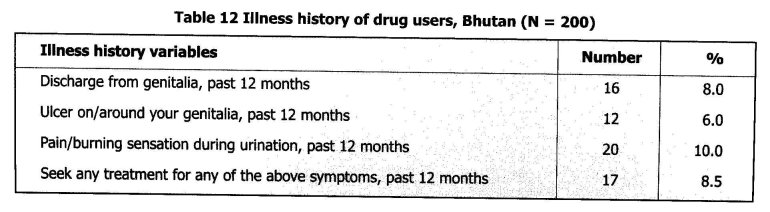
It can be observed from Table 12 that the participants reported the following symptoms related to sexually transmitted infections during the past 12 months: discharge from the genitalia (8°/0); ulcers on/around genitalia (6°/0); and, pain/burning sensation during urination (10%). Only 9% of the drug users sought any treatment for any of the above symptoms during the past year.
4.2.4 Knowledge and attitude in relation to HIV/AIDS
Variables related to knowledge and attitudes to HIV/AIDS of the drug users who participated in the study are described in Table 13. Most (98%) of the drug users were aware of HIV/AIDS. The knowledge of HIV transmission among the participants were: through contaminated injection equipment (93%1); by blood transfusion from an infected person (96°/0); from HIV infected mother to her unborn child (86%); and, through breast-feeding by a HIV infected mother (41°/0). Only a small proportion (8%) of drug users believed that they could recognise an HIV infected person by appearance. About two-thirds (66°/0) of the drug users knew that condoms protect against HIV. Despite high levels of knowledge related to HIV transmission, only a third (34%) of the drug users believed that they were at-risk of getting infected with HIV. Thirty-nine percent of the drug users had been tested for HIV; among those not tested as yet, more than a half (54°/0) desired to undergo HIV testing. Majority of the drug users were of the opinion that they would share the results of their HIV test with their regular partner if tested positive (65%) or negative (62%). Less than a fourth (24%) of the drug users had been treated ever for drug dependence. About two-thirds (65°/0) of the drug users had been approached by someone to provide HIV prevention information.
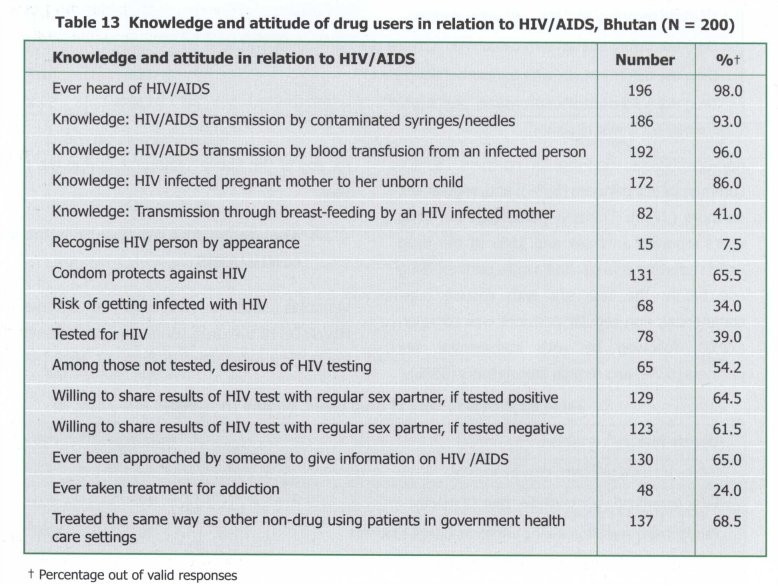
Many drug users believed that they would be treated differently from the non-drug using persons in the health care settings. More than two-thirds (69%) of the drug users were of the opinion that they would be treated as well as the non-drug users in government health care settings.
4.2.5 Regular sex partners of drug users
A total of 23 regular sex partners were recruited and completed a rapid situation and response assessment questionnaire. The median age of the regular sex partners was 22 years (range 17- 33 years). Forty-four percent of them were married and only a small proportion (13%) of them were illiterate. More than a three-fourth of the regular sex partners of drug users (78%) were employed. Nearly a half (48°/o) of the regular sex partners ever used drugs. Only 39°A) of the regular sex partners had used condoms during the last sexual act. Nine percent of the regular sex partners used drugs before their last sexual act. Thirteen percent of the sex partners reported anal sex. White vaginal discharge (13%), ulcers on the genitalia (13%) and pain/burning sensation while passing urine (17%) was not uncommon. Most (83°/0) of the sex partners were aware of HIV/AIDS but only 35% of the regular sex partners believed that they were at-risk for acquiring HIV. Nearly two-thirds (65%) of the sex partners believed that condoms protected against HIV infection. A small proportion (13°/o) of the sex partners had undergone HIV testing.
4.2.6 Recommendations
• As most of the drug users were literate, appropriate HIV prevention IEC materials should be developed to reach out to the drug using populations.
• As most of the IDUs used heroin by non-injecting method before transiting to injection, interventions to prevent transitions to injecting should target the non-injecting drug users.
• IDUs often lent syringes and needles; reducing injection related risk behaviours of drug users is critical to halt the escalating HIV among IDUs. Indirect sharing like sharing of injection paraphernalia was common and this needs to be addressed in order to reduce the transmission of blood borne viruses like hepatitis C.
• Many drug users were young persons between 21-30 years of age and were sexually active with a median number of two sexual partners. Despite the knowledge that condoms protect against HIV, condom use with regular sex partners was low and nearly a half of them had not used condoms during the last sexual act with commercial and casual sex partners. Interventions targeting drug users should always target sexual behaviour and promote consistent condom use with all sexual partners.
• Drug use before sex with casual and commercial sex partner was common and since drug use can compromise safe sex, this aspect should be considered in HIV prevention interventions.
• Symptoms of sexually transmitted infections were not uncommon; screening for STIs and effective STI care should be integral components of HIV prevention efforts for drug users.
• As nearly a fifth of the drug users had abscesses, comprehensive interventions for drug users should as well include primary medical care of managing abscesses.
• Most were aware of HIV and many are knowledgeable about needle related HIV transmission, unsafe blood transfusion and mother-to-child transmission; but, the knowledge relating to HIV transmission through breastfeeding was inadequate.
• Two-thirds of the drug users did not believe that they are at-risk of getting infected with HIV and hence enhancing the risk perception is crucial. There is a need to provide HIV testing for the drug users given the fact that most drug users had not been tested for HIV but among those not yet tested more than a half desired to undergo HIV test.
| < Prev | Next > |
|---|












