Chronic 3,4-Methylenedioxymethamphetamine (MDMA) Use: Effects on Mood and Neuropsychological Function?
Drug Abuse
AM. J. DRUG ALCOHOL ABUSE, 18(3), pp. 331-341 (1992)
Chronic 3,4-Methylenedioxymethamphetamine (MDMA) Use: Effects on Mood and Neuropsychological Function?
John H. Krystal,* M.D.
Psychiatry ServiceYale University School of Medicine
West Haven VA Medical Center
950 Campbell Avenue, West Haven, Connecticut 06516
Clinical Neuroscience Research Unit
Department of Psychiatry
Yale University School of Medicine
Connecticut Mental Health Center
34 Park Streqt, New Haven, Connecticut 06508
Lawrence H. Price, M.D.
Clinical Aleuroscience Research Unit
Department of Psychiatry
Yale University School of Medicine
Connecticut Mental Health Center
34 Park Street, New Haven, Connecticut 06508
Charles Opsahl, Ph.D.
Psychiatry Service
Yale-New Haven Hospital
Department of Psychiatry and Psychology
Yale University School of Medicine
New Haven, Connecticut
George A. Ricaurte, M.D., Ph.D.
Department of Neurology
Johns Hopkins Medical Institution
4940 Eastern Avenue, Baltimore, Maryland
George R. Heninger, M.D.
Clinical Neuroscience Research Unit
Department of Psychiatry
Yale University School of Medicine
Connecticut Mental Health Center
34 Park Street, New Haven, Connecticut 06508
*To whom requests for reprints should be addressed at Psychiatry service, Yale University School of Medicine, West Haven VA Medical Center, 950 Campbell Avenue, West Haven, Connecticut 06516. Telephone: (203) 932-5711, X2524, 4481.
ABSTRACT
3,4-Methylenedioxymediamphetamine (MDMA; "ecstasy") is a selective serotonin (5-HT) neurotoxin in animals. There is now preliminary evidence in humans of 5-HT deficits associated with extensive use of MDMA. In order to begin to describe the cognitive and mood effects of chronic MDMA use, nine individuals with extensive MDMA use histories were studied. Despite of the absence of memory deficits on clinical examination, a pattern of mild-to-moderate impairment was observed on both the Initial and Delayed Paragraph Tests of the Wechsler Memory Scale; eight of the subjects had at least mild impairment on at least one test in the neuropsychological battery. Despite previously reported suggestive evidence of 5-HT deficit in this group, none reported depressed mood or met clinical criteria for an affective disorder at the time of testing. These preliminary findings raise concern about possible detrimental effects of MDMA use on neuropsychological function for future systematic study and they highlight important issues regarding the effects of 5-11T deficits on cognitive function and mood regulation.
Key Words: Serotonin; 5-Hydroxytryptaniine (5-HT); MDMA; Neurotoxin; Wechsler Memory Scale; dro%
Drug abuse; Attention; Memory; Depression
INTRODUCTION
The ring-substituted amphetamine derivative 3,4-methylenedioxymethmphetamine (MDMA; "ecstasy") was first introduced in 1914 and patented as an appetite suppressant [11. MDMA has been reported useful as an adjunct to psychotherapy through facilitating interpersonal communication, enhancing insight, increasing self-esteem, and decreasing the abuse of other illicit substances [21. MDMA has also been used as a recreational psychoactive agent, and concern over its increasing popularity led to its classification as a Schedule 1 agent by the Drug Enforcement Agency in July 1985 [31. Despite legal sanctions, recreational use of MDMA has been increasingly visible: one survey found that 40% of the undergraduates polled at a major university had used MDMA at least once [41. The increased frequency of MDMA use has, in turn, raised questions about medical and psychiatric complications of acute and chronic MDMA use [51.
Subjective reports of acute effects indicate that after ingesting MDMA, one generally experiences a 4-to-8 hour pefiod of peak drug effect associated with feelings of increased closeness to people, euphoria, heightened arousal, selfconfidence, increased sensory sensitivity, a feeling of openness to new ideas, increased depth of emotion, and decreased appetite [6, 71. MDMA is reported to both increase the capacity to focus thought and to cause difficulty in concentrating and racing thoughts. Downing [61 reported that MDMA, at a mean oral dose of 0.52 mg/kg, did not acutely affect short-term memory or digit repetition although there was evidence of judgment impairment in 4110 subjects. Visual blurring, illusions, or infrequently, vipal hallucinations may also occur in association with MDMA administration. Other common MDMA effects include symptoms of sympathetic arousal (e.g., tachycardia, tremor, palpitations, dry mouth, and diaphoresis), trismus, and bruxism. The acute effects of MDMA can be prolonged by taking an additional dose of the drug or enhanced by coadministration of the 5-HT precursor, tryptophan (Subject C, this study). However, if too much additional MDMA is consumed in a single session, individuals report unpleasant symptoms of autonomic hyperarousal associated with feelings of restlessness and anxiety. Following the acute subjective effects of MDMA, users report a 24-48 hour period characterized by the persistence of acute MDMA effects and the onset f additional symptoms suggestive of the "crash" after psychostimulant administration. Thus, Peroutka and his colleagues [71 found that the most common symptoms in his sample of 100 recreational MDMA users were: drowsiness (36%), muscle aches or fatiguability (32%), lingering sense of closeness (22 %), depression (21 %), tight jaw muscles (21 %), difficulty concentrating (21%), and headache (17%).
It is now well-established that MDMA has at least transient neurotoxic effects on serotonergic (5-HT) neurons. Loss of the fine 5-HT terminals is associated with decreased levels of 5-HT and/or its metabolite 5-hydroxyindolacetic acid (5-HIAA) in several brain regions and in cerebrospinal fluid [8, 91. 5-HT neurotoxicity associated with MDMA use has also been described in humans. We have previously reported that a group of nine individuals with extensive MDMA use histories showed evidence of a blunted prolactin response to trytophan administration [101. Cerebrospinal fluid levels of 5-HIAA were normal in a small sample of MDMA users in one study [111 but were found to be 25 % lower than a comparison group of low back pain patients in another study with a larger sample size [121.
Despite concern that the 5-HT toxicity associated with MDMA use might have significant behavioral sequelae, to our knowledge there have been no reports about the long-term neuron&yghglogical consgg aences of MDMA use and few reports about long-term subjective effects. In order to begin to address these questions, we evaluated mood and neuropsychological function in nine individuals with extensive MDMA use histories. Suggestive evidence for 5-HT deficits in this group of MDMA users was previously reported [101.
SUBJECTS AND METHODS
Subjects were recruited nationally and tested in the outpatient facilities of the Clinical Neuroscience Research Unit, New Haven, Connecticut. Nine subjects (seven male, two female; mean ± SD, age, 34 ± 7 years; age range, 22-47 years) with a durrent or recent history of substantial MDMA use participated in this study. They had used what they believed to be MDMA for a mean of 5.1 ± 2.3 years (range, 2-7 years) at a rate of 1.9 ± 1.7 times per month (range, 0.33-5.0 times/month). The average usual dose of MDMA used was 135 ± 44 ing ( nge, 50-200 nig), corresponding to a mean dose of 1.8 mg/kg (range, 1. 1-2.3 mglkg). Many subjects reported the occasional use of much higher doses (up to 500 ing or 6 mglkg). The mean cumulative total dose of MDMA was estimated at 13.3 _± 3.4 range, 23-44.2 g). Prior to testing, the last reported use of MDMA was 66 ± 50 days (range, 20-180 days). Subjects were requested to abstain from psychoactive drugs for at least 3 weeks prior to testing. Three of the MDMA users did report inflequent marijuana use during the 3-week period before testing.
MDMA was the primary drug of choice for the subjects participating in this study, although they had also used other substances for recreational purposes. Data were collected on previous substance use in 8 of 9 subjects. Six of the eight subjects (#1-4, 6, 8, 9) reported at least experimentation with all of the following substances: alcohol, amphetamine, cocaine, and marijuana. Five of the eight subjects had used LSD (#1-3, 7, 9); 218 subjects used DMT (#3, 7), phencyclidine (#3, 7), or psilocybin (#1, 3); and one subject (#3) reported self-administration of a number of additional substances including harmaline, mescaline, ketamine, 5-methoxy-DMT, and ibogaine.
Neuropsychological and behavioral assessment was coordinated with a tryptophan infusion procedure described in detail elsewhere (10). Patients completed their neuropsychological testing beginning at least 3 hours after the intravenous infusion of 7 g of tryptophan. By this time neuroendocrine and behaviral measures indicated a return to baseline. A battery of neuropsychological tests was administered by a psychologist (C.O.), and an extensive clinical assessment and substance abuse history was obtained by research psychiatrists (J.H.K., L.H.P.).
Neuropsychological instruments included the revised version of the Wechsler Adult Intelligence Scale (WAIS-R), the paragraph and figural recall sections of the Wechsler Memory Scale [131, the Boston Naming Test, the multiple choice form of the Benton Visual Retention Test (revised), the Tokens Test, the Trail Making Test, the Tactual Performance Test, the Finger Oscillation Test, the Lafayette Pegboard Test, and a test of Grip Strength. Normative values applied to the data in this study were published by Russell et al. [141 and Russell [131. Scores were labled "mildly impaired" or "moderately impaired" if they fell one or two standard deviations below age-matched normative values, respectively. The Beek Depression Inventory [151 and an extended version of the Hamilton Depression Scale 116] were also administered to assess mood.
RESULTS
Subjective and Historical Reports
None of the subjects reported current anxiety or affective symptoms nor did they meet DSM-111-R (171 criteria for a current Axis I clinical syndrome. The low rate of current symptoms contrasted with a high prevalence of pre-MDMA psychiatric symptoms. Seven of the nine subjects reported periods in their life when anxiety or depression was a problem, and previous DSM-111-R diagnoses are listed in Table 1. Also, six subjects had family histories of alcohol or other substance abuse, three subjects had family histories of affective disorder, and one subject had a family history of generalized anxiety disorder (Table 1).
Neuropsychological and Clinical Findings
Mental status examinations conducted as part of the screening process did not reveal any clinical impairments in cognitive function, nor did neurological examinations reveal any focal neurologic deficits. Selected formal assessments of neuropsychological function are presented in Table 2. This group displayed a high level of cognitive ftmction, as reflected in the mean full scale IQ of 115 ± 9.5 and the absence of a difference in verbal and performance IQ. With the exception of performance on the Wechsler Memory Scales, there were no clear group patterns of impairment. On the Trail Making A Test, one subject (#4) showed mild (45 s for completion) ar;d one (#5) showed moderate (59 s) impairment. On the Tactual Performance Tests, one subject (#3) showed mild impairment (8 min and 44 s) in dominant hand function, two subjects (#3, 4) exhibited mild impairment (4 min and 50 s, 6 min and 4 s, respectively) in nondominant hand function, and one subject (#2) had mild impairment (2 min and 55 s) on the test for both hands. Two subjects (#5, 6) showed mild impairment (scores of 4 and 3, respectively) in their performance of the location component of the Tactual Performance Test. Subject #1 exhibited a mild degree of impairment (76 s) on the Lafayette Pegboard Test for nondominant hand function.
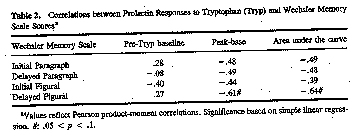
Performance on the Russell (1975) adaption of the Wechsler Memory Scale (WMS) was subtly impaired in several subjects (Table 1). Five of the nine subjects showed at least mild impairment on the WMS-Initial Paragraph Test compared to established normative values. Four of these five subjects also showed deficits on the WMS-Delay Paragraph Test, and three of the five subjects showed evidence of mild impairment on the WMS-Delay Paragraph Test. None of the Wechsler Memory Scale scores correlated significantly with the cumulative dose (in grams or mg/kg) of MDMA ingested. Also, neither the baseline prolactin level nor the prolactin response to tryptophan infusion correlated significantly with performance on the WMS-Initial Paragraph or WMSDelayed Paragraph tests, the subscales most frequently indicating impairment (Table 2). However, there was a trend toward significance in the correlation between the prolactin response to tryptophan and performance on the WMS-Delayed Figural Test (Table 2).
With the exception of Subject #8, all subjects had at least mild impairment on at least one test of neuropsychological function. However. none of the MDMA users showed evidence of current affecfive or anxiety disorder based, on clinical examinatim Also. none of the subjects exceeded a score of 5 on the Hamilton Depression Scale or 6 on the Beck Depression Inventory (Table 1).
DISCUSSION
These preliminary data raise the possibility that individuals with extensive MDMA use histories exhibit mild subclinical impairments in cognitive function but not affective disorder. Subjects in this study exhibited impairment on WMS subscales that may indicate memory or attentional deficits that were not evident on clinical examination. No other cognitive deficits were consistently observed in these subjects. Given the number of tests administered, deviations from normative values might be expected on the basis of chance alone. Thus, tests where one or two subjects exhibited deficits compared to normative samples must be considered particudarly suspect.
The prolactin response to tryptophan showed a trend toward inverse correlation with scores on the Delayed Figural Test of the WMS, suggesting that tryptophan impaired performance on this test. Performance on the figural test may have been particularly vulnerable to disruption by tryptophan, perhaps analogous to the denervation supersensitivity observed after the administration of 5-HT neurotoxins to animals [18, 191. In contrast, there were no significant correlations between prolactin response to tryptophan and performance on the Paragraph Tests of the WMS, the tests where most subjects exhibited impairment, suggesting that these impairments are not related to the effects of tryptophan infusion.
Deficits in 5-HT function caused my MDMA may have contributed to the attention or memory impairments detected in these subjects. Four subjects exhibited mild or moderate impairment on the WMS-Initial Paragraph Tests, five subjects exhibited mild-to-moderate impairment on the WMS-Delay Paragraph Test, and three subjects showed mild impairment in the WMS-Delay Figural Test. Little is known about 5-HT modulation of memory function in humans (reviewed in Ref. 20), however, 5-HT innervation of brain regions involved in memory, such as as the hippocampus, and cerebral cortex appear to be affected by MDMA in
animals and primates [8, 91.
The neuropsychological findings reported here must be interpreted with caution. The comparison of patients to age-matched normative"data rather than a comparable group of healthy subjects under identical experimental conditions limits the degree of assuredness with which one can derive conclusions from these data. Also, subjects completed their psychological testing following tryptophan infusion. Although behavioral and neuroendocrine measures had returned to baseline at the time of testing, it is still possible that the tryptophan infusions contributed to memory deficits observed in this study. Concern regarding potential tryptophan effects on memory function in this study is reduced by two observations: 1) Performance on the paragraph subscales of the WMS did not correlate with the prolactin response to tryptophan (Table 2), and 2) the neuroendocrine study suggested that these subjects were less responsive to tryptophan than healthy comparison subjects. Also, Winokur and his associates (21] did not find evidence of neuropsychological effects of a 7.5-g tryptophan infusion in healthy subjects at 115 min post-infusion, a shorter period between infusion and assessment than in the current study. This group concluded that tryptophan impaired the ability to sustain a high level of motor activity while sparing cognitive function.
Another limitation of these data is that subjects had used other psychoactive substances which may have had effects on neuropsychological function. Alcoholism is clearly associated with memory impairment. None of the subjects in this study met DSM-IH-R criteria for alcobol abuse or dependence in the previous year. However, 5-HT selective antidei)ressants reduce the detrimental effects of alcohol consumption on memory function, suggesting that alcohol abusers might be particularly sensitive to 5-HT neurotoxic effects [22]. Chronic LSD ingestion is also associated with cognitive impairment, although in a different pattern than was observed in the MDMA users [23, 241. Impaired performance on the WMS has also been reported in poly-substance abusers [251, although it is unclear which agents were responsible for memory impairment in this study.
The absence of clinical depression or depressed mood in these subjects suggests that decreases in 5-HT function may be necessary but not sufficient causes of depression. Several lines of evidence implicate decreased 5-HT function in depressed mood or major affective disorder: 1) Lowering of brain serotonin levels by tryptophan depletion or by the administration of parachlorophenylalanine has been reported to elicit depressed mood in healthy subjects and antidepressantremitted depressed patients; 2) the CSF levels of 5-HL4,A have been reported to be lower in depressed patients compared to healthy controls in some, but not all, studies; and 3) the prolactin response to tryptophan appears to be blunted in depressed patients and enhanced in these patients by antidepressant treatment (reviewed in Ref. 26). The MDMA users in this study showed evidence of blunting of their prolactin response to tryptophan, and the group studied by Ricaurte et al. [121 showed evidence of decreased CSF 5-HIAA. However, even though some of the MDMA users had 5-HT deficits, previous symptoms of depression, and/or a family history of affective disturbance, none of the MDMA users were depressed at the time of testing. The absence of depression in the MDMA users may be due to differences in the 5-HT dysregulation produce' by MDMA and that occurring in major affective disorder.
These preliminary data are of interest because they raise issues concerning the neuropsychological consequences of long-term MDMA use and the relationships between 5-HT systems, mood regulation, and memory function. The methodologic limitations of this study highlight the need for larger scale and prospective studies of the effects of MDMA use to further evaluate the clinical and scientific findings reported here.
ACKNOWLEDGMENTS
This study was supported in part by Grants MH-00579, MH-36229, MH25642, and DA-04060 from the U.S. Public Health Service, Washington, D.C.; by the Multidisciplinary Association for Psychedqlic Studies, Sarasota, Florida; and by the state of Connecticut. Additional partial support came froln the Department of Veterans Affairs. Daniel X. Freedman, M.D., was instrumental in facilitating the collaboration leading to this research. The clinical and research staff of the Abraham Ribicoff Research Facilities, New Haven, Connecticut, provided assistance.
REFERENCES
(1] Merck, E., Vefahren z ur darsteehmg von aRylozyaryl-dialyloxyaryl- und aLkylenedioxyarylarrunopropanen bzw. deren am sfickstoff monoaRylierren derivaten, German Patent 294,350 (1914).
[2] Greer, G., and Tolbert, R., Subjective reports of the effects of MDMA in a clinical setting, J. Psychoactive Drugs 18:319-328 (1986).
(3] Lawn, J. C., Schedules of controlled substances; temporary placement of 3,4-methylenedioxymethadmphetamine (MDMA) into Schedule 1, Fed. R egist. 50:23118-23120 (1985).
[41 Peroutka, S., Incidence of recreational use of 3,4-methylenedimethoxymetharnphetaniine (MDMA, "ecstasy") on an undergraduate campus, New EngL J. Med 317:1542-1543 (1987).
[51 Dowling, G. P., McDonough, E. T., and Bost, R. 0., 'Eve' and 'ecstasy.' A report of five deaths associated with the use of MDEA and MDMA, JAMA 257:1615-1617 (1987).
[6] Downing, J., The psychological and physiological effects of MDMA on normal volunteers, J. Psychoactive Drugs 18:335-340 (1986).
[7] Peroutka, S. J., Newman, H., and Harris, H., Subjective effects of 3,4-methylenedioxy methamphetamine in recreational users, Neuropsychopharmacology 1:283-287 (1988).
[8] Ricaurte, G. A., Forno, L. S., Wilson, M. A., DeLanney, L. E., Irwin, I., Molliver, M. E., and Langston, J. W., (±)3,4-Methylenedioxymcdiamphetamine selective damages central serotonergic: neurons in nonhuman primates, JAMA 260:51-55 (1988).
[9) Wilson, M. A., Ricraute, G. A., and Molliver, M. E., Distinct morphologic classes of scrotonergic axons; in primates exhibit differential vulnerability to the psychotropic drug 3,4-methylenedioxymethamphetamine, Neuroscience 28:121-137 (1989).
[10) Price, L. H., Ricaurte, G. A., Krystal, J. H., and Heninger, G. R., Neuroendocrine and mood responses to intravenotis Ltryptophan in 3,4-methylenedioxymethamphetamine (MDMA) users, Arch. Gen. Psychiatry 46:20-22 (1989).
[11 Peroutka, S. J., Pascoe, N., and Faull, K. F., Monoamine metabolites in the cerebrospinal fluid of recreational users of 3,4methylenedioxymediamphetamine (MDMA; "Ecstasy"). Res. Commun. Substance Abuse 8:125-138 (1987).
[12 Ricaurte, G. A., Finnegan, K. T., DeLanney, L. E., Irwin, L, and Langston, J. W., Aminergic metabolites in cerebrospinal fluid of humans previously exposed to MDMA: Preliminary obscrvations, Ann. N. Y. Acad. Sci. 600:699-710 (1990).
[13 Russell, E. W., A multiple scoring method for the assessment of complex memory functions, J. Consult. Clin. Psychol. 43:800809 (1975).
[14 Russell, E. W., Neuringer, C., and Goldstein, G., Assessment of Brain Damage: A Neuropsychological Key Approach, WileyInterscience, New York, 1970, pp. 107-109.
15 Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J., An inventory for measuring depression, Arch. Gen. Psychiatry 4:561-571 (1961).
[16 Mazure, C., Nelson, J. C., and Price, L. H., Reliability and validity of the symptoms of major depressive illness, Arch. Gen. Psychiatry 43:451-456 (1986).
[17 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. revised. American Psychiatric Association, Washington, D.C., 1987. 1~
[181 Nelson, D. L., Herbet, A., Bourgoin, S., Glowinski, J., and Hamon, M., Characteristics of central 5-HT receptors and their adaptive changes following intracerebral 5,7-dihydroxytryptarrune administration in the rat, Mot. Pharmacol. 14:983-995 (1978).
(191 Trulson, M. E., Eubanks, E. E., and Jacobs, B. L., Behavioral evidence for supersensitivity following destruction of central serotonergic nerve terminals by 5,7-dihydroxytryptamine, J. Pharmacal. Exp. 77ter. 198:23-32 (1976).
[201 Wolkowitz, 0. M., Tinklenberg, J. R., and Weingartner, H., A psychopharmacological e p rs ec- 10 sptive of cognitive functions: IL Specific pharmacologic agents, Neuropsychobiology 14:133-156 (1985).
[211 Winokur, A., Lindberg, N. D., Lucki, L, Phillips, J., and Amsterdam, J. D., Hormonal and behavioral effects associated with intravenous L-tryptophan administration, Psychopharmacology 88:213-219 (1986).
[221 Weingartner, H., Rudorfer, M. V., Buchsbaum, M. S., and Linnoila, M., Effects of serotonin on memory impairments produced by ethanol, Science 221:472-474 (1983).
[231 McGlothlin, W. H., Arnold, D. 0., and Freedman, D. X., Organicity measures following repeated LSD ingestion, Arch. Gen. Psychiatry 21:704-709 (1969).
[241 Wright, M., and Hogan, T. P., Repeated LSD ingestion and performance on neuropsychological tests, J. Nerv. Ment. Dis. 154:432-438 (1972).
[25] Sweeney, J. A., Meisel, L., Walsh, V. L., and Castrovinci, D., Assessment of cognitive functioning in poly-substance abusers, J. Clin. Psychol. 45:346-351 (1989).
[261 Price, L. H., Chamey, D. S., Delgado, P. L., Goodman, W. K., Krystal, J. H., Woods, S. W., and Hettinger, G. R., Clinical data on the role of serotonin in the mechanism(s) of action of antidepressant drugs, J. Clin. Psychiatry 51(4, Suppi.):44-50 (1990).
Last Updated (Monday, 20 December 2010 19:33)












