Heroin Addiction - A Metabolic Disease
Drug Abuse
Heroin Addiction - A Metabolic Disease
Vincent P. Dole, MD and Marie E. Nyswander, MD, New York
Arch Intern Med;Vol 120, July 1967
(An emulation of the original article)
THE METHADONE Maintenance Research Program began three years ago with pharmacological studies conducted on the metabolic ward of the Rockefeller University Hospital. Only six addict patients were treated during the first year, but the results of this work were sufficiently impressive to justify the trial of maintenance treatment of heroin addicts admitted to open medical wards of general hospitals in the city.
A simple, and somewhat arbitrary procedure was established. Addicts applying for the methadone program were accepted if they met the following criteria: age between 20 and 40, a history of at least four years of "mainline" heroin use with repeated relapses after withdrawal treatment, absence of major complications (psychosis or serious medical illness, disabling addiction to barbiturates or alcohol), and absence of compulsion (eg, acceptance of the treatment not a condition of probation or parole). After entering the program the patients were admitted to a hospital for six weeks, during which time they were given careful medical and social examinations and were gradually stabilized on a blockading dose of methadone
Methadone therapy was started in low dosage (10 to 20 mg/day in divided portions) and increased slowly over a period of four to six weeks to avoid narcotic effects.
After the patients had reached the stabilization level (80 to 120 mg/day) it was possible to maintain them with a single, daily, oral ration, without further increase in dose.
At the end of the six weeks of hospitalization the patients were discharged to outpatient clinics where they received their daily methadone, and gave urine specimens to be analyzed for drugs. The stations were established either in the outpatient area of a hospital or in rented offices located in the community.
No specific psychiatric treatment was provided in the routine, but counseling was available to any patient with a psychiatric problem. There has, however, been very little need for psychotherapy, and no indication that structured group therapy would contribute to rehabilitation.
The emotional problems of the patients after stabilization on methadone have been diversified and related to external situations (eg, jobs, school, family). It must be emphasized that the absence of routine psychiatric treatment did >not stem from indifference or lack of clinical resources; all patients have been seen by qualified psychiatrists on admission and, informally, at frequent intervals thereafter.
The close association of lay and professional members of the staff ensured that any major emotional problem manifested by a patient would have been brought to the attention of a staff psychiatrist. The lack of formal psychotherapy in the treatment program thus reflected the experience of the professional staff that routine psychotherapy was not needed for rehabilitation of the patients that we had stabilized on methadone.
Of 1,007 applicants interviewed during the past 14 months, 60% were accepted, 35% were rejected because of age or other departure from the criteria listed above, and 5% lost interest after the first interview. At the time of this report 304 patients have >been admitted to treatment, and 423 are on the waiting list (of whom 295 have been definitely accepted, and 128 are awaiting interviews). Although no effort has been made to recruit additional patients, we are now receiving approximately 35 applications per week from addicts on the street, and the rate is increasing. With >present facilities we can admit only seven per week and therefore have a growing waiting list.
Of the 304 patients admitted to treatment 91% have continued in the program, 8% were discharged because of behavioral problems unrelated to heroin addiction, and 1% left voluntarily. Approximately 70% of the patients who have been in the program for six months or longer are employed or in school; the remaining patients, although not yet socially productive, have at least ended heroin usage and the related antisocial behavior.
The dramatic improvements in social status of patients on this program have exceeded expectations. The study started with the hope that heroin-seeking behavior would be stopped by a narcotic blockade (and this has proven to be true), but it certainly was not expected that we would be able to retain more than 90% of the patients and that almost three fourths would be socially productive and living as normal citizens in the >community after only six months of treatment. Prior to admission almost all of the patients had supported their heroin habits by theft or other antisocial activities. Further handicapped by the ostracism of the community, slum backgrounds, minority group status, school dropout, prison records, and antisocial companions, they had seemed poor prospects for social rehabilitation.
The unexpected response of these patients to a simple medical program forced us to reexamine some assumptions that we brought to the study. Either the patients that we admitted to treatment were quite exceptional, or else we had been misled by the traditional theories of addiction.If, as is generally assumed, our patients long standing addiction to heroin had been based on weaknesses of character;either a self-indulgent quest for euphoria, or a need to escape realityit was difficult to understand why they so consistently accepted a program that blocked the euphoric action of heroin and other narcotic drugs, or how they could overcome the frustrations and anxieties of competitive society to hold responsible jobs.
There was nothing to suggest that the patients had been atypical addicts prior to treatment, except possibly the fact that they had applied for treatment without legal compulsion. In age distribution, ethnic backgrounds, previous arrests, and histories of relapse after detoxification, the patients met all the criteria of ordinary street addicts; there was no significant feature of their histories that could be recognized as different from the histories of addicts coming to the general detoxification service. None of the physicians in the many hospitals (federal, state, municipal, and private) in which they had previously been treated by detoxification had noted any especially favorable signs. Moreover, some of the patients came to the program motivated by the mistaken belief that maintenance would provide a legal euphoria. Even these patients have persisted with the blockade treatment after finding that they were wrong. Others, skeptical after many failures of detoxification and psychotherapy, applied in desperation hardly a stable motive to sustain a long range program of rehabilitation - yet they too, have stayed.
With 276 patients now living socially acceptable lives with methadone blockade and with many more street addicts waiting for admission, the question as to whether the patients are exceptional is no longer a practical issue. Exceptional or not, the patients are sufficiently numerous and have responded well enough to treatment to justify continuation of the program. The theoretical question however remains: Is addiction caused by an antecedent character defect and does maintenance treatment merely mask the symptoms of an addictive personality. The psychogenic theory of addiction would say so. This theory has a long history - at least one hundred years;and is accepted as axiomatic by many people. What, then is the evidence for it?
Review of the literature discloses two arguments to support psychogenic, or character defect, theory: the sociopathic behavior and attitude of addicts, and the inability of addicts to control their drug-using impulse. Of these arguments the first is the most telling. Even a sympathetic observer must concede that addicts are self-centered and indifferent to the needs of others. To the family and the community the addict is iresponsible, a thief, and a liar. These traits, which are quite consistently associated with addiction, have been interpreted as showing a specific psychopathology. What is lacking in this argument is proof that the sociopathic traits preceded addiction.
It is important to distinguish the causes from the consequences of addiction. The decisive proof of a psychogenic theory would be a demonstration that potential addicts could be identified by psychiatric examination before drug usage had distorted behavior and metabolic functions. However, a careful search of the literature has failed to disclose any study in which a characteristic psychopathology or "addictive personality" has been recognized in a number of individuals prior to addiction. Retrospective studies, in which a record of delinquency before addiction is taken as evidence of sociopathic tendencies, fail to provide the comparative data needed for diagnosis of deviant personality. Most of the street addicts in large cities come from the slums, where family structure is broken and drugs are available. Both juvenile delinquency and drug use are common. Some delinquents become addicted to narcotic drugs under these conditions while others do not. There is no known way to identify the future addicts among the delinquents. No study has shown a consistent difference in behavior or pattern of delinquency of adolescents who later become addicts and those who do not.
Theft is the means by which most street addicts obtain money to buy heroin and therefore is an inevitable consequence of addiction. For the majority this is the only way that they can support an expensive heroin habit. The crime statistics show both the force of drug hunger and its specificity: almost all of the crimes committed by addicts relate to the procurement of drugs.
The rapid disappearance of theft and antisocial behavior in patients on the methadone maintenance program strongly supports the hypothesis that the crimes that they had previously committed as addicts were a consequence of drug hunger, not the expression of some more basic psychopathology. The so-called sociopathic personality is no longer evident in our patients.
The second argument, that of deficient self-control, is more complicated since it involves the personal experience of the critic as well as that of the patient. It would seem that the moralists, having won their own struggles for self-control, measure the character of others by what they presume they would do if addicted. What is not clear in this judgment is whether the critics and the addicts have been subjected to equal temptations. It is not necessarily a sign of good character to dislike drugs. Many nonaddicted criminals tried narcotics in adolescence without becoming addicted. Presumably, the experience was not sufficiently rewarding for them to continue usage; in other respects these individuals may be quite deficient in moral standards. Conversely, the critics who are most contemptuous of addicts are those who were not exposed to narcotic drugs in adolescence.
Moralists generally assume that opiates are dangerously pleasant drugs that can be resisted only by strength of character. The pharmacology is somewhat more complicated than this. For most normal persons morphine and heroin are not enjoyable drugs, at least not in the initial exposures. Given to a postoperative patient these analgesics provide a welcome relief of pain, but addiction from such medical use is uncommon. When given to an average pain-free subject, morphine produces nausea and sedation but rarely euphoria. What, then is the temptation to become an addict? So far as can be judged from the histories of addicts, many of them found the first trials of narcotic in some sense pleasurable or tranquilizing, even though the drug also caused nausea and Vomiting. Perhaps their reaction to the drug was abnormal, even on the first exposure.
However this may be, with repeated use and development of tolerance to side effects, the euphoric action evolved, and the subjects became established addicts.
Drug-seeking behavior, like theft, is observed after addiction is established and the narcotic drug has become euphorigenic. The question as to whether this abnormality in reaction stems from the basic weakness of character, or is a consequence of drug usage, is best studied when drug hunger is relieved. Patients on the methadone maintenance program, blockaded against the euphorigenic action of heroin, turn their energies to school work and jobs. It would be easy for them to became passive, to live indefinitely on public support and claim that they had done enough in winning the fight against heroin. Why they do not yield to this temptation is unclear, but in general they do not.
Their struggles to become self-supporting members of the community should impress the critics who had considered them self-indulgent when drug-hungry addicts. When drug hunger is blocked without production of narcotic effects, the drug-seeking >behavior ends.
We are not aware of any comparable success in treatment of addicts by psychotherapy. This casts some doubt on the psychogenic theory of addiction but of course does not disprove it. Conceivably a basic character defect might lead to drug use and this in turn to an irreversible addiction in which the subsequent behavior of the subject is determined by conditioned reflexes or by metabolic changes in neurons following repeated exposure to narcotic drugs. This argument, however, represents a considerable departure from a purely psychological theory of addiction and relapse.
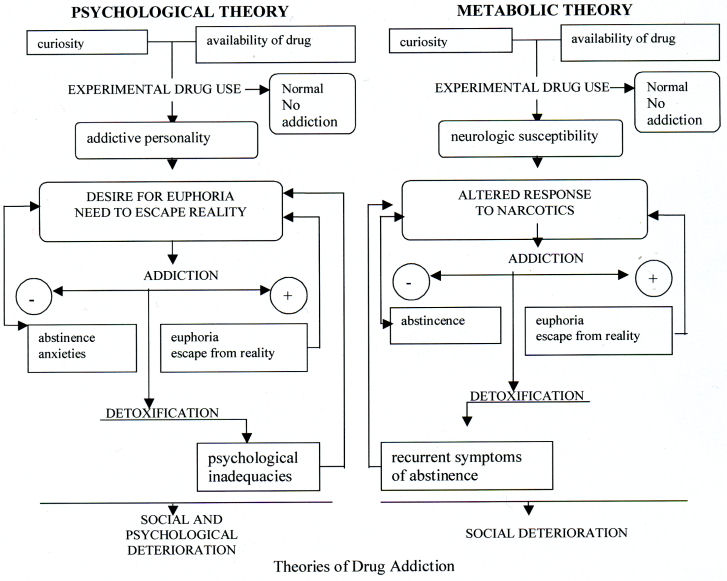
To make the contrast between psychologycal and metabolic (or "pharmacodynamic") theories more precise, let us represent these theories in diagrammatic form (Figure). The diagrams obviously do not exhaust the possibilities of conjecture - it would be easy to construct hybrid theories in which psychological and metabolic factors were combined in various ways, or to postulate that addicts are heterogeneous, some psychological and others metabolic - but this would merely complicate the discussion without going to the central point, which is the problem of how to use clinical data to discriminate between different theories of causation. The diagrams emphasize the fact that both theories, although widely divergent in describing preaddicts or ex-addicts, postulate essentially the same dynamics for perpetuation of an established state of addiction. This means that a choice between theories must be based on data defining the psychological and metabolic condition of the subjects before addiction or after a cure.
Knowledge of the preaddiction state is meager. So far as can be judged from retrospective data, narcotic drugs have been quite freely available in some areas of New York city, and experimentation by adolescents, common. The psychological and metabolic theories diverge somewhat in interpreting this fact; the first postulates preexisting emotional problems and a need to seek drugs for escape from reality, while the alternative is that trial of drugs, like smoking the first cigarette, may be a result of a normal adolescent curiosity and not a psychological pathology.As to the most important point - the reasons for continuation of drug use in some cases, and not in others - there is no definitive information, either psychological or metabolic. This is obvioussly a crucial gap in knowledge. Systematic study of young adolescents in areas with a high addiction rate is needed to define the process of becoming addicted and to open the way for prevention.
The other extreme, the cured addict, involves a controversy as to the goal of therapy. Those of us who are primarily concerned with the social productivity of our patients define success in terms of behavior - the ability of the patients to live as normal citizens in the community - whereas, other groups seek total abstinence even if it means confinement of the subjects to an institution. This confusion of goals has barred effective comparison of treatment results.
Actually the questions to be answered are straightforward and of great practical importance. Do the abstinent patients in the psychological programs have a residual metabolic defect that requires continued group pressure and institutionalization to enforce the abstinence? Conversely, do the patients who are blockaded with methadone exhibit any residual psychopathology?
No evidence is available to answer the first question. As to the latter point we can state that the evidence so far is negative. The attitudes, moods, intellectual and social performance of patients are under continuous observation by teams of psychiatrists, internists, nurses, counselors, social workers, and psychologists. No consistent psychopathology has been noted by these observations or by the social agencies to which we have referred patients for vocational placement. The good records of employment and school work further document the patients' capacity to win acceptance as normal citizens in the community.
Psychiatric evaluation of patients with individual problems show for the most part normal reactions to reality situations. It would appear, therefore, that if the addiction of our patients had originated in a need to escape reality, the psychopathology must have disappeared in the course of addiction. On the basis of psychogenic theory the converse would be expected; with years of avoiding reality by drug use, the patients should have become progressively less adequate emotionally. They would not be expected to respond in a normal way to an abrupt ending of heroin use, and confrontation with problems of school, vocational training, employment, and family responsibility.
The social deterioration of addicts may be profound - they may have lost family, property and social status - but it must not be too quickly assumed that these are weak individuals who would fail in society if relieved of the compulsion to obtain drugs.
The potential strengths of addicts, like their faults, cannot be judged while the addicts are trapped in the orbit of drug abuse.
Summary
The unexpectedly favorable response of addicts to the maintenance program has forced us to reexamine the psychogenic theory of addiction. Historically, this theory has been based upon study of established addicts, and not upon data obtained in the pre-or postaddicted state. The so-called addictive personality therefore could be interpreted either as a cause or a consequence of addiction.
The new evidence provided by the results of maintenance treatment strongly suggests that the "addict traits" are a consequence, not a cause, of addiction and demonstrates that a substantial number of addicts can be rehabilitated on a medical program. To explain these new findings, an alternative theory, emphasizing metabolic aspects of addiction is presented.
This study was supported in part by grants from the Health Research Council (City of New York Department of Health), Department of Hospitals, and the Community Mental Health Board of New York City </P
Generic and Trade Names of Drug
Methadone hydrochloride - Adanon Hydrochloride, Dolophine Hydrochloride, Althose Hydrochloride, Amidone Hydrochloride.
References
1. Dole, V.P., and Nyswander, M.E., A Medical Treatment for Diacetylmorphine (Heroin) Addiction, JAMA 193:646-650, 1965.
2. Dole, V.P.; Nyswander, M.E. and Kreek, M.J: >Narcotic Blockade, Arch Intern Med 118:304-309, 1966.
3. Dole, V.P., and Nyswander, M.E.: Rehabilitation of Heroin Addicts After Blockade with Methadone, NY State J Med 55:2011-2017, 1966
4. Dole, V.P.; Kim, W.K.; and Eglitis, I.: Detection of Narcotic Drugs, Tranquilizers, Amphetamines, and Barbiturates in Urine, JAMA 198:349-352, 1966.
>5. Terry, C.E. and Pellens, M: The Opium Problem, New York: Bureau of Social Hygiene, Inc., 1928.
6. Wikler, A,: "Conditioning Factors in Opiate Addiction and Relapse" In Wilner, D.M., and Kassebaum, G.G. (eds): Narcotics: New York: McGraw Hill, 1965, p. 85.
7. Wilker, A., and Rasor, R.W.: Psychiatric Aspects of Drug Addiction, Amer J Med 14:566-570, 1953.
Last Updated (Monday, 20 December 2010 20:05)












