| Articles - HIV/AIDS & HCV |
Drug Abuse
HIV prevention among drug users. Specialist or non-specialist provision. A conflict of ideologies
By Jan Keene, Gerry Stimson & Nina Parry-Langdon
The research in this study is based on an evaluation of five agency-based and three community-based syringe exchange schemes in Wales. This paper will discuss the problems of HIV prevention among drug users, particularly those in rural areas. It is suggested that HIV prevention services have been developed in many areas as an integral part of drug service provision, consisting of localised syringe exchange services based within drug agencies and offering a comprehensive package of advice about drugs, counselling and health care. This model of service provision (which could be called the ‘urban model’ of exchange) is not necessarily sufficient in reaching a range of clients with differing needs, nor are these localised services practical in rural areas with widely dispersed populations. Alternatives such as non-specialist, community-based dispersal/disposal facilities may provide a more realistic option for HIV prevention, particularly in rural areas or in areas where the present drug services are less readily adaptable to the ‘harm minimisation’ implicit within the concept of syringe exchange.
HIV prevention, drug use and syringe exchange
The response of administrators, managers and drug workers to people who inject drugs has changed in recent years as they adapt to the problems inherent in the prevention of HIV. The impact of HIV has induced various responses nationally and internationally. In England and Wales, the major response has been to develop syringe exchange projects of which there are now over 120 (Lart and Stimson 1990). The schemes are basically concerned with dispersing clean needles and syringes to drug users and providing linked disposal facilities. Continued access to clean equipment is, to some extent, dependent on the return of used needles and syringes. This service is provided free and usually from a particular base at regular times during the week. Syringe exchange schemes are often based in drug services or have links with these services (Lart and Stimson 1990), which enables them to serve other functions.
For example, many provide education about HIV risk behaviours, basic health care and access to other services. Stimson and colleagues (1988) have demonstrated that these schemes are effective in attracting clients - 30% of whom had not attended services previously. Such projects have also been shown to be fairly successful in making syringe dispersal contingent on the return of used equipment. For example, the return rate for schemes in Wales is nearly 80% overall. Accessibility is an important factor, as most clients travel on average less than two miles to reach services. Reduction in risk behaviour has been reported, and HIV risk behaviours are lower in those who attend schemes than amongst those who do not attend (Donoghoe 1989).
The theory and practice of syringe exchange involves a good deal more than simply the dispersal and disposal of equipment. In their report "NotJust a Syringe Exchange, Lart and Stimson (1991) have shown that many agencies in England offer a wide range of services in addition to syringes and needles, such as advice and help with social and psychological problems and health care.
This type of service provision is also reflected in drug agency-based schemes in Wales, where the following services are offered to clients attending most agencies: primary health care, advice and counselling on drug problems, advice on safer drug use and safer injecting, general counselling, advice on welfare rights, advice on safer sex, HIV counselling and testing, home visits and referral to other agencies.
In many drugs agencies in England, syringe exchange is seen as part of an overall health and harm minimisation package. This orientation has developed by integrating the notion of syringe exchange into pre-existing agency ideologies. The perceived aim of syringe exchange was often to create a contact with clients and client visits were seen by staff as a possible entr‚e to other services. Lart and Stimson (1991) conclude that, "If anything, the salience of the specific issue of HIV prevention as a reason for syringe exchange tended to get obscured by the other aspects of the service." It will be suggested in this paper that a similar situation exists in drug agency-based services in South Wales, though not for the non-specialist HIV prevention services in the North, where syringe exchange is less an integral part of drug service provision.
Development of syringe exchange in Wales: Achievements and constraints
Syringe exchanges were established in eight of the nine Health Authority Districts in Wales by the end of 1990 (See Table 1.) Responses to drug use and drug users in each of these districts had varied prior to the development of the projects. To understand the potential functioning and operational problems inherent in present-8ay syringe exchange projects, it is necessary to view them in the context of attitudes to drug use and service provision for drug users generally. The history of the development of syringe exchange in Wales has been influenced by earlier projects developed in urban areas in England, together with the necessity to adapt to varying population distributions and types of drug use, and perhaps most importantly the attitudes of local professionals in the drugs field.
Table 1: description of projects
| Date worker in post | Geography | Base | Worker | |
| South Glamorgan | 07/89 | City | Community Drug Team | Full time nurse |
| East Dyfed | 08/89 | Rural + small town | Drug Project | Full time nurse |
| Mid Glamorgan | 10/89 | Rural + large town | Community Drug Team | Full time nurse |
| Gwent | 11/89 | Rural + large town | Drug Project | Full time nurse |
| Powys | 04/90 | Rural | 3 bases | nil |
| Clwyd | 05/90 | Rural + small towns | 2 AIDS counselling | Part time AIDS counsellor |
| Gwynedd | 05/90 | Rural + town | 18 pharmacists | nil |
| West Glamorgan | 06/90 | City + 2 towns | 3 Drug Projects | Full time coordinator |
The type and degree of drug use in Wales varies, as in any country, from area to area. Opiate use is restricted largely to the towns in the South and Northern coastal and border towns, while amphetamine use is widespread across most of Wales, particularly in the Valleys. The extent of injecting drug use in Wales can be gauged by the number of pharmacists selling injecting equipment. Surveys of pharmacists are still not extensive, but the results of Glanz’s (1990) postal survey of 164 pharmacists in Wales showed that 26 had been asked for equipment in the past four weeks. The results of local surveys in South Wales illustrate that approximately 30% of pharmacists currently sell injection equipment to drug users.
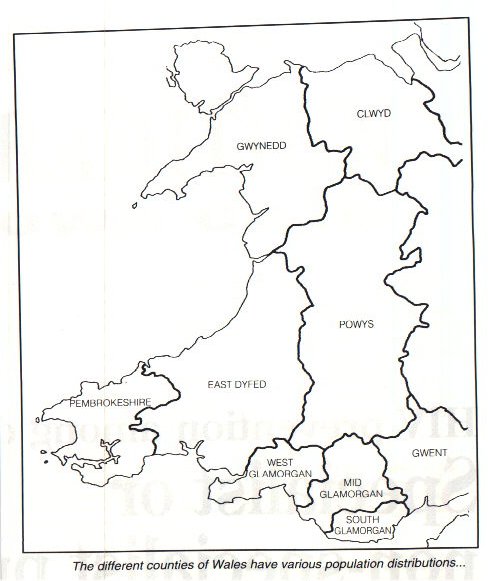
The different counties of Wales have various population distributions, with the majority of the population concentrated mainly in the industrial and mining towns in the valleys of South Wales. The more mountainous and rural areas of the North and West have sparse populations spread over large areas. The sparse population distribution of many parts of Wales has led to a concern for those drug users who do not live within easy reach of drug services/syringe exchanges.
This problem is compounded by the fact that many people who inject drugs do not see their drug use as a problem and are therefore unlikely to attend specialist drug services. Although drug services (as in England) are becoming more ‘user friendly’ - offering practical help and prescribing services together with a less rigid or judgemental approach - there are still many disincentives, such as the client’s distrust of service providers, ignorance of the services available and the inconvenience of travelling to specialist facilities. These last three factors are of particular relevance in many areas of Wales, particularly where syringe exchange services are based in one localised drug agency only (See Table 2).
Table 2: Specialist and non-specialist provision in Wales. Features of urban and rural services
| Urban | Rural |
| Focused IDU population | Dispersed IDU population |
| transport available | transport difficult |
| anonymous | less anonymity |
| resources focussed | resources dispersed |
| discreet | visible |
The local autonomy of drug and HIV prevention service providers in England is reflected in Wales and, therefore, services have developed differently in different areas largely depending on the attitudes and beliefs of those in the drugs and related fields. The general change in emphasis in the drugs field from traditional abstinence philosophies to ‘minimising the harm’ involved in the use of drugs, has occurred in the newer drug services in Wales, together with the established service in Cardiff. However, this is not the case in the North and to some extent the West of Wales, where abstinence philosophies traditionally prevailed in District Health Authorities and ‘no prescribing’ policies exist. Drug services in Wales have expanded and developed very quickly in the last five years. This was in some ways advantageous, as the newer services were often innovative in their policies and practices, and in some ways problematic as they had not had time to develop and consolidate services with the traditional, established services in the North and West of Wales.
The split ideologies in the approach to drug service provision in the North and West of Wales and that in the South, is reflected in the development of syringe exchanges in these areas. It is not surprising that the initial interest in syringe exchange came from those existing drug agencies which were previously working with a harm reduction model, the rationale of which advocated the type of health care response implicit within the concept of syringe exchange. As a consequence, syringe exchanges in the South were developed as adjuncts to established drug services and staffed by qualified nurses. In the North the situation was different, as the statutory drug (and alcohol) services in these areas worked with models of addiction less readily adaptable to the harm reduction approach implicit within an AIDS prevention strategy. HIV prevention services in these areas were not automatically integrated into the statutory drug services, but instead located in various centres in the community, developed as part of the AIDS counselling service (North East) and by community pharmacists (North West and Mid Wales).
It can be seen, therefore, that where a statutory drug service in Wales operated a ‘harm minimisation’ approach, service providers have taken the lead from England, developing one type of localised service offering help with drug problems together with both distribution and disposal of injecting equipment. In these areas, syringe exchange was actively supported and efforts were made to develop this within existing drug services (eg. Newport, Cardiff and Mid Glamorgan). In the South, therefore, services were provided quickly and efficiently. However, these services tended to be localised (81% of clients travelling five miles or less to attend), and therefore not used by clients outside this local ‘catchment area’. Community services in these areas have not yet been developed.
In the North, where the abstinence treatment philosophy is still prevalent and the population dispersed, syringe exchange was not supported or developed within existing drug service provision and, consequently, HIV prevention has developed independently. Instead, syringe exchange services were located in various centres in the community, by community pharmacists in the North West and by the HIV counselling services in the North East. These community-based services work primarily with a public health/ HIV prevention philosophy involving the dispersal and disposal of injecting equipment together with education and health care (See Table 3.)
Table 3: Features of "harm minimisation" and "abstinence" approaches to drug service provision
| Harm Minimisation | Abstinence |
| a choice of goals for clients | one goal only |
| unconditional help | help conditional on abstinence |
| prescribing services | no prescribing service |
| continued use acceptable | continued use not acceptable |
| easily integrates syringe | syringe exchange concept |
| exchange into philosophy | cannot be integrated into philosophy |
In this way, syringe exchange in the South was felt to be part of the professional territory of the statutory drug services, whereas in the North, syringe exchange was seen to be part of a public health response to the prevention of HIV and separated to some extent from the drug service provision. Staff based in schemes in the South state that one of the primary aims of the scheme is to attract users into their drug treatment service. This is not the case for staff in the North, who tend to see the prevention of HIV as more of an end in itself.
Future development
It has become clear that the prevention of HIV among drug users involves changing and improving specialist drug services. However, this is not enough, especially in rural areas where the distribution of the population undermines the effectiveness of localised specialist units. The possibilities of community based service provision involve sending outreach workers into the community and enabling community pharmacists and health service providers to take on an HIV prevention role. It may be more practical to see these services as having less ambitious aims, for example, restricting them to a public health role and their goal to the prevention of HIV.
It could be more efficient and effective to organise these three distinct aspects of HIV prevention - syringe dispersal, disposal and drug treatment - separately in rural areas.
Three elements of HIV prevention
Firstly, adequate syringe dispersal would ensure that drug users do not share infected syringes as a result of a lack of an easily available supply. Pharmacists could provide easy, anonymous access to affordable equipment, together with information. Other outlets could include GPs, Community Psychiatric Nurses, and other statutory and non-statutory drug services.
Second, to ensure that infected syringes are disposed of with no danger to either drug users and those close to them, or to the general public, it would be necessary to provide information regarding safe disposal along the lines of that given to diabetics (eg. burning, clipping and use of safe disposal containers). Easy access to disposal points could also be provided, which could be based in the premises of drug projects, pharmacists, Accident and Emergency Departments of hospitals, Health Centres and GPs’ surgeries. It may also be pragmatic to provide incentives to those people offering disposal points, and provide regular free removal of disposal containers.
‘Third, it is necessary to ensure that drug users are contacted in order to provide easy access to help with their drug and health problems, help in reducing the level of risk, and to give information, education, counselling. The dispersal and disposal points could be used as the means to advertise drug services and establish contacts between drug users and agencies.
Conclusion
Syringe exchange itself is based on a notion of providing injectors with clean equipment to prevent the spread of HIV among them (dispersal), together with the need to protect the general public, that is, a public health aim (disposal). These two aspects have traditionally been linked, and this system effectively creates and maintains contact between drug users and agencies, allowing the help and monitoring of users. Unfortunately, it may be this very help and monitoring that keeps some injecting drug users away from access to clean syringes. This study of services in Wales has indicated that the needs of injecting drug users in different areas are not adequately served due to the constraints of the response in each area.
For example, people living in rural areas of the Southern counties (where there is no community-based service) or some distance from the drug agencies, will not benefit from an agency-based response. Whereas the drug users in the North living near drugs agencies (where there is no agency-based syringe distribution provision), may well have benefited from an agency-based syringe exchange service.
Local autonomy concerning planning and management of services in Wales has led to a diversity of response. The consensus within influential local committees regarding certain issues within the drug treatment and HIV fields was sometimes in conflict with experience elsewhere. This has led to less conventional responses to the HIV problem in the North of Wales. It is possible that the community responses developed here, though slower to develop and more difficult to establish, may be less constrained in their future development than specialist services based in localised drug agencies.
This paper has considered the possibility of developing a community response to the prevention of HIV involving community pharmacists in the process of syringe dispersal and disposal. This is only one of a range of responses, from using volunteers and outreach workers to distribute syringes, to offering detailed information regarding safe disposal at home as for diabetics. HIV prevention among drug users has initially developed from an interest shown by those concerned with drug problems, that is those who work in drug agencies. Syringe exchange has therefore been initiated in, and developed as, an integral part of this drug service provision. Although many syringe exchange service users have not previously attended drug agencies, it is clear that these agencies are designed for, and have access to, people with ‘drug problems.’ They do not, however, cater for (and consequently do not attract) people who use drugs in a non-problematic way or do not think of themselves as having a ‘problem’. Many drug users are previously deterred from attending drug agencies for reasons of confidentiality, distrust of the helping professions and difficulties in travelling long distances (particularly in large areas with few localised services). These users would perhaps be less likely to use a syringe exchange service integrated with a drug agency service, than to take advantage of informal access to syringes in a local (or slightly more distant) pharmacy.
This work was carried out under contract with the Welsh Office and is published with their agreement.
Donoghoe, M., Stimson, G.V., Dolan, K. & Alidritt, L.1989 ‘Changes in HIV Risk Behaviour in Clients of Syringe Exchange Schemes in England and Scotland’ AIDS 3, 5, 267-272.
Glanz, A., Byrne, C. & Jackson, R 1990 Prevention ot AIDS Amongst Drug Users: The Role ot the High Street Pharmacist. London, Department of Health.
Lart, R. & Stimson, G.V.1990 National Survey of syringe exchange schemes in England. British Journal ot Addletlon 85,1433-1443.
Lart, R. & Stimson, G.V.1991 ‘ Not Just a Syringe
Exchange’ - A Study of the Organisation, working
practices and philosophy of three syringe
exchanges in England. Unpublished paper
Stimson, G.V., Alidritt, L., Dolan, K., & Donoghoe, M .C .1988. Syringe Exchange Schemes for Drug Users in England and Scotland. British Medical Journal 296, 1717-1719.
Stimson, G.V., Alidritt, L., Dolan, K., Donoghoe, M.C. & Lart, R. 1988. Injecting Equipment Exchange Schemes tor Drug Users in England and Scotland - Final Report University of London, Goldsmiths College.












