| Articles - Opiates, heroin & methadone |
Drug Abuse
OFFICE-BASED METHADONE PRESCRIBING: ACCEPTANCE BY INNER CITY PRACTITIONERS IN NEW YORK
J E N N I F E R M c N E E L Y, E R N E 5 T D R U C K E R, P H D, DIANA HARTEL. DRPH, AND ELLEN TUCHMAN , CSW
Ms. McNeely and Drs. Drucker and Hartel are from the Department of Epidemiology and Social Medicine. Montefiore Medical Center and Albert Einstein College of Medicine; Ms. Tuchman is from the Beth Israel Medical Center, Methadone Maintenance Treatment Program. Correspondence: Ernest Drucker, PhD, Department of Epidemiology and Social Medicine, Division of Public Health and Policy Research, Montefiore Medical Center, 111 East 210th Street. Bronx, \Y 10467. (Email: This e-mail address is being protected from spambots. You need JavaScript enabled to view it )
INTRODUCTION
There is growing interest in office-based prescribing as a means of expanding and improving methadone maintenance treatment (MMT) in the US. Primary health care providers already are utilized widely as methadone prescribers throughout Europe, Australia, and Canada," and in some regions over 50%, of methadone is prescribed'. in the offices of general practitioners and is dispensed in community pharmacies.2-4 °
This approach has provided the chief means of expanding MMT availability and has played a key role in containing the acquired immunodeficiency syndrome (AIDS) epidemic among injection drug users in several countries. 5 In the US, however, this form of practice is restricted severely by federal and state regulations confining methadone maintenance to large, specialized clinics, 6-8 which serve fewer than 20% of the heroin -dependent population! To address the problems of treatment availability and quality, the Institute of Medicine of the National Academy of Sciences has called for the integration of methadone maintenance into standard medical practice, a view also supported by the 1997 National Institutes of Health Consensus Development Conference Effective Medical Treatment of Opiate-Addiction and by the White House Office of National Drug Control Policy. 10
In 1998, we began a study of office-based prescribing (National Institute on Drug Abuse (NIDAI ROI-DA11324) for a group of 100 patients enrolled in the MMT programs of Montefiore and Beth Israel Medical Centers and the Albert Einstein College of Medicine, which currently treat over 12,000 patients. As part of the process of identifying and recruiting clinicians to participate in the study, we surveyed practitioners within our institute's primary care and infectious disease clinic sites, from which we would draw our prescribers. All of this sample of practitioners were employed by the institution full time and provided continuous and comprehensive care for 1,500-2,000 patients each. While riot in private practice, they operated from neighborhood clinics that are typical of the system providing primary care to the city's poorer residents. We assessed prior experience with methadone patients in their medical practices, their attitudes toward MMT and their willingness to prescribe methadone within office-based practices.
METHODS
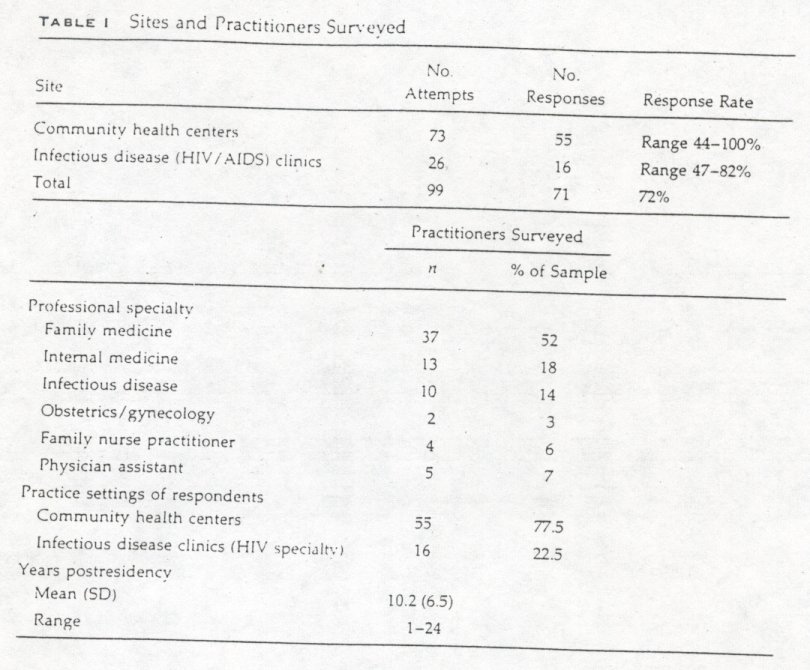
A 21-item survey was administered to primary care and human immunodeficiency virus (HIV)/AIDS providers (physicians, physician assistants, and nurse practitioners( in 11 practice sites of Montefiore, Beth Israel, and St. Joseph's Medical Centers in New York City and Yonkers. The survey was conducted at each practice site. with the questionnaire filled in by the interviewer, J. McNeely. Those providers who were unable to schedule an interview were asked to fill out the surv ey themselves and mail it, with telephone follow-up by the same interviewer: no differences were found in the two methods of responding.
SAMPLE
All respondents (physicians, physician assistants, and nurse practioners) worked in community -based primary care and HIV /AIDS clinics serving inner-city populations of the Bronx and Manhattan: 60-65% of patients receive Medicaid at the community health centers (Paul Meissner, personal communication, Montefiore Medical Center, April 21,1999), up to 77% at the HIV/AIDS clinics (Paul Meissner, oral communication, April 21, 1999; Millie Gonzalez-Haig, personal communication, Beth Israel Medical Center, April 21, 1999). Respondents were principally in family medicine, internal medicine, and infectious disease and had been practicing an average of 10.2 years (see Table 1). Of a total of 99 clinicians employed at the 11 sites, 71 (72%) agreed to participate in the survey.
RESULTS
PRIOR EXPERIENCE WITH METHADONE PATIENTS
Most of these clinicians had extensive prior experience providing medical care for methadone patients: 85% currently had MMT patients in their practices, with a median of four patients in their care at the time of the study (see Table If). Providers in practices that treated HIV/AIDS were most experienced with methadone patients, as expected given the co-occurrence of HIV and heroin use in New York City. They reported a median of 40 MMT patients in their practices
However, specific attitudes about the goals and length of methadone treatment varied substantially among this group. regarding, for example, whether limits should be set on its duration, if methadone should be withdrawn after the cessation of illegal drug use, and whether abstinence from all opioids, including methadone, should be the principal goal of treatment. These responses reveal some serious reservations on the part of many practitioners about the philosophy of indefinite maintenance treatment and suggest the need to address these issues in the training of prospective prescribers. Still, 52% supported setting no limit can the duration of maintenance treatment.
When asked to assess their knowledge about methadone pharmacology and clinical application (on a scale of 1 to 10), the average score was 5.5. Most cited their clinical training as the primary source for what they did know about methadone, but v ery few reported learning about MMT within a structured curriculum in medical school or during residency training. Still, 35% felt knowledgeable enough to prescribe methadone.
WILLINGNESS TO PRESCRIBE METHADONE WITHIN THEIR PRACTICES
Of all practitioners surveyed, 66% said that, given proper training and support, they would prescribe methadone for their patients. However, there is concern that the "multiple needs" of methadone patients maybe difficult to meet in these medical practice settings. Half (50%) of the providers shared this concern. In interview's, many practitioners saw the methadone patient population as having more complicated psychosocial needs and medical deficits than their average patient and called for additional supports.
Perhaps because they already saw the care of drug users as a substantial piece of their work, the HIV/ AIDS providers in this sample were most enthusiastic about prescribing methadone: 88% of them were ready to prescribe. They felt somewhat more knowledgeable about MM T than most primary care providers-94% of the HIV /AIDS practitioners (versus 63% of the primary care practitioners) were comfortable working with drug users, and they were less concerned that they would be unable to meet the multiple needs of methadone patients.
CONCLUSIONS
For the practitioners we surveyed, the question of prescribing methadone was not laden with fear about bringing drug users into their practices-indeed most already had. and continue to have, substantial experience with methadone patients. Rather, methadone was seer, as another useful tool for better managing the overall health of patients who are addicted.
However, there was concern among these practitioners about the substantial medical and psychosocial needs that such patients bring. Combined with acute awareness of the limited time available (under the current productivity pressures of outpatient medical practice and managed care) and the lack of adequate support staff (e.g., social workers, counselors, and case managers), this concern is realistic. HIV/AIDS providers generally felt less worried about the extra steeds of methadone patients, perhaps because of the more extensive ancillary support in these practices. If methadone is to be prescribed in the context of primary care medicine in this country, we should make efforts to provide such additional support, both for the benefit of the patient and for the ability of the practitioners to maximize the effects of methadone prescribing. This objective need not be an impediment to instituting office-based care of heroin addicts. The "shared care" system of general practice in the United Kingdom, in which addiction specialists and supplemental counseling and social services support a network of primary care physicians caring for methadone patients, may offer a suitable model."
Some recent work in the US suggests that a significant number of primary care providers are prepared to accommodate methadone prescribing within, their practices. The medical maintenance model"-employed for the most well-stabilized and socially integrated patients-is now developing in Connecticut, Washington, and California following 10 years of positive experience in New York. Over the past year as part of our NIDA research study, we have initiated rnethadone prescribing within primary care at our institutions, in which 15 primary care providers have assumed prescribing authority for 70 methadone patients currently enrolled in our MMT programs.
The principal finding of this study is that a significant proportion of these practitioners already were caring for the populations and communities most in need of more addiction treatment and were supportive of the current initiatives to extend methadone treatment to mainstream medical practice. Even at the caseload of our current study (3-5 patients per practitioner), the 47 respondents of this sample willing to prescribe methadone in their practices could accommodate 200 patients-the equivalent of a standard methadone clinic. At 10-20 patients each, they could care for 470-940-the equivalent of many large methadone programs. With additional training and proper ancillary support, it appears that a large potential workforce of rnedical providers is available and accepting of office-based prescribing within primary care and HIV/AIDS practices. Based on the growing body of evidence from abroad and our experience thus far in New York City, methadone prescribing can be integrated successfully into medical practice.
ACKNOWLEDGEMENT
This research was supported by NIDA R01 DA11324-01.
REFERENCES
1. Nadelmann E. McNceely I. Drucker F. International perspectives. In: Lowinson JH, Ruiz J', Millman Rl Langrod JG. editors. Substance Abuse: a Comprehensive Textbook. 3rd ed. Baltimore MD Williams and Wilkins; 1997:22-39.
2. Barrell M : t the Re g ulation and Delivery of Methadone in 12 Member ,taw s of the European union Luxembourg Office for Official Publications of the European Communing; 1996.
3. Sheridan J. Strang ), Barber \, Clanz A. Role of community pharmacies in relation to J II\' prevention and drug misuse findings from the 1995 national survey in England and Wales. BMJ 1996:313(7(1;2):272-274.
4. Muhleisen P, Lintzeris N, Koutroulis G et al. Evaluation of methadone dispensing in community pharmacies in Victoria. Aust Pharm Suppl. 1998;17(8):7-12.
5. Drucker (:. Lurie P, Wodak A. Alcabes P. Measuring harm reduction: the effects of needle and syringe exchange programs and methadone maintenance on the ecology ,+t HIV AIDS 1998:12(suppl A):3217-S230.
6. LS Food and Drug Administration. Sec. 291.501 and 291.505 (54 FR 8960. March 2, 1984; ;4 FR 12331: March 27, 1489).
7. Institute of Medicine. Federal Regulation of Methadone Treatment. Rettig RA, Yarmolinsky \. editors Washington DC: National Academy Press; 1995.
8. Dole VP . Hazards of process regulations: the example of methadone maintenance. 1A.\ L l 1970;267.2234-2233.
9. National Institutes Health. Effective medical treatment of opiate addiction. NIH Consensus Statement 1997 November 17-19;15(6):1-38.
10 Office of National Drug Control Mice. Consultation Document on Opioid Agonist Treat-wit! Washington 1)C. ONDCP 1998.
11.Wells P GP prescribing: putting "shared care" policy into practice. Paper presented at: !itch International Conference on the Reduction of Drug Related Harm. March 24, 1999. Geneva.
12 Novick DM. Pascarelli Ff. Joseph I I et al. Methadone maintenance patients in general medical practice 1.1.\1;1. 114~;;.2;0:3299-3303.












