| Articles - Education and Prevention |
Drug Abuse
"UP YOUR BUM"
A SIMPLE, SAFER ROUTE OF DRUG TAKING OR A SQUIRT TOO FAR?
Presenter/Author: Matthew Southwell - General Manager, East London and City Drug Services.
1. Introduction:
This paper presents and reviews an adapted model of drug taking which offers a further alternative to injecting. The paper also describes the community development process and results of consultation that were applied in working up this option. It builds on the work of the Healthy Options Team in promoting chasing as a safer alternative to injecting. 1 "Up Your Bum" (UYB) is presented as a parallel alternative to injecting set within a wider framework of harm reduction and Hepatitis C (HCV) prevention work with injecting drug users.
2. Background:
During the 1996 Rankin Lecture, Dr Alex Wodak proposed a vision of drug services where the promotion of non-injecting routes of administration would become a key response to HCV. 2 While others had previously highlighted chasing as a potential harm reduction strategy s such an exclusive emphasis on drugs transitions provoked strong debate. Some user groups feared that such an approach would demonise injecting and that abstinence was a hidden sub-text to work on drug transitions. a This both highlighted the strength of attachment to injecting, particularly within the Australian context, and emphasised the need to carefully reflect on the marketing of messages around drugs transitions. The recognition of these factors underpins the approach to drugs transitions work in east London which promotes non-injecting routes as one of a range of options (with priority given to safer injecting practice) each of which are recognised as having different strengths and weaknesses. s
Having presented the Healthy Options Team"s pilot Chasing Campaign at the 7th International Conference on the Reduction of Drug Related Harm a constructive debate was entered into with the Australian IV League. While Healthy Options Team had not presented chasing as a universal panacea, the discussions about the Chasing Campaign inevitably were informed by the recent Rankin Lecture. The limitations of chasing as a comprehensive alternative to injecting were clearly identified during this debate. While this has not prevented the positive development of the Heroin Chasing Campaign as a joint initiative between the HOT and the Respect Users Union, it stimulated east London services to consider the potential opportunities of a wider focus to work on drugs transitions which has led in part to the development of "Up Your Bum." (UYB).
3. Weaknesses Identified With Chasing As Exclusive Focus For Drugs Transitions Work:
3.1 Chasing is only suitable for crack/cocaine, opium and some forms of heroin.
3.2 The technique of chasing takes a week on average to acquire and for some the skill is difficult to master, When drug users are reliant on the effectiveness on their route of administration to manage dependency adopting a new skill is an intimidating challenge. Whereas health professionals have been able to advise on injecting, chasing remains a skill which can be most effectively taught by those who have personally mastered the approach.
3.3 Among drug using communities with no history of smoking, chasing is an alien and totally unfamiliar technique. For example in Italy there is not an established peer group of heroin chasers who can act as a resource to injectors creating greater barriers, but not precluding, transitions to chasing.
3.4 Chasing may be impractical in some settings particularly for those new to the technique. It is important to note however, that experienced chasers can apply the technique in complex settings (ie: outdoors in the rain with the foil shielded by a baseball cap).
3.5 The promotion of transitions to chasing relies heavily on the high purity of street drugs. Spontaneous transitions to chasing in Europe and the USA were strongly influenced by rises in street purity levels. If purity was to fall it would be reasonable to assume that increased transitions to injecting would follow.
3.6 Injecting provides a "rush" that is not available with chasing.
3.7 There are times when users want to get as close to overdosing as possible. Drug users may be happy with chasing to promote control and stability for most of the time. At other times heroin users may wish to fully "gouch out" or "nod off" which may be better facilitated by injecting. It is important to emphasise that this is not necessarily a sign of abdicating control but reflects different individuals having different expectations about their drug use at different times.
4. Development of "Up Your Bum" as adapted route of drug taking:
In light of these weaknesses it was decided to attempt to identify a simple, multi-purpose route of drug taking which would offer a degree of "rush" without the risks of transmitting the blood borne viruses that were associated with injecting. It was also felt to be important to choose a technique which had a greater familiarity for injectors which reinforced and built upon existing skills.
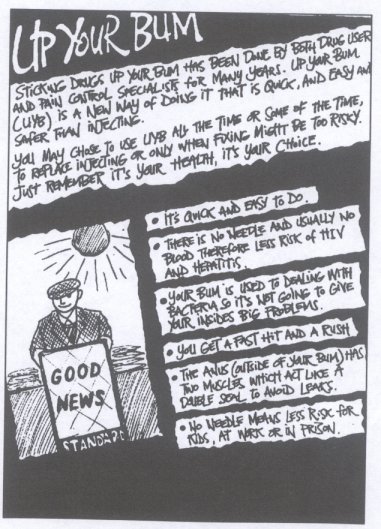
None of the existing practices of drug taking met this standard. Therefore, what has been proposed is a merger between two existing forms of illicit drug use with traditional models of palliative care. The result is a form of self-administered solution enema. The drugs are prepared as for injection, drawn up from the spoon into a barrel (without a needle), the barrel is then inserted through the anus and the liquid squirted into the bottom third of the rectum.
5. Development Process:
Having arrived at a basic concept, a three phase development strategy was agreed upon to explore, evaluate and test this technique before developing a formal harm reduction campaign. The development process was strongly informed by a community development process built on a dynamic working relationship with drug users during the concept development phase.
DEVELOPMENT PROCESS
Phase One:
Technique design - to identify whether the technique was practical and deliverable as harm reduction tool.
Exploratory discussions with key groups of drug; users.
Advice from those working in fields which had relevance to this project:
genitourinary medicine;
sexual health promotion around anal sex and sex toys;
palliative care specialists;
drugs field - both drug treatment and those involved in dance safety initiatives.
Cost benefit analysis undertaken. Decide whether to proceed to phase two.
Phase Two:
Finalise technique design.
Produce test materials:
test product with target audience;
test attraction to non-injectors;
test reaction of managers, policy makers and other professional stakeholders.
Collation of results
define specific target audience;
agree design protocol;
commission final harm reduction materials;
consider training issues;
agree marketing approach.
Phase Three:
Production of demonstration project:
-
formal focus groups;
-
staff training;
-
launch of demonstration project.
Note on user consultation:
During the development phase a number of groups of injectors were identified to play a peer support role to the project. 'These users were injectors of a diverse range of drugs and were of different genders, races and sexualities. They were a selected rather than a representative group. A group of clubbers were identified to test the products appeal among non-injectors. These were from the mixed gay men's dance scene (which was identified as being the group most likely to be attracted to UYB), all had long histories of recreational drug use and had practised a range of different methods of drug taking. All groups were asked not to pass on information about UYB during phases one and two and the non-injectors were asked not to disseminate the technique att all. Respect Users Union was seen as part of the professional consultation process.
6. Results Of Phase One:
Feed back to the initial exploratory phase can be divided into results from three discreet populations:
6.1 Clubbers/Non-injectors:
We did not identify substantial overt injecting on London club scene (and this was validated by discussions with a lesbian and gay dance safety initiative 6). However, among some sections there was more experimentation with less conventional routes of drug taking.
Drug users already inserted drugs anally:
* dabbing - inserting powdered drugs into the rectum on the finger;
* stuffing - inserting drugs in powdered form wrapped in cigarette paper into the rectum or ecstasy tablets pushed into the rectum.
However, this was mostly on the club scene, with stimulants and among recreational drug users. Some clubbers who had stuffed ecstasy reported that it had on occasions caused burning in the rectum. UYB was seen has highly attractive by clubbers particularly on the gay men's scene but by no means solely among gay men.
6.2 Injectors:
Older opiate users remembered suppositories which most had melted to extract drugs for injection. It was the slow release nature of the suppositories that was unattractive.
There was interest from injectors in the technique and its familiarity and ease of application were positively received. However, there was great concern about effectiveness. As UYB had no history within the injecting community, there were fears about risking ones drugs on an untried approach.
There was some stigma with the route most notably among heterosexual men. Women were more open to UYB and questioned whether the vagina might also be a possible alternative route of drug taking.
6.3 Professional Advice:
The anal route is seen as a positive option by pain control specialists particularly for slow release at night. However, there is limited research into this route and most drugs are not licensed specifically for anal use.
There were greater theoretical risks than had been expected involved with the sharing of barrels but the primary risks were associated with sharing rather than the technique itself (see Appendix A - Cost Benefit. Analysis). Damage to the rectum lining reported by ecstasy "stuffers" would probably be minimised through the drugs being used in solution form. Ecstasy is particularly known for its caustic effects.
Anxiety was expressed that an externally introduced technique could result in a new drug using epidemic similar to the 1970s growth of drug use following the dissemination of heroin chasing. It is important to note the arrival of a new type of heroin was a key part of this increase in drug taking. ' Therefore, there was a dual relationship between drug and technique.
The potential for UYB to have the effect of reducing the stigma towards injecting among non-injectors through acclimatising them to injecting equipment was discussed. Talking about and observing injecting has been shown to increase an individuals propensity to transfer to injecting. 8 However, this was not supported by the clubbing sample group themselves who remained hostile to injecting while intrigued by UYB.
7. Design Of Test Campaign
In light of this information the initial work sought to develop an approach that was attractive to injectors while seeking to minimise up take among non injectors. It was seen as desirable to promote UYB to injectors where it would have a harm minimisation effect while isolating clubbers from UYB where is might increase risks.
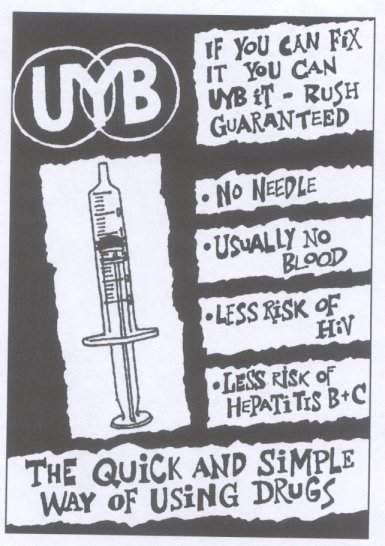
To test our ability to achieve these goals a sample product was produced. This used a fanzine style leaflet to create distance from glossy club flyers reinforced by the use injecting street language. It was also decided to use a logo which avoided naming the technique. This was to achieve two goals:
* to avoid building resistance among injectors before they had opened and begun to read the leaflet;
* to reduce attraction to gay clubbers.
Further its was agreed to give high prominence to the image of a syringe barrel on the front cover of the leaflet/poster to attract injectors and "turn off" clubbers.
The leaflet text avoids giving advice on preparing the drug for injection or UYB, placing another obstacle in the road of non-injectors while recognising that injectors will already have this knowledge.
8. Results Of Consultation On Test Campaign:
8.1 Injectors:
Process:
A rough mock up of the front cover and one page of the leaflet was developed (see Appendix B) with a draft text of the leaflet. These were shown to the injectors peer support groups and also to injectors not previously involved in the project through open but structured focus sessions which covered fifteen people either in a group or individual setting. 9 These were run alongside the Healthy Options Team needle exchange.
Results:
Injectors would discuss and try the technique when they were introduced to it alone. In groups, injectors quickly developed group resistance to the idea an experience which had more in common with work around sexual health than drug use. Women were less resistant to the campaign than men and readily accepted messages about the dangers of vaginal use. Heterosexual men reacted very differently to gay men and women. One example was their common refusal to discuss sharing of barrels in UYB as the thought was too distasteful (although this stigma was valued as preventing sharing among this group).
The use of cautious health promotion language ("usually no blood") was confusing and distracted people from the message the UYB would without sharing avoid blood borne viruses.
UYB was identified as having value for injectors when their syringes became clogged when veins collapsed in the middle of injecting.
8.2 Clubbers/Non-injectors:
Process:
The materials were shown to the peer support group of clubbers. However, this group was already aware of the technique and had seen earlier more positive presentations of the technique. The predisposition of the peer support group of non-injectors was in favour of the technique thus promoting greater interest in the harm reduction materials than might be expected with non-injectors coming fresh to the leaflet. It was decided not to sample a new group of non-injectors due to anxiety about information on the technique reaching outside the target population.
Results:
While the barrel had some effect in reducing attraction to non-injectors, the highlighting of the benefits on the front cover was attractive (ie: rush guaranteed). The potential potency of UYB among clubbers, particularly on the gay men's scene, was reinforced. Potential for mixing with anal sex was seen as a possibility.
8.3 Professionals:
Process:
These images were used to test the reaction of policy makers, drugs workers, the police and managers through joint planning structures and the management framework of our parent organisation.
Results:
The reactions were very strong to the campaign including shock and horror ("This is just distasteful! ") and a belief that harm reduction should have limits (eg: from the ex-manager of a needle exchange: "If people have got to the point of needing this type of intervention then they should really be told to stop! "). Others thought the whole process was very amusing.
There was also a legitimate concern that the campaign contained positive messages about drug use which if fell into the hands of school children could become misdirected. Therefore, there was strong agreement that the campaign to be targeted carefully and an argument was put forward that UYB should not to be supported by fully fledged marketing campaign. This considered both actual risk but also concerns about a sensational response from the media and/or politicians.
From those involved in work on drugs transitions there were concerns about the impact of negative publicity of UYB on other work on drugs transitions.
It is also important to note that alongside some of these reactions were those who felt the campaign was exciting, valuable, and well thought through. This group tended to stress the importance of the work including a clear programme for the management of risk to ensure the project achieved its potential.
Respect Users Union remained strongly committed to the approach and lobbied for it to be made more publicly available. Other users groups expressed strong interest.
9. Design Of Final Campaign:
9.1 Revised design specification:
In light of this testing is was decided that generally the leaflet text was appropriate. Most significantly it was decided to refocus the imaging and marketing of the campaign:
there would be a clear separation from other drugs transitions campaigns;
the value of reaching each individual (particularly heterosexual men) away from peer pressure was recognised;
given the negative association between UYB and anal sex among heterosexual male injectors it was decided to make closer linkage between UYB and injecting in groin given the acceptance that use of this site for injecting had no sexual connotations;
it was decided to abandon the idea of a general supporting poster for the campaign in demonstration phase.
(see Appendix C - Images from demonstration project).
9.2 Marketing Approach:
To reinforce the design specification a clear marketing approach was formulated:
10. Conclusion:
The project has now reached the end of phase two and a formal demonstration project is now being finalised. Following a series of formal focus groups with those not involved in the development of the project to date, the campaign will be subject to an ethical review process facilitated within the framework of Tower Hamlets Healthcare NHS Trust. From work to date it is possible to draw a number of conclusions:
1. UYB is a positive option for injectors that makes anal use an accessible route of administration;
2. there are both risks and benefits associated with the technique although negative factors can be reduced through careful design and marketing;
3. drug users should be made aware of both pros and cons of UYB to promote informed choice.
4. individualised and narrow cast advertising approaches are most appropriate to this technique;
5. traditional broad based health promotion technique are likely carry substantial risks of passing messages to those other than the target population;
6. UYB balances many of the short comings of the chasing campaign but it carries with it a different set of obstacles and stigmas;
7. it is recommended to take a cautious approach to the dissemination of UYB as campaigns can be widened at a later date whereas ground is likely to be hard to recover if UYB becomes widely publicised.
REFERENCES:
1. Southwell, M. and Jankowska, T. Promoting heroin and crack/cocaine chasing as harm reduction tools in the late 1990s 7th International Conference on the Reduction of Drug Related Harm (1996).
2. Wodak, A. Rankin Lecture - 7th International Conference on the Reduction of Drug Related Harm (1996).
3. Strang, J., Des Jarlais, D., Griffiths, P., Gossop, M. The study of transitions in the route of drug use: the route from one route to another. British Journal of Addiction Vol 87 (1992).
4. Wood, C. Demonising the needle - Connections (1996).
5. Southwell, M. and Kennedy, D. From theory to practice: Developing a harm reduction strategy in response to Hepatitis C - Drug News (1997).
6. Vatry, I. and Baker, K. Personal correspondence with Project LSD (1996).
7. Griffiths, P., Gossop, M., Strang, J. Chasing the dragon: The development of heroin smoking in the United Kingdom - unpublished (1996).
8. Hunt, N. and Stillwell, G. A brief intervention to prevent initiation into injecting - 8th International Conference on the Reduction of Drug Related Harm (1997).
9. Haywood, J. Feedback from HOT focus groups - correspondence (1997)
Appendix A COST/BENEFIT ANALYSIS
| BENEFITS | COSTS |
| 1. Suitable for most power or pill form drugs 2. Simple to acquire 3. Familiar to injectors 4. Offers degree of "rush" 5. Quick absorption 6. Role of rectum as filter 7. Dramatically reduced risks transmission of blood borne viruses (even with sharing) 8. Not affected by Paraphernalia Laws 9. Reduced community safety risks 10. Reduced irritation for those "stuffing" drugs with caustic effect 11. Stigma attached to sharing among some populations |
1. Potential trauma to rectum lining 2. No reduced overdose risk 3. Laxative effect of repeated use in one session (i.e stimulants) 4. Theoretical risk of transmission of blood borne viruses if trauma exists and sharing takes place 5. Other risks present if sharing takes place (i.e hepatitis A, salmonella, genital warts etc.) 6. Acclimatise non-injectors to injecting equipment 7. Bring new dynamic into drug taking 8. Ethics of introducing "new" technique |