| Articles - Prison & probation |
Drug Abuse
AIDS, DRUGS AND RISK BEHAVIOUR IN PRISON: STATE OF THE ART
Kate Dolan, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, Australia
The study of HIV transmission, risk behaviours and prevention in the prison setting is a difficult but important task. The difficulties lie in gaining access to inmates, obtaining representative samples and reliable reports of risk behaviour, and collecting conclusive evidence of HIV transmission in prison. This area of research is important because the high level of inmate turnover means that HIV transmission in prison threatens HIV control in the community when inmates are released. Research is required to evaluate the effectiveness of HIV prevention measures in prisons as little such evidence exists. Most studies of HIV transmission in prisons have found few cases. This has been interpreted as HIV transmission being low in prisons. Yet there are. conditions in most prison systems that are conducive to the transmission of HIV but which also hinder detection of transmission. Approximately one-third of all inmates inject drugs while in prison but they serve short sentences and are therefore under-represented in annual cohort studies of transmission. The dramatic reduction in injecting risk -behaviour in community settings has not occurred in prisons. Efforts to prevent HIV infection will be undermined if concerted efforts do not include prisoners.
INTRODUCTION
Prisons are probably one of the most difficult settings for the study of HIV risk behaviour and transmission. This article will mainly cover prisons in developed countries as most of the literature comes from these countries. However, there has been an indication from at least one developing country, Thailand, that prisons can play a crucial role in the transmission of HIV (Wright et al., 1994).
After considering the characteristics of prisoners and ethics of prison research, this article reviews the literature on the prevalence of HIV infection among prisoners, the proportion of prisoners who are drug injectors and the risk behaviours in which prisoners engage such as drug injecting, tattooing and sexual activity. In order to improve our understanding of the likelihood of HIV infection in prison, the evidence of HIV transmission in prison is also reviewed and the notion of mixing, or the extent of intermingling of inmates that is integral to prison systems, is considered.
ATTRIBUTES OF PRISONERS AND PRISONS
Prisoners are failed risk-takers. They are predominately males aged between 20 and 40 years old and a group usually considered to be very sexually active. Most come from disadvantaged backgrounds and have low levels of education. Minority groups, such as blacks in the USA and Aboriginals in Australia, are vastly over-represented in prison populations. Alcohol (Wright, 1993) and drug problems (Dolan et al., 1995) are very common among prisoners worldwide. The prevalence of infections linked to drug injecting such as hepatitis B and C (Crofts et al., 1995) and sexually transmissible diseases (Cohen et al., 1992) are several times higher among prison entrants than among the general population. Female prisoners are generally more likely than male prisoners to report a history of drug injecting (35% vs 18%; Patel et al., 1990) and therefore to be infected with HIV (Vlahov et al., 199 1).
Correctional facilities can be stressful, crowded and violent places where drug withdrawal is common (Turnbull and Stimson, 1994). Although imprisonment has been shown in some studies to reduce drug use (Shewan et al., 1994), inmates have reported injecting drugs (Taylor et al., 1995) and engaging in homosexual activities (Dolan, 1994) for the first time while incarcerated. These have been attributed to boredom and the single sex nature of correctional establishments.
ETHICS OF PRISON RESEARCH
Research into special populations usually raises a number of ethical issues. Prisoners, haying lost many basic civil rights, are a particularly vulnerable group. The World Health Organization emphasised the importance of ethics committees in its guidelines for HIV research in prison: 'independent examination by an ethical review committee should be carried out for all research procedures in prisons and ethical principles must be strictly observed. The results of such studies should be used to benefit prisoners (WHO, 1993, p2).
One major role of ethics committees is to ensure that potential respondents or subjects are not harmed by research. But ethics committees also have the potential to produce long-term detrimental effects on the very populations they are trying to protect.
The lack of prison data has made it difficult to argue a case for implementing HIV prevention in correctional facilities. It was reported in a study of HIV transmission in a US prison that 'prior ethic committee review precluded individual interviews for high risk histories' (Brewer et al., 1988; p366). Consequently, the study was unable to determine whether HIV transmission occurred in prison or prior to prison. It was also impossible to obtain an appropriate denominator for the measurement of incidence, i.e. confining the population studied to those who reported engaging in risk behaviour in' prison rather than the entire study sample.
Inmates' knowledge, attitudes and behaviour were studied in Toronto in order to produce AIDS educational material. But the effectiveness of such material produced is likely to have been impaired as (permission to conduct (the) study was granted pro-, viding the behaviour questions did not inquire I about sex and drug use in prison' Joepell, 1992, p39).
The WHO guidelines on HIV in prison recommend studies of risk behaviour to inform planning policies and intervention, but they stipulate that 'prison administrations should not seek to influence the scientific aspects of such research procedures, their interpretation or their publication'( 1993, p2).
Collecting data on risk behaviours in prison is important because the absence of such data can be used to justify inaction. In the UK, for example, 'Home Office ministers have not been convinced that making condoms available for use in prison, would be appropriate or helpful' (Groves, 1991).
This suggests that the ministers leave open the possibility that in the future they may be convinced of the appropriateness of providing condoms in prison. They have, however, ruled out the possibility of syringe exchange: 'even though the [prison medical] service recognises that some inmates will gain access to injectable drugs and will share injecting equipment, needle exchange schemes in prison cannot be contemplated' (Groves, 1991).
Most prison authorities have had policies to test prison entrants for HIV infection (Harding and Schaller, 1992). Sometimes this has been on a mandatory basis even though voluntary testing can be just as accurate in determining HIV prevalence (Hoxie et al., 1990). However, in a voluntary pilot HIV testing programme among inmates in London, onlyO.3% of the 54% who agreed to participate tested positive. This was probably an underestimate as another study found 5% of recently released prisoners were infected in 1990 (Turnbull et al., 1992). This low level of compliance may be partly a result of the restrictions imposed on infected inmates orinmates thought to be infected (Turnbull et al., 1993). Infected inmates are often segregated which precludes confidentiality of their HIV status (Harding and Schaller, unpublished).
DUTY OF CARE
The American AIDS Litigation Project examined the legal aspects of AIDS (Gostin, 1990). According to the 8th Amendment in the US constitution, US prisoners are to he protected from cruel and unusual punishment. This is considered to include contracting communicable disease. Claims that compulsory screening and segregation are necessary to prevent HIV transmission in prison have been rejected by US courts on the grounds of insufficient evidence. But the necessity of providing AIDS education in prison has been recognised by US courts, as failure to provide it can create distress (which is considered tantamount to cruel and unusual punishment).

PREVALENCE OF HIV AND AIDS
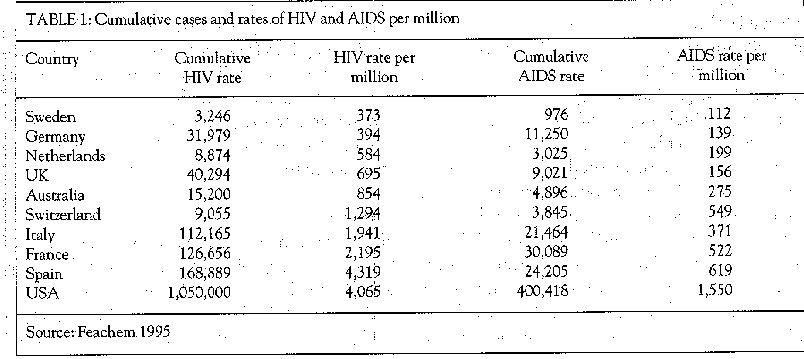
By 1995, more than one million cases of AIDS had been reported to the World Health Organization (WHO, 1994). A comparison of estimated cumulative incidence and rates of HIV and AIDS per million of population in eight European countries, Australia and the USA appear in Table 1. The USA, Spain, France and Italy have some of the highest rates of HIV infection - between 2000 and 4000 cases per million population.
HIV INFECTION AMONG INMATES
HIV infection is more prevalent in prison populations than in the corresponding community because of the increased prevalence of HIV infection in injecting drug users (IDUs) and the high proportion of IDUs in prison populations (Harding, 1987). As early as 1988, about half of the inmates in Madrid prisons (Estebanez et al., 1988) and 20% of prisoners in New York City tested HIV positive (Truman et al. , 1988). Within prison populations, certain groups have higher levels. In 10 US correctional systems, infection levels were higher among women (15 %) than men (8 %), among younger women (5 %) than younger men (2%), and among non Caucasians (5%) than Caucasians (3%) (Vlahovetal., 1991). It was estimated that in New York state prisons in 1988, there were 2200 male and 200 female HIV positive entrants, making HIV the leading medical problem among inmates (Smith et al., 1991).
HIV surveillance has been the most common form of HIV research in prison (Table 2). HIV prevalence among prisoners has ranged from 0% in Iowa, USA in 1986 (Glass et al., 1988) to 34% in Catalonia, Spain in 1989 (Martinet al., 1990). The high prevalence reported among Spanish prisoners reflects the high prevalence of HIV among IDUs and their considerable over-representation in the prison population.
EVIDENCE OF HIV TRANSMISSION IN PRISON
Demonstration of HIV transmission in prison has proven to be remarkably difficult. Of the seven published studies investigating HIV transmission in prison, six failed to prove conclusively that transmission had occurred in prison and all six concluded that such transmission was rare. However, these six studies sampled only long-term prisoners. Paradoxically, this group is probably at a lower risk of infection than short term prisoners because they reside in maximum security institutions where opportunities to associate, engage in risk activity and become infect, ed are more restricted in comparison with inmates in lower security institutions.
The only study to conclusively demonstrate significant HIV transmission in prison setting (Tayloret al., 1995) was fortuitously prompted by several acute cases of hepatitis B infections. These infections, along with two possible primary HIV infections, suggested surprisingly high levels of risk behaviours. (This study is described on page 10 as Study T)
The most common methodology used to study HIV incidence in prison has been repeated mass screening of inmates, usually on entry and annual follow-up. This method underestimates HIV incidence for several reasons. Prisons are dynamic institutions where the number of annual prison entrants and internal transfers is usually double and treble the daily census. With so many movements into, out of and around the prison system, annual cohort studies will over-represent inmates with longer sentences who are less likely to become infected with HIV Conversely, drug-using offenders who are at most risk of infection in prison will be under-represented in cohort studies as they tend to be held on remand (awaiting trial) or serve short sentences.
The next most common methodology is studies of inmates incarcerated for very lengthy periods. The extensive duration of imprisonment suggests that it is highly unlikely that the inmates could have acquired HIV infection before imprisonment and still be alive. However, the main shortcoming with these studies is that the denominator for the number infected is unknown and so rates of transmission can, not be estimated.
In the following section, evidence of HIV transmission in prison from reports and studies was considered in three ways. Evidence was considered first on the strength of methodology to demonstrate transmission; second, on the extent of transmission that may have occurred; and third, on aspects of the study design that may have influenced the results.
Report I
HIV infection among IDUs presenting for drug treatment in Bangkok rose from 2% in early February to 2 7% by early March in 198 7 (Wright et al., 1994) and up to 43% in September 1988 (Choopanya, 1989). The dramatic increase closely followed an amnesty on the king's birthday when numerous prisoners were released. Substantial HIV transmission in prison is believed to have been responsible for rapid dissemination of HIV (Wright et al., 1994).
This study was only suggestive of transmission having occurred in prison, but indicated that the extent can be potentially considerable.
Report 2
In New York, six HIV- infected inmates were identified who had been incarcerated without interruption before infection became prevalent in their communities (Gaunay and Gido, 1986).
This evidence is only suggestive of HIV infection in prison and there was no indication of the extent of transmission as no denominator was provided.
Report 3
In Australia, one inmate was reported to have tested negative after six years in prison and then tested positive while incarcerated without interruption. Medical files confirmed his reports of severe symptoms were consistent with primary HIV infection (Dolan et al., 1994a) .
This can be regarded as a definite case of HIV infection occurring in prison, but no indication of the extent of transmission can be made.
Study I
HIV testing was offered to inmates who had been imprisoned in Maryland for at least seven years in 1985. Of 137 (38%) inmates who accepted testing, two 0%) infected inmates were detected both of whom had been incarcerated for nine years. The unknown effect of selection bias was acknowledged by the authors (Centers for Disease Control, 1986).
The possibility that the inmates were infected before entering prison cannot be excluded. The extent of reported transmission was very low, but the study sampled only long-term prisoners and the extent of transmission may have been underestimated.
Study 2
In Florida, 87 of 556 prisoners (16%) who had been continuously incarcerated since 1977 had an HIV test result recorded in their prison medical files by 1991. A positive test result was recorded for 18 (2 1 %) of these inmates. Eight of these (44%) were still without symptoms at the end of 1991,whichsug, gests that HIV infection occurred in prison. The authors acknowledged that the evidence of prison transmission was presumptive, although strong. The authors suggested that a great deal of sexual activity was occurring in prison and recommended condom provision (Mutter et al., 1994).
The evidence of infection occurring in prison was strong, but not beyond doubt. Again, the sample studied consisted of long-term prisoners who are probably at lower risk.
Study 3
Only I % of 913 inmates in a US maximum security military prison tested HIV positive in 1983 (Kelley et al., 1986). Repeated testing of the 542 inmates who were still incarcerated at a follow-up in 1985 found no cases of seroconversion (95% confidence interval 0% to 0.5%). These data represent 685 person-years of incarceration. Data representing an additional 641 person-years of follow-up were obtained by pairing 199 specimens collected in July 1985 with samples collected in May 1982, but again no new HTLV-111 (HIV) infections were detected. This gave a combined annual seroconversion rate of 0% (95% Cl 0% to 0.2%). Some segregation of HIV positive inmates occurred. However, 25 hepatitis B seroconverters were identified by pairing sera collected during the same period giving an annual incidence of 2%forHBV
No evidence of HIV transmission was detected in this study. However, the only data presented on the sample suggests that this military sample was atypical of civilian prison populations. In the sample, 15% and 38% of inmates had drug and sex offences, respectively. As these proportions in the general prison population are usually reversed, it would be unwise to generalise to other prison systems. As previously indicated, inmates in maximum security generally have very limited opportunities to associate with other inmates, engage in risk behaviour and to become infected with HIV The policy of segregating HIV infected inmates may also have reduced the risk of HIV transmission. No information was provided on how the 913 inmates who were tested had been selected. The follow-up rate was low (59%) although the duration of follow-up was long (mean = 15 months; 542 inmates represented 685 person-years of prison).
The 2% incidence for hepatitis B was high, but it was not possible to determine whether these transmissions occurred in prison. Also, no information was provided on the baseline prevalence of hepatitis B, risk behaviours or whether these inmates were segregated. Although no evidence of HIV transmission emerged, the extent to which generalisations can be made from a maximum security military prison to prisons with different security levels or with a civilian population is unclear.
Study 4
A total of 7% of 422 prison entrants in Maryland tested positive for HIV in 1985. Infected inmates were more likely to be non-violent offenders, committed in Baltimore City and be black. Repeat testing of 393 prisoners (representing 482 prison-years) in 1987 detected two prisoners who had seroconverted in prison. They had been incarcerated for 69and 146 days at baseline testing. HIV incidence was 0.41 % per prison year (Brewer et al., 1988).
Inmates who refused to participate or were missed in the follow-up were significantly more likely to have been committed for a drug offence, be black or have a sentence of less than five years. Furthermore, inmates who had been released before generating eligibility lists differed on most characteristics from those enrolled in the study. These characteristics were thought to be associated with shorter sentence lengths. The authors noted that 'prior ethic committee review precluded individual interviews for high risk histories'(1 988, p366).
Although the study demonstrated HIV transmission had occurred, it was unclear whether inmates had become infected before or during imprisonment. The study concluded that the extent of transmission was limited to two inmates. However, 83% of all prison entrants were excluded from the study and excluded inmates were similar to inmates who were infected at entry. The study sample under-represented drug injectors who would be at a far greater risk of HIV infection than other prisoners. This suggests that the study design may have resulted in transmission being underestimated. Nevertheless, application of this incidence figure to the Maryland prison population indicates that 60 HIV infections occur annually (Hammett et al., 1993).
Study 5
All prison entrants and all current inmates in Nevada were tested for HIV in 1985. In each group 2% were found to he positive. Repeat testing of 1069 inmates nearing release detected three inmates who had seroconverted in prison. Those inmates had spent 130, 20 and seven days in prison when they testing negative. The sample represented 1207 person-years of imprisonment and provided a seroconversion rate of one person per 604 prison-years (0.2%). The authors concluded that the reported rates were maximum estimates of transmission and that HIV transmission among inmates in Nevada was rare (Horsburgh et al., 1990).
It was unclear whether the infections occurred in prison as inmates had only been incarcerated for a relatively short period before they tested negative. The extent of transmission was limited to three inmates becoming infected. However, inmates on short sentences were under-represented and, consequently, incidence may also have been under-represented.
Study 6
HIV prevalence among all prison entrants in Illinois was 3.3% in 1988 and 3.9% in 1989. Among inmates who had already served one year, 3.2% were positive in 1989. After one year, eight inmates who had tested negative at baseline had later tested positive. HIV incidencewasO.33% (95% Cl 0. 14% toO.64%) among the 2390 susceptible inmates (Castro et al., 199 1).
The evidence of transmission in prison was' strong but infection could have still occurred before incarceration. The extent of transmission was higher than all other studies but was still low. The study relied on mass screening over a one-year period which meant short term prisoners were missed.
Study 7
An investigation was prompted by several acute cases of hepatitis B infection and two primary HIV infections in a prison in Glasgow. Of 636 inmates at Glenochil Prison between I January and 30 June 1993, 378 inmates (59%) were still incarcerated when the investigation was launched. Among the 258 inmates who were not present, most (74%) had been transferred to other prisons and the rest (26%) had been released. Of the 378 inmates still incarcerated, 60% accepted counselling. Uptake of counselling ranged from 43% to 84% in the 11 subunits in Glenochil Prison. Many of those who declined counselling were believed to be injectors from a subunit of the prison where injecting was particularly prevalent. Of the 227 inmates counselled, one-third (33%) had a history of injecting. Almost half (4 3%) of IDU prisoners admitted injecting in Glenochil Prison. Of these 33 injectors, 29were tested for HIV and 14 were positive (48%).
Although only 38% of drug injecting inmates were tested, there was a strong association between becoming infected and injecting in prison in early 1993 (p<0.01). Fifteen inmates who had injected in Glenochil tested negative but were still in the window period for HIV seroconversion at the time of the study.
Definitive evidence that HIV infection had occurred in prison was based on early banding patterns on Western Blot tests, antigen results, HIV negative and positive test results, primary symptomatic HIV infection and dates of incarceration. Of the 14 infected inmates, definite evidence of HIV transmission in prison existed for eight, of whom six had become infected in Glenochil Prison, while the possibility of infection in another prison could not be excluded for two others. Another six infections also possibly occurred in prison, but infection occurring outside prison could not be excluded. All inmates infected in prison reported extended periods of sharing syringes.
This study differed from previous studies in three ways: first, it comprised a methodical approach to an apparent outbreak; second, it used precise biological measures to provide irrefutable confirmation of behavioural data; and third, risk behaviour data were collected. It was unfortunate that the inmates who had been transferred to other prisons or released were not followed up. However, the official report speculated on the possible extent of the outbreak in Glenochil (Scottish Affairs Committee, 1994) after discussions with prison medical officers and estimated that, assuming untested inmates were as likely to be IDUs (and therefore become infected) as those who had been tested, then the total number of infected inmates would be between 22 and 43 inmates (compared with the eight detected cases). They also acknowledged that 258 inmates were missed because theywere either transferred (74%) or released (26%) within the six month study period and that some of these may have been infected.
OTHER EVIDENCE
Two studies that employed mathematical modelling techniques estimated the potential for HIV to spread among prisoners. They concluded that approximately 62 prisoners become infected in England (Medley et al., 1992) and 38 in New South Wales (Dolan et al., 1994b) each year.
RISK BEHAVIOUR
Injecting drug use and homosexuality are not commonly reported in general populations. Less than I % of respondents reported a history of injecting drug use while 6% of males reported a homosexual experience (Johnson et at., 1992) in a large-scale English study (n = 18,876). The rate of injecting in 17 European countries has ranged from 30 to 230 per 100,000 of population (European Centre, 1994).
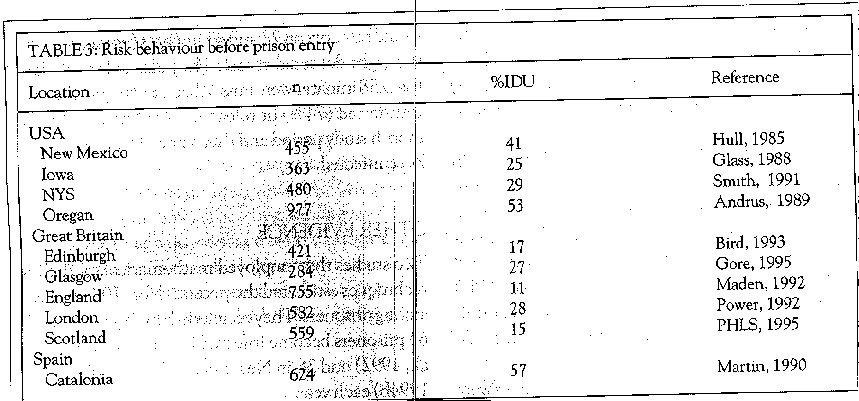
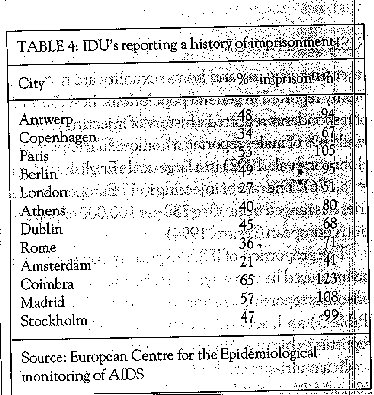
The proportion of IDUs in prison populations can be measured in two ways. First, by the proportion of prisoners reporting a history of injecting drug use (see Table 3) and, second, by the proportion of IDUs reporting a history of imprisonment (see Table 4).
In a multi-site study of IDUs in Europe, between 20 and 57% of IDUs reported a previous incarceration on a mean of two occasions. With few incentives to report either a history of injecting or imprisonment, these figures would probably be underestimates. In this study, only 27% of IDUs in London reported a history of imprisonment, whereas three other studies of IDUs in London found previous imprisonment rates of more than 50% (Dolan et al., 1993).
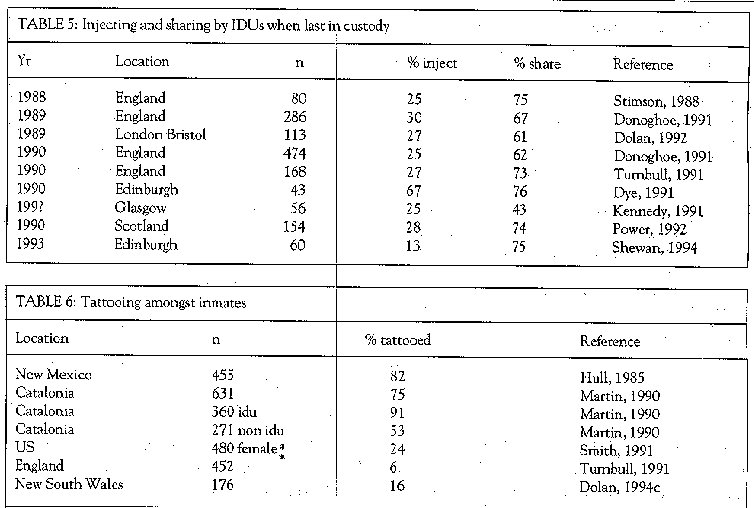
Being in prison does not necessarily mean that IDUs will engage in risk behaviour. Indeed, IDUs are more likely to stop injecting than continue while in prison (Shewan et al., 1994). Approximately one in four injectors reported continuing to inject drugs while in prison in the UK (see Table 5). Likewise, injecting in prison is not a risk for HIV unless syringes are shared. Therefore, ascertaining the likelihood of sharing is crucial to understanding the potential for HIV spread in prison. Injecting equipment is scarce in prisons and, therefore, is often shared (see Table 5). Even though fewer IDUs inject in prison, a higher proportion of IDUs overall share in prison than in the community (Dolan et al., 1996). While only one quarter of IDUs imprisoned in the UK were injecting, approximately two-thirds of these shared syringes while incarcerated.
Based on current UK data, we can estimate that for every 100 IDUs in a one-year period, 20 will go to prison, five will inject in prison and three of these will share syringes. With the number of IDUs in England (conservatively) estimated to be 75,000 (Advisory Committee on the Misuse of Drugs, 1988), then, each year, approximately 15,000 IDUs are likely to be imprisoned of whom 3750 IDUs will inject and 2475 IDUs will share injecting equipment while in prison.
PRISON INJECTING EQUIPMENT
Few qualitative data exist on HIV risk behaviour in prison. In one study, drug injecting was observed by an inmate in an English women's prison in the early 1990s. Atotalof92 injections were observed. Of the I I sets of injecting equipment that were known to exist, six sets were brought in by visitors, two sets by inmates after court appearances and three sets came from the hospital wing. Nine sets were known to have been shared by at least 41 individuals (mean 4.5 IDUs per set, range 28 IDUs per set). During five days, one set of injecting equipment was used by seven individuals in four areas of the prison (Pickering and Stimson, 1993).
During an amnesty at Oxford Prison in England, inmates were asked to surrender their syringes. HIV antibodies were detected in two of the three syringes surrendered (Farmer et al., 1989). In South Australia, examination of 58 syringes confiscated from prison revealed the following: most were I ml in size (95%), one quarter had visible blood, over a half showed signs of multiple use and two-thirds were refashioned, most commonly cut in half (Seamark and Gaughwin, 1994). The condition of syringes in prison has not been taken into account when guidelines for cleaning injecting equipment have been devised.
TATTOOING IN PRISON
Few studies have investigated tattooing in prison (see Table 6). In Norway, tattooing was found to be associated with hepatitis C infection among prisoners (Holsen et al., 1993). A high prevalence of tattooing was found, especially among IDU prisoners. Tattooing may provide a link between non- injecting and injecting inmates, thus enabling blood-borne infections to be disseminated. Only 6% of ex-prisoners in England reported being tattooed during their last imprisonment, but half of those reported sharing the tattoo implements (Turnbull et al., 199 1). However, the number of IDUs recruited in this study was limited which probably accounts for the low prevalence of tattooing reported.
SEXUAL BEHAVIOUR
The third risk behaviour of importance in the prison environment is male-to-male sexual activity. Correctional facilities can help control sexually transmitted diseases at the population level by treating large numbers of infected inmates, many of whom serve short sentences (Cohen et al., 1992). A total of 10% of inmates in a New York City j ail had acquired gonorrhoea during a three-month period in 1986 (van Hoeven et al., 1990) which apparently persuaded prison administrators that condom distribution was justified.
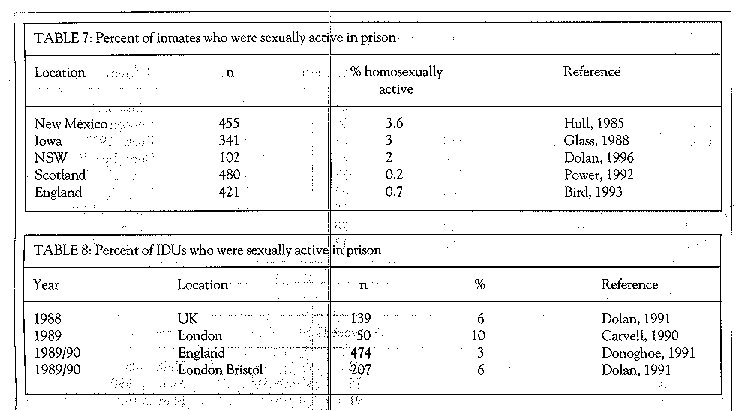
Few male prisoners report being sexually active in prison (see Table 7). Slightly more male IDU prisoners report male-to-male sexual activity (see Table 8). Some prisoners are particularly vulnerable to sexual assault, such as young prisoners (Heilpern, 1995) and transgender prisoners (Dolan et al., 1996).
HIV POSITIVE INMATES
The risk behaviours of HIV infected inmates, which determines the extent of HIV spread in prison, have been studied in New South Walesl South Australia, England and Scotland. HIV-positive IDUs were significantly more likely to inject in prison than IDUs who were HIV negative or unaware of their HIV status in England (Dolan et al., 1990) and in Scotland (Dye and Issacs, 199 1 ). Virtually all HIV infected inmates who had injected also reported sharing injecting equipment. In NSW, HIV-infected inmates were significantly more likely to have sex in prison than uninfected ones (Dolan et al., 1996).
ASSOCIATIONS WITH IMPRISONMENT
HIV infection has been associated with imprisonment in France (Richardson et al., 1993) and Spain (Granados et al., 1991). Almost half (48%) of those imprisoned on four or more occasions in Spain were infected, compared with one-fifth (2 1 %) of those imprisoned less often. Injecting drug use before imprisonment was the most common exposure category for HIV positive inmates in New York (Vlahov et al., 199 1).
Factors identified with syringe sharing among Scottish prisoners were: injecting a wide range of drugs in prison; using temgesic; and discontinuing methadone treatment on prison entry (Shewan et al., 1994).
MIXING
From an epidemiological perspective, prisons play a pivotal role in the random mixing of disparate individuals. For example, the daily prison census in NSW in 1993 was approximately 6000. Yet 14,000 individuals entered and were released from the prison system while a staggering 20,000 internal transfers of inmates occurred (NSW Department of Corrective Services, 1994). Although nearly all prisoners are eventually released, about half will be reimprisoned at some stage. The random mixing promoted by inmate movement is common to many prison systems but is not generally understood. Those unfamiliar with prison systems often perceive offenders as being isolated from society for extended periods. Nothing could be further from reality.
CONCLUSIONS AND RECOMMENDATIONS
The approach of most prison authorities to HIV infection conflicts with that of authorities in community settings. Prison authorities in many jurisdictions have vigorously pursued HIV testing programmes in preference to implementing prevention strategies. Therefore, HIV prevalence among prison entrants has been well documented in most countries (although England and Wales are exceptions). In addition, ample data exist on inmates risk' behaviours in a number of countries.
One of the major challenges lies in collecting definite evidence of HIV transmission occurring in prison. Transmission data may best be obtained by a case study approach involving short-term prisoners.
While prisons have the potential for transmitting infections, such as HIV and tuberculosis, they also present opportunities to provide prevention and treatment to a vast number of individuals. But correctional authorities are often (understandably) conservative in their management of prisons and prison medical services are almost always under-funded. These two factors have resulted in poor health care for prisoners, which are a very disadvantaged population compared with community members. The medical case load would be proportionally greater among prison populations and, therefore, prison medical services require proportionately more funding.
Prisoners are a very vulnerable population in many ways and are often treated in a manner that has no parallel in the community. It has been recommended that 'for practical and ethical reasons, measures for the control of AIDS in the prison environment should follow closely the strategy for the community in general. This policy implies an approach based on individual responsibility, in which each prisoner is treated as being autonomous and personally responsible for his own health and for the consequences of his behaviour. Prisoners should be informed about AIDS risk and given the opportunity to take prophylactic measures' (Hardling, 1987, p1262).
The notion of mixing, as mentioned earlier, bias potentially dire consequences for public health, as experienced in Bangkok. The general population needs to be informed about the vast level of intermingling that prison systems promote. Perhaps then the priority of infection prevention among prisoners may receive the attention it deserves. Prison authorities need to be reminded of their duty to care for those in their custody. Some successive attempts to improve a number of HIV issues in prison have been the result of lengthy court battles.
ACKNOWLEDGEMENTS
I wish to thank the Psychiatrische Universitatsklinik of Berne for inviting me to present the paper based on this article at the Conference. 1 am very grateful to the Swiss Federal Office of Health for generously funding my visit.
REFERENCES
Acedo A, CamposA, BauzaJ, Ayala C,Jove, M, Herrero L, Canigral G, Tascon A (1989). HIV infection, hepatitis and syphilis in Spanish prisons. The Lancet July 22: 226.
Advisory Committee on the Misuse of Drugs (1988). AIDS and DrugMisuse. London: HMSO.
Andrus JK, Fleming DW, Knox C, McAlister RO, Skeels MR, Conrad RE, Horan JM, Foster LR (1989). HIV testing in prisoners: Is mandatory testing mandatory? AJPH 79 (7): 840-842.
Bird AG, Gore SM, Jolliffe DW, Burns SM (1992). Anonymous HIV surveillance in Saughton prison Edinburgh. AIDS 6: 725-33.
Bird AG, Gore SM, Jolliffe DW, Burns SM (1993). Second anonymous HIV surveillance in Saughton prison. Edinburgh prisoners give a lead to other heterosexuals on being HlVtested.AIDS 7: 277-9.
Brewer TF, Vlahov D, Taylor E, Hall D, Munoz A, Polk F (1988). Transmission of HIV-1 within a statewide prison system. AIDS 2: 3637.
Carvell ALM, Hart GJ (1990). Risk behaviours for HIV infection among injectingdrug users. British MedicalJourrial300: 1383-4.
Castro K, ShanskyR, ScardinoV, NarkunasJ, CoeJ, Hammett T (1991). HIV transmission in correctional facilities. Paper presented at the VlIth International Conference on AIDS, Florence, 16-21 June. Abstract no: MC3067 p314
Centers for Disease Control (1986). Acquired immunodeficiency syndrome in correctional facilities: a report of the National Institute of Justice and the American Correctional Association. MMWR 35(12):195-9.
Choopanya K (1989). AIDS and Drug Addicts in Thailand, Bangkok. Bangkok: Bangkok Metropolitan Authority Department of Health.
Cohen D, Scribner R, Clarke J, Cory D (1992). The potential role of custody facilities in controlling sexually transmitted diseases. AJPH 82(4): 552-6.
CroftsN, StewartT, Hearne P, PingXY, BreschkinAM, Locamini SA (1995). Spread of blood-borne viruses among Australianprison entrants. 1374tishMedicalJourrial 310: 285-8.
Dixon PS, Flanigan TP, De Buono BA, Laurie JL, De Ciantis ML, Hoy J, Stein M, Scott HD, Carpenter CCJ (1993). Infection with the human immunodeficiency virus in prisoners: Meeting the health care challenge. The American Journal of Medicine 95: 629-35.
Dolan KA, Donoghoe M, Stimson G (1990). Drug injecting and syringe sharing in custody and in the community: an exploratory survey of HIV risk behaviour. The HowardJournal29(3): 177-186.
Dolan KA, Donoghoe MC, Jones S, Stimson GV (1992). A cohort study of syringe exchange clients and other drug injectors in England, 1989 to 1990. Report to the Department of Health. London: Monitoring Research Group, The Centre for Drugs and Health Behaviour, Charing Cross and Westminster Medical School, London.
Dolan KA (1993). Drug injectors in prison and the community in England. InternationalJournal ofDrug Policy 4 (4): 179-183.
Dolan K G 994). Sex in the stammer. National AIDS Bulk-tin 8: G 6, 12-13. Sydney: Australian Federation of AIDS Organisations, Sydney.
DolanK, HallW, Wodak A, Gaughwin M (1994a), Evidence of HIV transmission in anAustralian prison. Letter.MJA 160: G 734.
Dolan K, Kaplan E, Wodak A, Hall, W, Gaughwin M (I 994h). Modelling HIV transmission in NSW prisons, Australia. G Tenth International Conference on AIDS, Yokohama abstract no PD0524. pp336. H
Dolan K, Hall W, Wodak A (I 994c). Bleach availability and risk behaviour in prison in New South Wales. Technical Report No 22. Sydney National Drug and Alcohol Research Centre. H
Dolan K, Wodak A, Penny R (1995). AIDS behind bars: H preventing HIV spread among incarcerated drug injectors. AIDS 9: 825- 32.
Dolan K, Shearer J, Hall W, Wodak A (1996). Bleach is easier I~ to obtain but ininates are stilt at risk of infection in New South Wales prisons. Technical Report. Sydney National f Drug and Alcohol Research Centre.
Dolan K, Wodak A, Hall W, Gaughwin M, Rae F (1996). HIV risk behaviour before, during and after imprisonment in New South Wales. Addiction Research. 1 7
Donoghoe MC, Dolan KA, Stimson GV (199 1). The 1989 1990 National Monitoring Study. Monitoring Research Group. The Centre for Research on Drugs and Health Behaviour. Charing Cross and Westminster Medical f School, London.
Dye S, Isaacs C (199 1). Intravenous drug misuse among prison inmates: implications for spread of HIV. British MedicalJourna1302: 1506.
EstebanezP,ColomaC, ZunzuneguiMV,Rua&T (1988). Preva- Ilence and risk factors for HIV infection among inmates. IV International Conference on AIDS Stockholm, June Abstract no 4202.
European Centre for the Epidemiological Monitoring of AIDS J (1994). Surveillance of AIDS/HIV in Europe, 1984-1994. France: Saint Maurice.
FarmerR, Preston D, Emamij, BarkerM (1989).Thetransmissionof HIV within prisons and its likely effect on the growth of the epidemic in the general population. University of London.
Feachem RG (1995). Valuing the past ... investing in the future. Evaluation of the National HIV/AIDS strategy 1993-94 to 1995-96. Australian Government Publishing Service, Canberra.
Gaunay W, Gido R (1986). AIDS a demographic profile of New York State inmates mortalities 1981-1985. New York: New York State Commission of Correction.
Gellert GA, Maxwell RM, Higgins KV, et at (1993). HIV infection in the women's jail, Orange County, California, 1985 through 199 1. American Journal of Public Health 83 (10): 1454-56.
GlassGE, HauslerWJ, Loeffelholz PL, YesalisCE (1988). Seroprevalence of HIV antibody among individuals entering the Iowa prison system. AIPH 78(4): 447449.
Gore SM, Bird AG, Burns SM, Goldberg DJ, Ross AJ, MacgregorJ (1995). Drug injection and HIV prevalence in inmates of Glenochil prison. BMJ 310: 29 3-296.
Gostin LO (1990). The AIDS Litigation Project - A National review of courts and human rights commission decisions, Part 1: The social impact of AIDS. Law & Medicine 263 (14):1961-1970.
Granados A, Miranda MJ, Martin L (1990). HIV seropositivity in Spanish prisons. Presented at the VIth International AIDS Conference. San Francisco. Abstract no ThDl 16.
Groves T (1991). Prison policies on HIV under review. BMJ 303: 1354
Hammett TM, Harrold L, Gross M, Epstein J (1993). 1992 Update: AIDS in correctional facilities, issues and options. Abt Associates Inc.
HardingT (1987). AIDS in prison. The LancetNov 28:1260-63
HardingT, SchallerG (unpub). HIV/AIDS and prisons: update and policy review. June 1992, University Institute of Legal Medicine, Geneva.
Heilpern D (1995). Sexual assault of New South Wales prisoners. Current Issues in Criminaljustice 6: 3 27-334.
Holsen DS, Harthug H, Myrmet H (1993). Prevalence of antibodies to hepatitis C virus and association with intravenous drug abuse and tattooing in a national prison in Norway. EurJ Clin Microbiol Infect Dis 12 (9): 673-676.
Horsburgh CR, Jarvis JQ, McArthur T, Ignacio T, Stock P (1990). Seroconversion to human immunodeficiency virus in prison inmates. American Journal of Public Health 80(2): 209-10.
Hoxie NJ, VergerontJM, Frisby HR, PfisterJR, Golubjatnikov R, DavisJP (1990). HIVseroprevalence and the acceptance of voluntary HIV testing among newly incarcerated male prison inmates in Wisconsin. American Journal of Public Health 80(9): 1129-113 1.
Hull HF, Lyons LH, MarmJM, Hadler SC, Steece R, Skeels MR (1985). Incidence of hepatitis B in the penitentiary of New Mexico. American Journal of Public Health 75 (10): 1213 1214.
Johnson AM, Wadsworth J, Wellings K, Bradshaw S, Field J (1992). Sexual lifestyles and HIV risk. Nature 360: 3 December.
Kelley PW, Redfield RR, Ward DL, Burke DS, Miller RN (1986). Prevalence and incidence of HTLV- I 11 infection inaprison.JAMA 256(16):2198-99.
Kennedy DH, Nair G, Elliott L, Dittonj (1991). Drug misuse and sharing of needles in Scottish prisons. British Medicaljournal 302: 1507.
Maden A, Swinton M, Gunn J (1992). A survey of pre-arrest drug use in sentenced prisoners. British Journal of Addiction 87: 27-33
Martin V, BayasJM, LaligaA, PumarolaT, VidaIJ, Jimenez de Anta MT, Satleras L (1990). Seroepiderniology of HIV -I infection in a Catalonian penitentiary. AIDS 4: 1023-26.
Medley G, Dolan KA, Stimson G (1992). A model of HIV transmission by syringe sharing in English prisons using surveys of injecting drug users. Presented at the VIIIth International Conference on AIDS, Amsterdam. Abstract number MoD 0038, pp75.
Mutter RC, Grimes RM, Labarthe D (1994). Evidence of intraprison spread of HIV infection. Archives of Internal Medicine 154: 793-795.
NSW Department of Corrective Services (1994). Annual Report 1993-1994. Sydney.
Patel KK, Hutchinson C, Sienko DG (1990). Sentinel surveillance of HIV infection among new inmates and implications for policies of corrections facilities. Public Health Retorts 105(5):510-514.
Pickering H, Stimson GV (1993). Syringe sharing in prison. The Lancet 342: 4 September, 621-622.
PowerKG, Markaova 1, RowtandsA, Mckee KJ, AnstowPJ, KilfedderC (1992). Comparison of sexual behaviourand risk of transmissionof Scottish inmates, with or without a history of intravenous drug use. AIDS Care 40): 53-67.
Public Health Laboratory Service (1995). Unlinked anonymous HIV seroprevalence monitoring programme in England and Wales. London: Department of Health.
Scottish Affairs Committee (1994). Drug abuse in Scotland, Report. London: HMSO.
Seamark R, Gaughwin M (1994). jabs in the dark: Injecting equipment found in prisons, and the risks of viral transmission. AUSTJPH 180): 113-6.
Shewan D, Gemmell and DavisJB (1994). Behavioural change amongst drug injectors in Scottish prisons. Soc Sci Med 39(11): 1585-6.
Singleton JA, Perkins Cl, Trachtenberg Al, Hughes MJ, Kizer KW, Ascher M (1990). HIV antibody seroprevalence among prisoners entering the California correctional system. Westj Med 153: 394-9.
Smith PF, Mikl J, Truman Bl, Lessner L, Lehman JS, Stevens RW, Lord EA, Broaddus RK, Morse DL (199 1). HIV infection among women entering the New York State correctional system. Americanjournal of Public Health 81: 35-40.
Stimson GV, Alldritt L, Dolan KA, Donogh(V M (1988). Injecting Equipment Exchange Schemes: A FiAal Report on Research. London: Goldsmiths' College.
TaylorA, Goldberg D, EmslieJ, WrenchJ, Gruer L, Cameron S, Black J, Davis B, McGregor J, Follett E, Harvey J, Basson J, McGavigan J (1995). Outbreak of HIV infection in a Scottish prison. BMJ 3 10: 289-92.
Toepell A (1992). Prisoners and AIDS. Knowledge, Attitude and Behaviour. Ontario: National Clearing House on AIDS.
Truman BI, Morse D, Mikl J, Lehman S, Forte A, Broaddus R, Stevens R (1988). HIV seroprevalence and risk factors among prison inmates entering New York State Prisons. Presented at the lVth International Conference AIDS. Abstract no 4207.
Turnbull Pi , Dolan KA, Stimson GV (199 1). Prisons, HIV and AIDS: Risks and Experiences in Custodial Care. Horsham: Avert.
Turnbull P, StimsonG (1994). DrugUse in Prison. Letter. BNV 308:1716.
van Hoeven KH, Rooney WC, Joseph SC (1990). Evidence of gonococcal transmission within a correctional system. Americanjournalof Public Health 80(12): 1505-6.
Vlahov D, Brewer F, Munoz A, Hall D, Taylor E, Polk BF (1989). Temporal trends of Human Immunodeficiency Virus Type I (HIV- 1) infection among inmates entering a statewide prison system, 19851987.JAIDS2(3): 283-90.
Vlahov D, Brewer TF, Castro KG, N arkunas J P, Salive ME, Ullrich J, Munoz A (1991). Prevalence of antibody to HIV-1 among entrants to US Correctional Facilities. JAMA 265(9): 1129-32.
World Health Organization (1993). WHOGuidelines on HIV infection and AIDS in Prisons. Geneva: WHO.
Wright KN (1993). Alcohol use by prisoners. Alcohol Health & Research World 17 (2).- 15 7-6 1.
Wright NH, Vanichsem S, Akarasewi P, Wasi C, Choopanya K (1994). Was the 1988 HIV epidemic among Bangkok's injecting drug users a common source outbreak? AIDS 8: 529-32.












