Diversion of prescribed drugs by drug users in treatment: analysis of the UK market and new data from London
Drug Abuse
RESEARCH REPORT
Diversion of prescribed drugs by drug users in treatment: analysis of the UK market and new data from London
JANE FOUNTAIN, JOHN STRANG, MICHAEL GOSSOP, MICHAEL FARRELL & PAUL GRIFFITHS
National Addiction Centre, Maudsley Hospital/Institute of Psychiatry, London, UK
Abstract
Aims. To review the available knowledge about the diversion to the illicit market of drugs prescribed to drug users in treatment in the United Kingdom, and to identify aspects of the London market in more detail. Method. An analysis of the literature and new data in terms of the extent and nature of the market, the practicalities of trade, motives for selling, reasons for demand and the influence of variations in prescribing practice on diversion. Prices of diverted prescription drugs and details of their availability in London are presented. Findings. The size of the market is substantial and appears to involve a large number of individuals, each diverting small amounts of their own prescribed drugs. Major motives for selling prescribed drugs are to raise funds to buy other, preferred, drugs and/or to pay for a private prescription. Buyers in treatment appear to be motivated by a desire to supplement their own prescriptions because they are dissatisfied with the particular drug prescribed, dosage and formulation. Drug uses in treatment can exploit the variations in prescribing practice—such as how much 'take-home' medication they are allowed and whether tests are conducted to ascertain if they are using it themselves—and divert their prescribed drugs. Prices of prescription drugs on the illicit market can fluctuate on a daily basis according to supply and demand. Conclusions. The results suggest that, to be effective, diversion control must simultaneously involve deterrents from prescribers, drug treatment services, law enforcement agencies and dispensing pharmacists. Finally, some suggestions for further research on this under-studied issue are suggested.
Introduction
This paper examines the diversion to the illicit market in the United Kingdom of drugs prescribed to drug users to treat their drug dependence and misuse. These drugs are methadone, benzodiazepines and, less commonly, stimulants such as dexamphetamine sulphate (Dexedrine) and opioids other than methadone, such as dihydrocodeine tartrate (for example, DF118), buprenorphine (Temgesic) and diamorphine
(heroin). Such an analysis is timely for several reasons. First, there has been recent attention to the increased incidence of drug overdoses in which methadone is involved (Ward, Mattick & Hall, 1992; Marks, 1994; Cairns, Roberts & Benbow, 1996; Newcombe, 1996a; McCarthy, 1997; Strang et al., 1999). Secondly, there is an increase in the number of notifications of addiction to pharmaceutical drugs (Home Office, 1997). Thirdly, the Task Force Report to Review Services for Drug Misusers (Department of Health, 1996) identified diversion as a problematic aspect of substitute prescribing, as did the later Department of Health Drug Misuse and Dependence: Guidelines on clinical management (1999). Fourthly, there have been anecdotal reports of non-dependent drug users using methadone or benzodiazepines to relieve the after-effects of so-called 'recreational' use of drugs such as ecstasy and stimulants. Fifthly, the health risk behaviour of those who misuse prescription drugs—especially benzodiazepines—is a particular cause for concern (Klee et al., 1990; Ruben & Morrison, 1992; Strang, Seivewright & Farrell, 1993; Ghodse, 1995). Finally, implicit in the new UK Guidelines on Clinical Management (Department of Health, 1999) is that good prescribing practice minimizes diversion.
It is generally accepted that some diversion is unavoidable (Department of Health, 1996), and the literature on diversion control argues that the energy and ingenuity which some drug users devote to obtaining drugs to divert can thwart control attempts unless all avenues are closed simultaneously. When restrictions are placed on only one substance or source of supply, buyers may find a substitute or experiment with new combinations of drugs or routes of administration to achieve the desired effect (Gossop, Strang & Connell, 1982; Klee et aL, 1990; Strang, Seivewright & Farrell, 1992, 1993; Fountain et al., 1999). The process is greatly assisted by drug users' efficient grapevines (Dupont, 1988; Fountain et al., 1996).
Method
Most of this paper derives from an analysis of the published and unpublished literature on the topic. However, it also includes previously unpublished results from a study on the use of diverted prescription drugs by chronic drug users and the operation of drugs market-places in London where these substances are traded (Fountain et aL, 1996, 1998, 1999). Literature searches revealed few studies dealing with the phenomenon in readily accessible publications such as journals dealing with drug-related issues. Unfortunately, major UK studies have hitherto appeared only in reports to organizations who commissioned the research (for example, Dale & Jones, 1992; Haw, 1993).
The London data comprise price information
and observations on availability. They come from a study conducted in 1995-96 (Fountain et al., 1996, 1998, 1999) which used qualitative methods with a small number of networks of chronic polydrug users from several drugs market-places. In total, approximately 100 drug users were involved in the study, with access to the market-places facilitated by drug users known previously to the research team. The • sample were chosen specifically because they bought and/or sold drugs prescribed to drug users in treatment. A third of the sample were interviewed on several occasions over the study period, and these interviews were tape-recorded and transcribed. Staff from treatment services were also informally interviewed. However, casual conversations with, and observation of, those trading in prescription drugs played an equally important role in the data collection process. For the purposes of this paper, three key informants were asked to update the data on prices and availability. This indicated no significant change over the 3-year period.
Results
The extent and nature of the market
Reports of the proportion of drug users in treatment who sell their prescribed drugs range from 5% to 34% (Whynes et al., 1989; Haw, 1993; Parker & Kirby, 1996) and studies that ask for the sources of drugs used by misusers support the view that there is a substantial market in diverted prescription drugs (Dale & Jones, 1992; Haw, 1993; McDermott & McBride, 1993).
There appears to be geographical variation in the type and amount of diverted substances. Major reasons for this are local prescribing policies, the availability of illicit drugs and the patterns of drug use of buyers and sellers (Whynes et aL, 1989; Haw, 1993). Over- and undersupply can occur in the same market-place on • the same day since trade seems to rely heavily upon the surplus supplies of many individual sellers; several individuals collecting 2 weeks' • supply of drugs from a pharmacy on the same day can create a glut, but a shortage can quickly follow when they are sold (Burr, 1983; Fountain et al., 1996).
Research on the distribution of diverted prescription drugs shows that sellers operate only at the lowest level of distribution. Sales are conducted by a large number of individuals, each diverting some of their own prescribed drugs (Edmunds, Hough & Urquia, 1996; Fountain et al., 1996; Parker & Kirby, 1996). There are no reports that smuggling, illicit manufacture and organized crime feature in the distribution of prescription drugs in the United Kingdom.
`Market-places' are central to the distribution of prescription drugs and typically evolve near drug treatment agencies, needle exchanges and those pharmacies which dispense prescriptions to drug users in treatment. Drug trading hours often reflect those of these agencies (Burr, 1983;
Jones & Power, 1990; Fountain et al., 1996). In some areas, prescription drugs and illicit drugs are bought and sold in the same market-place, while in others they are traded in separate locations (Edmunds et al., 1996, Fountain et al., 1996). The legality of ownership of prescription drugs facilitates the operation of market-places where they are traded. Potential buyers and sellers can linger with impunity until the point of sale. It has been reported that the police rarely discover diverted prescription drugs because distribution is contained within networks of drug users trading in personal prescriptions (Parker & Kirby, 1996). However, the police may be attracted to drugs market-places because of the behaviour of those who frequent them, the presence of known drug users (some of whom have criminal records), and complaints from the general public (Jones & Power, 1990; Pharmaceutical Journal, 1996a, 1997b). Market-places have shown themselves to be remarkably resilient, and their reaction to disruption has often been to relocate nearby (Burr, 1983; Dale & Jones, 1992; Edmunds et al., 1996; Fountain et al., 1996).
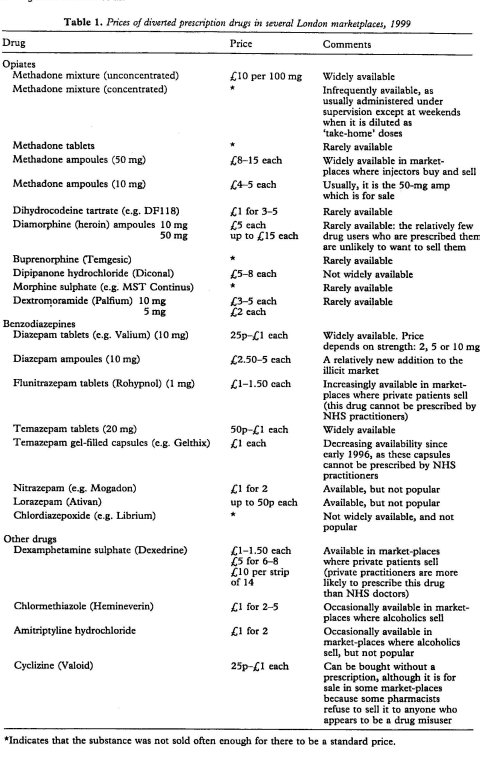
There are few data on the prices of diverted prescription drugs on the illicit market, particularly those other than methadone, and prices can fluctuate according to supply and demand. As a guide only, prices of prescription drugs sold on the market-places in London studied by Foun- tain et al. (1996; data updated 1999) are shown in Table 1. From this, some general principles about the determinants of price on the illicit market can be postulated:
• Overall, prescription drugs seem to be cheaper than their equivalent in illicitly manufactured drugs.
• Drugs that are dispensed in an injectable formulation—methadone and diazepam am-
poules—are more expensive than the oral formulations. The scarcity of injectables on the illicit market may further add to their cost. (In the United Kingdom, for example, 10 times more prescriptions are written for oral methadone mixture than for injectable methadone ampoules (Strang, Sheridan & Barber, 1996; Strang & Sheridan, 1998).)
• High-dose units are cheaper per mg than low-dose units: thus, a 10-mg methadone ampoule costs £2.50-3.50 in London, while a 50-mg ampoule can cost as little as £8 in times of plentiful supply.
• The quality of the 'hit' of a substance may affect its price. This is reflected, for instance, in the relatively high prices of temazepam and diazepam in relation to lorazepam (Ativan) and chlordiazepoxide (for example, Librium).
• Benzodiazepines are relatively cheap on the illicit market.
Trading in prescription drugs: the practicalities
The diversion of prescription drugs may occur in principle at any point in their manufacture, transportation, delivery, storage and dispensation. However, studies reveal that drug users in treatment are the primary diverters (VHPF, 1974; Burr, 1983; Spunt et al., 1986; Fountain et aL, 1996). The theft of prescription drugs from UK manufacturers, pharmacies, surgeries and drug treatment clinics is rare (Ruben & Morrison, 1992; Parker & Kirby, 1996). There have been only rare reports from UK studies that prescription drugs have been diverted to the illicit market by manufacturers and wholesalers, and reports of doctors and other health workers being involved in illegal diversion are also rare. There is some diversion from individuals who are not drug users in treatment but who have been prescribed opioids for pain, and benzodiazepines for stress or depression (Jones & Power, 1990) but, again, this practice does not appear to be widespread.
Some pharmacists who dispense prescriptions to drug users in treatment have been found to disregard the instructions regarding the frequency with which the drugs are to be dispensed (`pick-up' intervals), allowing patients to collect up to 2 weeks' supply at a time (Edmunds a al., 1996; Fountain et al., 1996). It has been reported occasionally that some pharmacists also give credit to private patients, allowing them to take away more drugs than they have paid for, some of which are then sold in order to raise the money to pay the pharmacist for the next instalment (Pharmaceutical Journal, 1997b). It has also been reported that pharmacists have sold large quantities of prescription-only drugs to dealers (Pharmaceutical Journal, 1993), or smaller amounts to drug users (Pharmaceutical Journal, 1996b, 1997a).
The majority of drug users in treatment who acquire prescription drugs surplus to their own requirements use either or both of two methods (Dale & Jones, 1992; Fountain et al., 1998): they obtain prescriptions from more than one drug treatment service (`multiple-scripting', often inaccurately known as 'double-scripting') and/or they obtain a larger dosage and/or a wider variety of drugs than they use (`over-scripting'). Thus they may exaggerate the amount of drugs used in order to obtain a larger prescription for substitutes than needed, they may claim addiction to alcohol in order to obtain benzodiazepines, use false identities in order to obtain more than one prescription, claim to be a temporary resident to acquire a `one-off prescription, or exploit prescribers judged to be sympathetic (Burroughs, 1953; McKeganey, 1988; Jones & Power, 1990; Wheeldon, 1992; Seivewright, Donmall & Daly, 1993; Fountain et al., 1998).
Motives for selling
Individuals are likely to change their motives according to their current drug-using pattern, treatment status and financial situation. We believe that a crude form of classification can be made:
• drug users in treatment who are dissatisfied with the drugs they are prescribed;
• drug users receiving private treatment who are raising funds to pay prescription and dispensing fees; and
• alcoholics selling benzodiazepines to buy alcohol.
The first two of these classifications seem to be most common (Fountain et al., 1996). A prescription from a National Health Service (NHS) practitioner currently has a standard fee of £5.90 per item (or is free to those on a low income) but the cost of private treatment varies. In London, where the majority of private treatment is located, the initial consultation and assessment from a private practitioner is around £50, plus £25 per week for the prescription/consultation. The total cost, depending on the drug, dosage, formulation and the pharmacy's prices, can reach £125 a week.
Benzodiazepines not only reach the illicit market via drug users in treatment. It has been reported that alcoholics who are receiving benzodiazepines as part of their treatment programme sell them to drug users in order to raise the funds to buy alcohol (Jones & Power, 1990; Fountain et al., 1996).
Some sellers can best be described as 'reluctant' or 'retired' criminals. Drug users with no prescription to use as currency to buy their preferred drugs must fund their use by other methods. It has been reported that if a drug user in treatment is obtaining surplus drugs and selling them, they are less likely to commit other acquisitive crimes (Burr, 1983; Dale & Jones, 1992; Edmunds et al., 1996; Fountain et al., 1996). This is a pivotal rationale some private practitioners use for prescribing the drugs, the dosage and the formulation wanted (Brahams, 1987; Garfoot, 1996). However, it should be noted that although private patients have been reported to commit fewer crimes (other than selling drugs) than patients of other prescribers (Burr, 1983), it has also been shown that, typically, drug users with a prescription commit fewer crimes than those not in treatment (Dale & Jones, 1992; Haw, 1993; Farrell et al., 1994; Gossop et al., 1999). Fountain et al. (1996) detail how their sample of ageing drug users in treatment sold their prescribed drugs rather than commit other crimes to fund their heroin use: their appearance, physical capabilities and reputations in local shops meant that burglary, mugging and shoplifting were not viable income sources.
Reasons for demand
In the United Kingdom, the most economical method for a drug user to obtain prescription drugs is to acquire an NHS prescription. If the prescribed dosage and variety of drugs are less than they are trying to obtain, then over- or multiple-scripting is another cost-free option (Fountain et al., 1998). If yet more prescription drugs are sought, two options exist: to buy them on the illicit market or to obtain a private prescription which, as discussed shortly, is more likely to be for the preferred variety, dosage and formulation. The latter is the cheaper option if an individual can raise and maintain the necessary fees: for example, in London, the cost of a private prescription for four 50-mg methadone ampoules per day (a frequently prescribed amount) is around £100 per week. On the illicit market, these would cost £224-L420 (see Table 1). However, some drug misusers could not accumulate £100 as a single sum every week. An alternative is to buy from the illicit market several times a week, according to the cash available, where they can obtain single ampoules at £8-15 each.
This section deals mainly with the reasons why diverted prescription drugs arc bought by those drug misusers with whom most research on diversion is concerned: polydrug-using opiate addicts. The major reasons for the demand are that the potential purchaser does not have a prescription for the drugs they want, or that they have a prescription but use a higher dosage than has been prescribed, and/or prefers other formulations (such as injectable rather than oral methadone).
As the supply of diverted prescription drugs differs between markets, so does demand. In some markets, diverted prescription drugs are not a marketable commodity (Whynes et al., 1989), while others trade primarily in these substances (Edmunds et al., 1996; Fountain et a/., 1996). Contradictory reasons for demand have been reported, and there have been calls for further research into this issue (Ruben & Morrison, 1992; Strang et al., 1993; Darke, 1994).
Patterns of use of diverted prescription drugs range from regular and heavy use by polydrugusing opiate addicts to occasional use by so-called 'recreational' drug users. Purchases of diverted drugs are not necessarily made on a regular basis. The diverted drug can be a 'treat', for use as an experiment, or in an emergency such as buying oral methadone to avoid withdrawal symptoms when no heroin is available (Dale & Jones, 1992; Fountain et al., 1996). Thus the amounts of substances purchased from the illicit market vary from, for example, a single dose of methadone occasionally to 2 weeks' supply regularly, or from a couple of benzodiazepine tablets as a 'one-off experiment to 20 tablets every day. Some buyers are discerning about the drugs they buy, others are less particular. In addition, an individual is likely to change his or her reasons for purchasing prescription drugs according to his or her current drug-using pattern, treatment status and financial situation. Bearing these differences firmly in mind, purchasers can be classified into drug users who:
• are supplementing a prescription;
• have no prescription;
• have a prescription, but not for the drugs and/or the formulation they prefer, and have raised the funds to buy their preferences by selling their own prescribed drugs;
• are polydrug users; or
• prefer pharmaceutical to illicit drugs.
Each of these types of purchaser will now be considered in turn.
Supplementing a prescription. An insufficient dose (real or perceived) of prescribed drugs can occur at the start of treatment, particularly if the addict has high expectations that it will address all of his or her drug needs and will stop cravings for other drugs (Dole, Nyswander & Kreek, 1966; Preston, 1996). It can also occur during treatment, if the dosage is reduced too quickly and if tolerance to the drugs prescribed—and/or those used in addition—increases (Fountain et al., 1996). The demand for diverted prescribed drugs should not be attributed solely to too low a dosage, however. It may also reflect a preference for an effect which cannot be obtained from the prescribed drugs alone (Bell et al., 1990; Newcombe, 1996b).
No prescription. There are several reasons why those who are drug-dependent and buy diverted prescription drugs do not arrange their own prescriptions, including an unwillingness—especially of women with children—to submit to official attention, and that previous treatment episodes have left them disillusioned with services (McKeganey, 1988; Sheehan, Oppenheimer & Taylor, 1988; Stimson et al., 1995; • Department of Health, 1996; Powis et al., 1996). Some buyers may not be dependent drug users, and thus have no condition requiring treatment and a prescription. Such a group might include, according to recent anecdotal reports, young ecstasy and stimulant users, who use methadone
or benzodiazepines to relieve after-effects of their 'recreational' drug use.
Prescription not for the drugs and/or formulation preferred. NHS drug treatment services are reluctant to prescribe injectable formulations to drug misusers and successive government documents have emphasized the caution with which such injectable drugs should be prescribed (ACMD, 1993; Department of Health, 1991, 1999). However, this reluctance to prescribe injectable drugs stimulates demand from the illicit market by injectors for pharmaceutical drugs which are—or can be rendered—injectable, even though these same individuals may already be receiving a prescribed supply of the same drug in oral form (Dale & Jones, 1992; Fountain et aL, 1996).
Polydrug users. Opiate addicts do not generally use diverted methadone (particularly the oral formulation) for its pleasurable effects. Rather, its main roles in polydrug-using repertoires are as a cheap and safe medication to reduce withdrawal symptoms and as a base for drug cocktails (Dale & Jones, 1992; Haw, 1993; Lauzon et al., 1994; Chatham et al., 1995; Rettig & Yarmolinsky, 1995). Combinations, about which the user may be discerning or not, can include illegally manufactured drugs (such as heroin and cocaine), methadone and other prescribed opioids, alcohol, benzodiazepines and stimulants (cocaine, amphetamine sulphate and dexamphetamine sulphate). Benzodiazepincs are also used to 'come down' from stimulant use, and to counteract the insomnia caused by stimulants or opiate withdrawal. These drugs are also taken by some users to give them the confidence to commit crimes (Klee et al., 1990; Ruben & Morrison, 1992; Fountain et aL, 1996).
Prefer pharmaceutical drugs. Polydrug-using opiate addicts who include prescription drugs (licitly and illicitly obtained) in their drug-using repertoires use combinations of substances to achieve one or more of three effects: a 'rush' or 'hit' (a sudden onset feeling of excitement as the drugs take effect), a touch' (a trance-like, intoxicated state), and/or to 'hold' them (stop withdrawal symptoms). The impurity and cost of illicit drugs means that some prefer prescription drugs to obtain these effects (Fountain et al., 1996). It has been suggested that benzodiazepines and buprenorphine (Temgesic) are consequently taking the place of heroin as the preferred drug (Sakol, Stark & Sykes, 1989; Hammersley, Lavelle & Forsyth, 1990; Klee et al., 1990). An additional significant attraction of
prescription drugs to the purchaser is that they are manufactured in standard doses and are recognizable.
Self-treatment. It has been suggested that some of those buying diverted prescription drugs—particularly methadone—are engaged in self-treatment (Langrod, Galanter & Lowinson, 1974; Spunt et al., 1986; Gossop, Battersby & Strang, 1991; Dale & Jones, 1992), and that the benefits of prescription drugs are therefore reaching an out-of-treatment population. However, `self-treatment' suggests that users arc mimicking the therapeutically based decisions of treatment agencies. The combinations and suprathcrapcutic amounts of drugs used by some who buy prescription drugs on the illicit market are not generally purchased with such therapeutic objectives, and would not be available to them in these forms and doses via legitimate treatment sources (Ruben & Morrison, 1992; Scivcwright & Dougal, 1993; Strang et al., 1993). Nevertheless, some users of diverted prescription drugs have assimilated the harm reduction advice emanating from drug treatment services and disseminated by the drug users' grapevine. Ironically, the knowledge that illicit drugs and injecting are dangerous probably increases the demand for the 'safer' prescription drugs for injection (Edmunds et al., 1996; Fountain et al., 1996), even though there may be additional dangers from the crushing and injecting of tablets meant only for oral use (Strang et a/., 1998; Department of Health, 1999).
Variations in prescribing practice and their influence on prescription drug diversion
There is no central policy in the so-called 'British system' which defines who can prescribe substitute drugs to drug users. Any qualified doctor, whether drug specialist or general practitioner, whether NHS or private practitioner, has the authority to prescribe any drug in the treatment of addiction, apart from heroin and cocaine and, since 1984, dipipanone (Diconal), for which a special licence is required and is issued in practice only to NHS drug specialists. A consequence of this is that the opportunity exists for drug users in treatment to exploit the looseness of the system to divert some or all of their prescribed drugs (Battcrsby et al., 1992; Strang & Gossop, 1994; Brewer, 1995; Farrell et al., 1995; Preston 1996; Strang et al., 1996; Fountain et al., 1998). The type, dosage and formulation of the drugs prescribed varies widely not only between the three types of prescriber, but also among practitioners from each group. The prescribing and dispensing of benzodiazepines are less tightly controlled than for methadone (Department of Health, 1996), making them easier to divert.
Some of the private practitioners who treat drug users prescribe a wider variety of drugs, and most prescribe larger dosage of drugs than NHS sources, specify longer dispensing intervals and are more likely to prescribe injectable drugs (Strang et al., 1996; Pharmaceutical Journal, 1997b). In some market-places, drugs diverted from private prescriptions represent the major source of supply, and the establishment or removal of just one private practice can result in a change in the drug-using patterns of those who buy there (Burr, 1983; Spear, 1994).
Whether their motives are pecuniary (Edmunds et al., 1996) or involve genuine treatment strategies (Garfoot, 1996), the liberal prescribing practices of some private practitioners has long been a cause for concern (for example, Strang, 1982; Bewley & Ghodsc, 1983; Spear, 1994; Parameshwar, 1995; Department of Health, 1996; Strang et al., 1996; Preston, 1996; Department of Health, 1999). For some drug users, however, such liberal prescribing represents an attractive treatment option, but if they have inadequate other income, they may pay for prescribing and dispensing fees by over-scripting and selling the surplus.
The majority of GPs refuse to treat drug users, despite endeavours to persuade them otherwise (for example, Glanz & Taylor, 1986; McKeganey, 1988; Bell, Cohen & Cremona, 1990; Groves et al., 1996; Ford & Ryrie, 1999) and, of those who do, there are wide variations in their prescribing practices (Gerada & Tighe, 1999).
NHS specialist drug treatment clinics generally adhere to agreed procedures and practices (Connell & Mitcheson, 1984) and to recommended practice and the incorporation of monitoring and safeguards against diversion. Specialist clinics are also less likely than general practitioners to prescribe methadone tablets (which may be crushed and injected), more frequently stipulate daily dispensing of each day's supply of drugs and arrange supervision of consumption (Gossop et al., 1999). Clients of a specialist clinic are therefore able to divert fewer drugs, and only a small amount at a time.
As discussed below, other differences in policies which facilitate or hinder diversion are whether or not the service allows clients to take home their medication, checks patients' identities, conducts tests or operates a used ampoule return system.
Take-home' medication. It is well established that take-home medication is the facet of prescribing policy which most facilitates diversion (Inciardi, 1977; Burr, 1983; Spunt et al., 1986; Lauzon et al., 1994; Rettig & Yarmolinsky, 1995). Daily dispensing and supervised consumption are the norm internationally, but British guidelines recommending this practice (Department of Health, 1991, 1999) are widely disregarded, with a third of all methadone prescriptions in England and Wales being given out in quantities of at least a week's supply in a single dispensing (Strang et al., 1996). Obviously, if all prescribed drugs were consumed under strict supervision then diversion should be minimal, although there is continued professional dispute about the feasibility of this approach and how it would be conducted in practice (Scott, Burnett & McNulty, 1994; Thomas, 1994; Brewer, 1995; McLeod, 1995). Even where consumption is supervised, the sale of `spitbacks' (where clients hold a drug in their mouths and spit it out) may occur, as has been reported in the United States and Canada (Spunt et al., 1986; Lauzon et al., 1994). This has rarely been reported in the United Kingdom, however, even in parts of the country such as Glasgow, where supervised consumption of oral methadone has recently been extensively introduced (Gruer et a/., 1998). The possible supervision of consumption of injectable drugs—which comprise about 10% of prescribing to drug misusers (Strang et al., 1996)—has recently been introduced in Switzerland as part of the treatment of entrenched opiate addicts (Perneger, del Rio & Mino, 1998; Bammer et al., 1999). However, in the United Kingdom, there has so far been virtually no supervision of the administration of injectable drugs, which is generally considered impractical in the case of those who inject them several times a day (Brewer, 1995; Metrebian, Shanahan & Stimson, 1996).
Identity checks. Until it was discontinued in April 1997, it was possible for prescribers to verify the identity of an opiate addict patient with the Home Office Addicts Index. This procedure could expose those who had obtained more than one prescription. Unfortunately, failure of practitioners to register patients diligently and exclusion of benzodiazepine and stimulant dependence meant that the Index had limited efficiency (Mott, 1994). Nowadays, identity checks are conducted in some localities or by some practitioners (Brewer, 1995). This approach offers a mechanism for reducing substantially the scope for diversion although, without an identity card system in operation in the United Kingdom, it may be difficult for the practice to become widespread outside specialist centres (that is, it might be particularly difficult to be implemented by GPs). In these circumstances, if implemented only patchily, it would be unlikely to be effective and might merely promote movement of patients seeking to exploit the weaknesses of the system towards services without this identity check.
Drug testing. Testing—at the start of treatment and at regular intervals during its course—is frequently advocated as vital for the management of drug users in treatment and an essential diversion control strategy (Preston, 1996). This is usually undertaken with urine samples. There are tests to determine whether a claim of addiction is correct, which substances are being used, substitution dosages and changes in consumption levels. However, there is a wide variation in the use of such tests between prescribers. Further, whether testing takes the form of breathalysing, urinalysis, hair analysis or serum level testing (for example, plasma methadone monitoring), each has its limitations (Brewer, 1995; Raistrick et al., 1995; Metrebian, Shanahan & Stimson, 1996; Wolff et al., 2000).
Ampoule return. There have been attempts to prevent the diversion of injectable methadone and heroin by marking the ampoules with an identifier. Patients must return their used ampoules before receiving more (Metrebian et al., 1998). This does not appear to be common practice, however. While such an approach would not ensure absolutely that the take-home supply of injectable drugs had been used by the
patient themselves, it would nevertheless stand as a practical obstacle to the sale of ampoules on the illicit market. This strategy might effectively deter the patient with an occasional or uncommitted involvement with this market.
Discussion: options for control of the diversion of prescription drugs
The literature which explores possible diversion control strategies was comprehensively reviewed by NIDA, 1993. The main themes can be summed up as follows:
To be effective, an integrated prescription drug control system is necessary. This involves co-operation between prescribers, drug treatment services, law enforcement agencies and dispensing pharmacists. Control measures by any one of these agencies are unlikely to be effective if not supported by changes in practice of the others. One example is that tightening the controls on prescribing by specialist drug treatment clinics would have little effect on diversion if private practitioners who over-prescribe continued. Another illustration is that, although lowering the doses of drugs prescribed to addicts would make fewer substances available for diversion, too low a dosage might be a major reason for demand for more from the illicit market.
• A balance needs to be struck between measures to control abuse of the system, while at the same time supporting ease of access to treatment for the patient and encouragement of the involvement of a larger number of medical practitioners. The positive outcomes of effective control systems are a reduction in diversion and a more appropriate use of drugs. The negative outcomes are the financial cost of control measures and that prescribers and patients will come under increased scrutiny, which may discourage both from participation in treatment.
• More research is needed to determine the prevalence of diversion, identify the mechanisms by which it occurs, and establish the effect of changes in prescribing practices on drug-using patterns and treatment outcomes. We explore possible ways of undertaking such research later in this discussion.
Private prescribing to addicts is uncommon but, when it occurs, is often distinctive (Strang et al., 1996). Greater scrutiny and tighter controls on private prescribing have consequently been suggested as a way of dealing with unacceptably lax practice and the substantial risk of diversion of prescribed drugs to the illicit market (Department of Health, 1996). However, a possible effect of this strategy has been identified by Edmunds et al. (1996) in London, who argue that a reduction in private prescriptions could lead former private patients (who had previously used and also sold some of their drugs) to increase their fund-raising activities in order to pay for more. Edmunds and colleagues posit that the result could be an increase in acquisitive crime.
In the United Kingdom, the willingness of general practitioners to be involved in the management of the drug misuser is substantially dependent on prior education and the perceived level of work (Deehan, Taylor & Strang, 1997), in much the same way as has been found to be the case with GPs and their management of the problem drinker (Deehan et al., 1998a, 1998b). However, it remains unclear whether the provision of support necessarily results in increased GP involvement or merely provides a new avenue of referral (Tantam et al., 1993). Despite general guidance, arrangements for joint working between specialists and GPs remain extremely variable and idiosyncratic (Gerada & Tighe, 1999).
How might our qualitative study, or similar, be conducted in other countries or regions and in other times? Methods of monitoring and reporting on the extent of prescription drug diversion are currently poorly developed even though, as recognized by the UK government's Tackling Drugs to Build a Better Britain (Stationery Office, 1998), diverted prescription drugs comprise `significant quantities' of the drugs trade. More sophisticated methods of monitoring are necessary in order to provide a sound knowledge base with which to inform policy. The first stage of this process is to clarify objectives. The study conducted by Fountain et al. (1996) set out to obtain a better understanding of the illicit market in diverted prescription drugs in London, but other objectives could easily be identified and could be applied elsewhere. These might include the following: identification of which prescribed drugs are being diverted and their relative prices on the illicit market; the proportion of substances prescribed to drug misusers in treatment which are diverted; the size of the market compared to that of illicitly manufactured heroin; prescribing practices or legislation which facilitate and hinder diversion; the effect of changes in legislation or treatment provision on the prescription drugs available on the illicit market; market-place operations; the place of diverted prescription drugs in drug-using repertoires; sources of supply; and reasons for demand.
These data should be regularly collected and reported. Certainly they would then be more meaningful and might better inform the much-needed science-policy dialogue (Edwards, Strang & Jaffe, 1993). Changes could provide an early indication of changes in the drug-using patterns of a population due to modifications of prescribing practices (Fountain at al., 1999), or identify a new source of supply. For example, to what extent does decrease in supply of one drug put up its price on the illicit market and increase the demand for alternatives? To what extent does this, in turn, put up the prices of other drugs? If levels of consumption remain the same, to what extent do price rises lead the consumer to increase their fund-raising activities, including diversion and other crimes (Bean & Wilkinson, 1988; Fountain et al., 1998)? The extent to which diversion control and consequent price rises lead to increased fund-raising activities or to decreased levels of use will be determined partly by the price-elastic nature of demand for such illicit or diverted drugs, but this is an area which has only rarely been seriously explored (but cf. Wagstaff & Maynard, 1988). Even when these issues have been explored more fully, additional careful consideration will still need to be given to the possible different or more unpredictable effect of diversion control, particularly if it is implemented in a piecemeal fashion.
There are also likely to be regional and international differences in the results, and these geographical differences may provide opportunities for valuable comparisons and tracking, depending on which drugs are prescribed to drug users in treatment, prescribing practices which dictate the ease with which they can be diverted, and which are preferred by drug users who buy prescription drugs on the illicit market. For example, it seems only in the United Kingdom that temazcpam gel-filled capsules have been popular with injectors (Strang et al., 1992) and while Fountain et al. (1996) report that methadone was the staple of the London drug markets they studied, Haw (1993) found the prescription-only drug dihydrocodeine tartrate (for example, DF118) was the most commonly used `street drug' among her sample in Edinburgh, Scotland.
When substitute prescribing is included as an option for treating drug users, the level of concern and decisions made about the potential for diversion depend on whether the policy-making community is more concerned with treating addicts than preventing them selling drugs. We conclude that, however difficult, the objective should be the identification of the most health-conferring balance between caution against over-prescribing (and perhaps allowing the patient to sell the surplus on the illicit market) and caution against under-prescribing (and perhaps contributing to the patient 'topping up' from the illicit market).
Acknowledgement
The study and literature review from which much of the data for this paper were taken were funded by the Department of Health, England. The views expressed however, are those of the authors.
References
ADVISORY COUNCIL ON THE MISUSE OP DRUGS (ACMD) (1993) AIDS and Drug Misuse Report: update (London, HMSO).
BAMMER, G., DOBLER-MIKOLA, A., FLEMING, P., STRANG, J. & UCHTENHAGEN, A. (1999) The heroin prescribing debate: integrating science and politics, Science, 284, 1277-1278.
BATFERSBY, M., FARRELL, M., Gossor, M., ROBSON, P. & STRANG, J. (1992) 'Horse trading': prescribing injectable opiates to opiate addicts—a descriptive study, Drug and Alcohol Review, 11, 35-42.
BEAN, P. T. & WILKINSON, C. K. (1988) Drug taking, crime and the illicit supply system, British Journal of Addiction, 83, 533-539.
BELL, G., COHEN, J. & CREMONA, A. (1990) How willing are general practitioners to manage narcotic misuse? Health Trends, 2, 56-57.
BELL, J., BOWRON, P., LEWIS, J. & BATEY, R. (1990) Serum levels of methadone in maintenance clients who persist in illicit drug use, British Journal of Addiction, 85, 1599-1602.
BEWLEY, T. & GHODSE, A. H. (1983) Unacceptable face of private practice: prescription of controlled drugs to addicts, British Medical Journal, 286, 18761877.
BRAHAMS, D. (1987) 'Serious professional misconduct' in relation to private treatment of drug dependence, Lancet, 8528, 340-341.
BREWER, C. (1995) Recent developments in maintenance prescribing and monitoring in the United Kingdom, Bulletin of the New York Academy of Medicine, 72, 358-370.
BURR, A. (1983) Increased sale of opiates on the black-market in the Piccadilly area, British Medical Journal, 287, 883-885.
BURROUGHS, W. S. (1953) Junky (London, Penguin). CAIRNS, A., ROBERTS, I. & BENBOW, E. (1996) Characteristics of fatal methadone overdoses in Manchester, 1985-1994, British Medical Journal, 313, 264-265.
CHATHAM, L. R., ROWAN-SZAL, G. A., JOE, G. W., BROWN, B. S. & SIMPSON, D. D. (1995) Heavy drinking in a population of methadone-maintained clients, Journal of Studies on Alcohol, 56, 417-422.
CONNELL, P H & MITCHESON, M. (1984) Necessary safeguards when prescribing opioid drugs to addicts: experience of drug dependence clinics in London, British Medical Journal, 288, 767-769.
DALE, A. & JONES, S. S. (1992) The Methadone Experience (London, The Centre for Research on Drugs and Health Behaviour).
DARIO:, S. (1994) The use of benzodiazepines among injecting drug users, Drug and Alcohol Review, 13, 53-69.
DEEHAN, A., TAYLOR, C. & STRANG, J. (1997) The general practitioner the drug misuser, and the alcohol misuser: major differences in general practitioner activity, therapeutic commitment, and 'shared care' proposals, British Journal of General Practice, 47, 705-709.
DEEHAN, A., TEMPLETON, L., TAYLOR, C., DRUMMOND, C. & STRANG, J. (1998a) Are practice nurses an unexplored resource in the identification and management of alcohol misuse? Results from a study of practice nurses in England and Wales in 1995, Journal of Advanced Nursing, 28, 592-597.
DEEHAN, A., TEMPLETON, L., TAYLOR, C., DRUMMOND, C. & STRANG, J. (1998b) Low detection rates, negative attitudes, and the failure to meet the 'Health of the Nation' alcohol targets: findings from a national survey of GPs in England and Wales, Drug and Alcohol Review, 17, 49-258.
DEPARTMENT OF HEALTH (1991) Drug Misuse and Dependence. Guidelines on clinical management (London, HMSO).
DEPARTMENT OF HEALTH (1996) The Task Force to Review Services for Drug Misusers: report of an independent review of drug treatment services in England (London, Department of Health).
DEPARTMENT OF HEALTH (1999) Drug Misuse and Dependence: guidelines on clinical management (London, The Stationery Office).
DOLE, V. P., NYSWANDER, M. E. & KREEK, M. J. (1966) Narcotic blockade, Archives of Internal Medicine, 118, 304-309.
DUPONT, R. L. (Ed.) (1988) Abuse of benzodiazepines: the problems and the solutions. A report of a committee of the Institute for Behavior and Health, American Journal of Drug Abuse, 14 (suppl. 1), 1-69.
EDMUNDS, M., HOUGH, M. & URQUIA, N. (1996) Tackling Local Drug Markets. Crime detection and prevention series paper 80 (London, Home Office Police Research Group).
EDWARDS, G., STRANG, J. & JAFFE, J. H. (Eds) (1993) Drugs, Alcohol and Tobacco: making the science and policy connections (Oxford, Oxford University Press).
FARRELL, M., WARD, J., MATTICK, R., HALL, W., STIMSON, G. V., DES JARLAIS, D., GOSSOP, M. & STRANG, J. (1994) Methadone maintenance treatment in opiate dependence: a review, British Medical Journal, 309, 997-1001.
FARRELL, M., NEELEMAN, J., Gossor, M., GRIFFITHS, P., BUNING, E., FINCH, E.& STRANG, J. (1995) Methadone Provision in the European Union, International Journal of Drug Policy, 6, 168-172.
FORD, C. & RYRIE, I. (1999) Prescribing injectable methadone in general practice, International Journal of Drug Policy, 10, 39-45.
FOUNTAIN, j., GRIFFITHS, P., FARRELL, M., GOSSOP, M. & STRANG, J. (1996) A Qualitative Study of Patterns of Prescription Drug Use Amongst Chronic Drug Users, report prepared for the Department of Health (London, National Addiction Centre).
FOUNTAIN, J., GRIFFITHS, P., FARRELL, M., GOSSOP, M. & STRANG, J. (1998) Diversion tactics: how a sample of drug misusers in treatment obtained surplus drugs to sell on the illicit market, International Journal of Drug Policy, 9, 159-167.
FOUNTAIN, J., GRIFFITHS, P., FARRELL, M., GOSSOP, M. & STRANG, J. (1999) Benzodiazepines in polydrugusing repertoires: the impact of the decreased availability of temazepam gel-filled capsules, Drugs: Education, Prevention and Policy, 6, 61-69.
GARFOOT, A. (1996) Letter, Time Out, August 21-28. GERADA, C. & TIGHE, J. (1999) A review of shared care protocols for the treatment of problem drug use in England, Scotland, and Wales, British Journal of General Practice, 49, 125-126.
GLANZ, A. & TAYLOR, C. (1986) Findings of a national survey of the role of general practitioners in the treatment of opiate misuse: extent of contact with opiate misusers, British Medical Journal, 293, 427430.
GHODSE, H. (1995) Drugs and Addictive Behaviour: a guide to treatment, 2nd edn (Oxford, Blackwell).
GOSSOP, M., STRANG, J. & CONNELL, P H (1982) The response of out-patient opiate addicts to the provision of a temporary increase in their prescribed drugs, British journal of Psychiatry, 141, 338-343.
GOSSOP, M., BATTERSBY, M. & STRANG, J. (1991) Self-detoxification by opiate addicts: a preliminary investigation, British Journal of Psychiatry, 159, 208-212.
Gossor, M., MARSDEN, J., STEWART, D., LEHMANN, P. & STRANG, J. (1999) Methadone treatment practices and outcome for opiate addicts treated in drug clinics and in general practice: results from the National treatment Outcome Research Study, British Journal of General Practice, 49, 31-34.
GROVES, P., HEUSTON, J., DURAND, M. A., ALBERY, I., Gossor, M. & STRANG, J. (1996) The identification and management of substance misuse problems by general practitioners, Journal of Mental Health, 5, 193-193.
GRUER, L., Wasox, P., Scurr, R., ELLIOT, L., MACLEOD, J., HARDEN, K., FORRESTER, E., HINSHELWOOD, S., MCNULTY, H. & SILK, P. (1997) General practitioner centred scheme for treatment of opiate dependent drug injectors in Glasgow, British Medical journal, 314, 1730-35.
HAMMERSLEY, R., LAVELLE, T. & FORSYTH, A. (1990) Buprenorphine and temazepam abuse, British journal of Addiction, 84, 301-303.
HAW, S. (1993) Pharmaceutical Drugs and Illicit Drug Use in Lothian Region (Edinburgh, Centre for HIV/ 4 AIDS and Drug Studies (CHADS), City Hospital).
HO/VIE OFFICE (1997) Home Office Statistical Bulletin, issue 22/97 (London, Government Statistical Service).
INCIARDI, J. A. (1977) Methadone Diversion: experiences and issues, publication no. (ADM) 77-488 (Washington DC, US Department of Health, Education, and Welfare).
JONES, S. & POWER, R. (1990) observation to intervention: drug trends in West London, International Journal of Drug Policy, 2, 13-15.
KLEE, H., FAUGIER, J., HAYES, C., BOULTON, T. & MORRIS, J. (1990) AIDS-related risk behaviour, polydrug use and temazepam, British Journal of Addiction, 85, 1125-1132.
LANGROD, J., GALANTER, M. & LOWINSON, J. (1974) Illicit methadone abuse, in: SENAY, E., SHORTY, V. & ALKSNE, H. (Eds) Developments in the Field of Drug Abuse: National Drug Abuse Conference, pp. 461-466 (Cambridge, Massachusetts, Schenkman).
LAUZON, P., VINCELETTE, 3., BRUNEAU, J., LAMOTHE, F., LACHANCE, N., BRABANT, M. & SOTO, J. (1994) Illicit use of methadone among IV drug users in Montreal, journal of Substance Abuse Treatment, 11, 457-461.
MARKS, J. (1994) Deaths from methadone and heroin, Lancet, 343, 976.
McGurn-iv, J. H. (1997) More people die from methadone misuse than heroin misuse, British Medical Journal, 315, 603.
McDEttmorr, P. & MCBRIDE, W. (1993) Crew 2000: peer coalition in action, Drug/ink, 8, 13-14. McLEon, I. (1995) Letter, British Medical Journal, 310, 1407-1408.
MCKEGANEY, N. (1988) Shadowland: general practitioners and the treatment of opiate abusing patients, British Journal of Addiction, 83, 373-386.
METREBIAN, N., SHANAHAN, W. & STIMSON, G. V. (1996) Heroin prescribing in the United Kingdom: an overview, European Addiction Research, 2, 194200.
METREBIAN, N., SHANAHAN, W., WELLS, B. & STIMSON, G. V. (1998) Feasibility of prescribing injectable heroin and methadone to opiate-dependent drug users: associated health gains and harm reductions, Medical Journal of Australia, 168, 596-600.
Morr, J. (1994) Notification and the Home Office, in: STRANG, J. & Gossor, M. (Eds) Heroin Addiction and Drug Policy: the British system, pp. 270-289 (Oxford, Oxford University Press).
NEWCOMBE, R. (1996a) Live and let die: is methadone more likely to kill you than heroin? Druglink, I1, 9-12.
NEWCOMBE, R. (1996b) A reply to Ward et al. (letter), Addiction, 91, 1728-1729.
NIDA (1993) Impact of Prescription Drug Diversion Control Systems on Medical Practice and Patient Care, NIDA Research Monograph 131 (Rockville MD, National Institute on Drug Abuse).
PARKER, H. & KIRBY, P. (1996) Methadone Maintenance and Crime Reduction on Merseyside, Crime Detection and Prevention Series Paper 72 (London, Home Office Police Research Group).
PARAMESHWAR, E. (1995) Letter, British Medical Journal, 28 May.
PERNEGER, T. V., DEL Rio, G. F. & MINO, A. (1998) Randomised trial of heroin maintenance programme for addicts who fail in conventional treatments, British Medical Journal, 317, 13-18.
PHARMACEUTICAL JOURNAL (1993) News item, Vol. 250, March 27.
PHARMACEUTICAL JOURNAL (1996a) News item, Vol. 256, March 9.
PHARMACEUTICAL JOURNAL (1996b) News item, Vol. 257, November 23.
PHARMACEUTICAL JOURNAL (1997a) News item, Vol. 258, March 15.
PHARMACEUTICAL JOURNAL (1997b) News item, Vol. 259, July 26.
Powis, B., GRIFFITHS, P., GOSSOP, M. & STRANG, J. (1996) The differences between male and female drug users: community samples of heroin and cocaine users compared, Substance Use and Misuse, 31, 529-543.
PRESTON, A. (1996) The Methadone Briefing (ISDD).
RAISTRICK, D., GODFREY, C., HAY, A., SUTTON, M., TOBER, G. & WOLFF, K. (1995) Prescribing Methadone, YARTIC Occasional Paper 7 (Leeds, Centre for Health Economics/Leeds Addiction Unit).
RETTIG, R. A. & YARMOLINSKY, A. (Eds) (1995) Federal Regulation of Methadone Treatment (Washington DC, National Academy Press).
RUBEN, S. M. & MORRISON, C. L. (1992) Temazepam misuse in a group of injecting drug misusers, British Journal of Addiction, 87, 1387-1392
SAKOL, M. S., STARK, C. & SYKES, R. (1989) Buprenorphine and temazepam abuse by drug takers in Glasgow—an increase,British Journal of Addiction, 84, 439-441.
SCOTT, R. A., BoRNErr, S. J. & MCNULTY, H. (1994) Letter, British Medical Journal, 308, 1438.
SEIVEWRIGHT, N. & DOUGAL, W. (1993) Withdrawal symptoms from high dose benzodiazepines in poly drug users, Drug and Alcohol Dependence, 32, 13-23.
SEIVEWRIGHT, N., DONMALL, D. & DALY, C. (1993) Benzodiazepines in the illicit drugs scene: the UK picture and some treatment dilemmas,International Journal of Drug Policy, 4, 42-48.
SHEEHAN, M., OPPENHEIMER, E. & TAYLOR, C. (1988) Who comes for treatment: drug misusers at 3 London agencies, British Journal of Addiction, 83, 311320.
SPEAR, B. (1994) The early years: the 'British System' in practice, in: STRANG, J. & Gossor, M. (Eds) Heroin Addiction and Drug Policy: the British system, pp. 3-27 (Oxford, Oxford University Press).
SPUNT, B., HUNT, D. E., LIPTON, D. S. & GOLDSMITH, D. S. (1986) Methadone diversion: a new look, Journal of Drug Issues, 16, 569-583.
STATIONERY OFFICE (1998) Tackling Drugs to Build a Better Britain: the Government's 10-year strategy for tackling drug misuse (London, The Stationery Office).
STIMSON, G. V., HAYDEN, D., HUNTER, G., METREBIAN, N., RHODES, T., TURNBULL, P. & WARD, J. (1995) Drug Users' Help-Seeking and Views of Services, a report prepared for The Task Force to Review Services for Drug Misusers (London, Department of Health).
STRANG, J. (1982) Personal view, British Medical Journal, 284, 972.
STRANG, J., SEIVEWRIGHT, N. & FARRELL, M. (1992) Intravenous and other abuses of benzodiazepines: the opening of Pandora's box? British Journal of Addiction, 87, 1373-1375.
STRANG, 3., SEIVEWRIGHT, N. & FARRELL, M. (1993) Oral and intravenous abuse of benzodiazepines, in: HALLSTROM, C. (Ed.) Benzodiazepine Dependence, pp. 129-142 (Oxford, Oxford University Press).
STRANG, J. & GOSSOP. M. (Eds) (1994) Heroin Addiction and Drug Policy: the British system (Oxford, Oxford University Press).
STRANG, j., SHERIDAN, J. & BARBER, N. (1996) Prescribing injectable and oral methadone to opiate addicts: results from the 1995 national postal survey of community pharmacies in England and Wales, British Medical Journal, 313, 270-272.
STRANG, J. & SHERIDAN, J. (1998) National and regional characteristics of methadone prescribing in England and Wales: local analyses of data from the 1995 survey of community pharmacies, Journal of Substance Misuse, 3, 240-246.
STRANG, J., BEARN, 3., FARRELL, M., FINCH, E., GOSSOP, M., GRIFFITHS, P., MARSDEN, J. & WOLFF, K. (1998) Route of drug use and its implications for drug effect, risk of dependence and health consequences, Drug and Alcohol Review, 17, 197-211.
STRANG, J., GRIFFITHS, P., Powis, B., FOUNTAIN, J., WILLIAMSON, S. & GOSSOP, M. (1999) Which drugs cause overdose amongst opiate misusers? A study of personal and witnessed overdoses, Drug and Alcohol Review, 18, 253-261.
TANTAM, D., DONMALL, M., WEBSTER, A. & STRANG, J. (1993) Can general practitioners and general psychiatrists be expected to look after drug misusers? Results from evaluation of a non-specialist treatment agency, British Journal of General Practice, 43, 470474.
THOMAS, P. D. (1994) Letter, British Medical Journal, 309, 53-54 (see also correction 309, 544).
VISTA HILL PSYCHIATRIC FOUNDATION (VHPF) (1974) Methadone diversion, Drug Abuse and Alcoholism Newsletter, 3, 4.
WAGSTAFF, A. & MAYNARD, A. (1988) Economic aspects of the illicit drug market and drug enforcement policies in the United Kingdom, Home Office Research Study 95 (London, HMSO).
WARD, J., MATTICK, R. & HALL, W. (1992) Key Issues in Methadone Maintenance Treatment (Australia, University of New South Wales).
WHEELDON, N. M. (1992) Wolff-Parkinson-White syndrome mimicking myocardial infarction on ECG-exploitation by a heroin addict, British Journal of Clinical Psychology, 46, 269-270.
WHYNES, D. K., BEAN, P. T., GIGGS, J. A. & WILKINSON, C. (1989) Managing drug use, British journal of Addiction, 84, 533-540.
WOLFF, K., FARRELL, M., MARSDEN, J., MONTEIRO, M. G., Au, R., WELCH, S. & STRANG, J. (1999) A review of biological indicators of illicit drug use, practical considerations and clinical usefulness, Addiction, 94, 1279-1298.
Correspondence to: Jane Fountain, National Addiction Centre, 4 Windsor Walk, London SE5 8AF, UK. Submitted 1st February 1999; initial review completed 18th May 1999; final version accepted 7th September 1999.
ISSN 0965-2140 print/ISSN 1360-0443 online/00/030393-14 OD Society for the Study of Addiction to Alcohol and Other Drugs Carfax Publishing, Taylor & Francis Ltd
Last Updated (Thursday, 23 December 2010 23:14)












