Section1: The history of injecting and needle exchange
Drug Abuse
Section1: The history of injecting and needle exchange
Introduction
Development and use of the hypodermic needle and syringe
Injecting and drug dependence
Injecting in the 20th century
The 'Edinburgh experience'
The development of UK service provision
Current UK service provision
Current worldwide service provision
International harm reduction movements
Key events in the development of injecting drug use
Key points
Introduction
The risks of HIV and hepatitis infection to injecting drug users are present throughout the world. However, the services that exist to prevent infection amongst injecting drug users vary widely from country to country.
Starting with the development of the hypodermic syringe and injecting as a mode of drug administration, this section provides an historical perspective to responses to the injection of illicit drugs.
The way that injecting grew as a method for administering drugs is charted, with a description of how, when and why needle exchange services in the UK were developed.
Current service provision in the UK is then described and placed in a global context with descriptions of the position in the USA, Australia, European countries and Asia. This section is intended to give the UK reader an overview of the response in other countries and regions.
Development and use of the hypodermic needle and syringe
It is impossible to be precise about when injecting as we know it began. Clearly weapons such as blowpipes and poison-tipped darts were in use thousands of years ago to introduce substances into the body.
Intravenous injection was recorded as early as the 17th century.
Subcutaneous injecting did not begin until the mid to late 19th century, probably as an extension of the then new practice of inoculation against disease.
The invention of the syringe
Various people have been credited with the invention of the syringe including :
![]() Christopher Wren
Christopher Wren
![]() Robert Boyle1
Robert Boyle1
![]() Pascal2
Pascal2
![]() De Graaf3.
De Graaf3.
It is therefore difficult to establish that any one person was completely responsible and of what, in the context of these claims, a 'syringe' consisted: at its most basic it was a type of simple pump.The truth is probably that syringe-type devices were invented by many different people and then adapted by others.
Wren is the first person recorded to have employed intravenous injecting in Britain. In 1656 he experimented by injecting dogs with opium and other substances4. Wren's 'syringe' was a crude device, consisting of a quill attached to a small bladder and was known as a clyster (Figure 1.1). An incision in the skin had to be made in order to gain access to the vein. (Crude injecting devices still persist today; many self injectors do not have access to modern sterile equipment and manufacture their own from what is available. In the UK this is most likely to occur in prisons.)
Wren also attempted human experiments in intravenous injection. For this Macht reports that Wren used "the delinquent servant of a foreign ambassador", but the experiment was unsuccessful, as Macht observed:
"...the victim either really or craftily fell into a swoon and the experiment had to be discontinued." 4
It was at least 100 years before a syringe with an attached needle intended for puncturing the skin was first produced.
In 1807 The Edinburgh Medical and Surgical Dictionary defined a syringe as follows:
"A well known instrument, serving to imbibe or suck in a quantity of fluid and afterwards expel the same with violence. A syringe is used for transmitting injections into cavities and canals." 5
However, the same source describes injection as being employed almost solely for injecting substances into the blood vessels of corpses for the purpose of enhancing anatomical study. Various developments towards the modern syringe were made as a result of the study and teaching of anatomy in 17th and 18th centuries.
In the 17th century, De Graaf made a device that closely resembled the modern syringe. Its purpose was to trace the blood vessels of corpses. His syringe had a metal barrel to which the needle was attached directly.
Figure 1.1: Clyster
Wellcome Institute, London
Early experiments
Intravenous injecting continued and was further developed in the 17th century. Numerous drugs were used to attempt to treat various conditions, particularly epilepsy and syphilis.
One of the first drugs injected in this way was opium4.
The use of this administration route declined however, probably as a result of the unsuitable substances injected (such as cinnamon, oil of sulphur and arsenic) and an unsurprising lack of encouraging results.
Absorption of drugs through the skin
At the beginning of the 19th century attempts were made to introduce drugs into the body via the skin itself. This initially took the form of variations on a general theme of blistering an area, removing the outer layer of skin and placing a poultice or plaster containing the active agent on to it. Lafargue developed this idea in 1836 by introducing morphine under the epidermis with a vaccination lancet, i.e. a solid needle dipped in morphine and then pushed under the skin3.
By the middle of the century Lafargue had developed a technique of placing solid morphine-based pellets under the skin. Initially this was achieved by simply making a hole with a large needle and pushing the pellet into the hole. Over time an instrument was devised to aid this procedure which Lafargue called the 'seringue seche' or dry syringe.
Other variations of this method included work by Crombie who, in 1873, used a technique of coating silk thread with morphia, puncturing the skin with a needle and then drawing the impregnated thread under the skin. Crombie developed this technique because he felt that the hypodermic syringe was expensive and easily damaged.
The development of injecting
Experiments with intravenous injection were revived at the end of the 18th century with important discoveries of the dangers of large quantities of air being introduced into veins and the similar dangers of oil-based intravenous injections.
Figure 1.2: Early hypodermic syringe
By permission of the Oxford University Press6
Intravenous injection continued throughout the 19th century but was overshadowed towards the end of the century by the introduction of techniques of subcutaneous injecting, which at the time was seen as more versatile and useful.
Kane, in 18807, described intravenous injection principally as an unwanted consequence of subcutaneous injection and gave ways to avoid its occurrence. Macht writing as late as 1916 said:
"However useful intravenous medication may be in special cases, its field of application is certainly more limited than that of hypodermic (subcutaneous) injection..."4
Figure 1.3: Watch chain syringe from the late 19th century
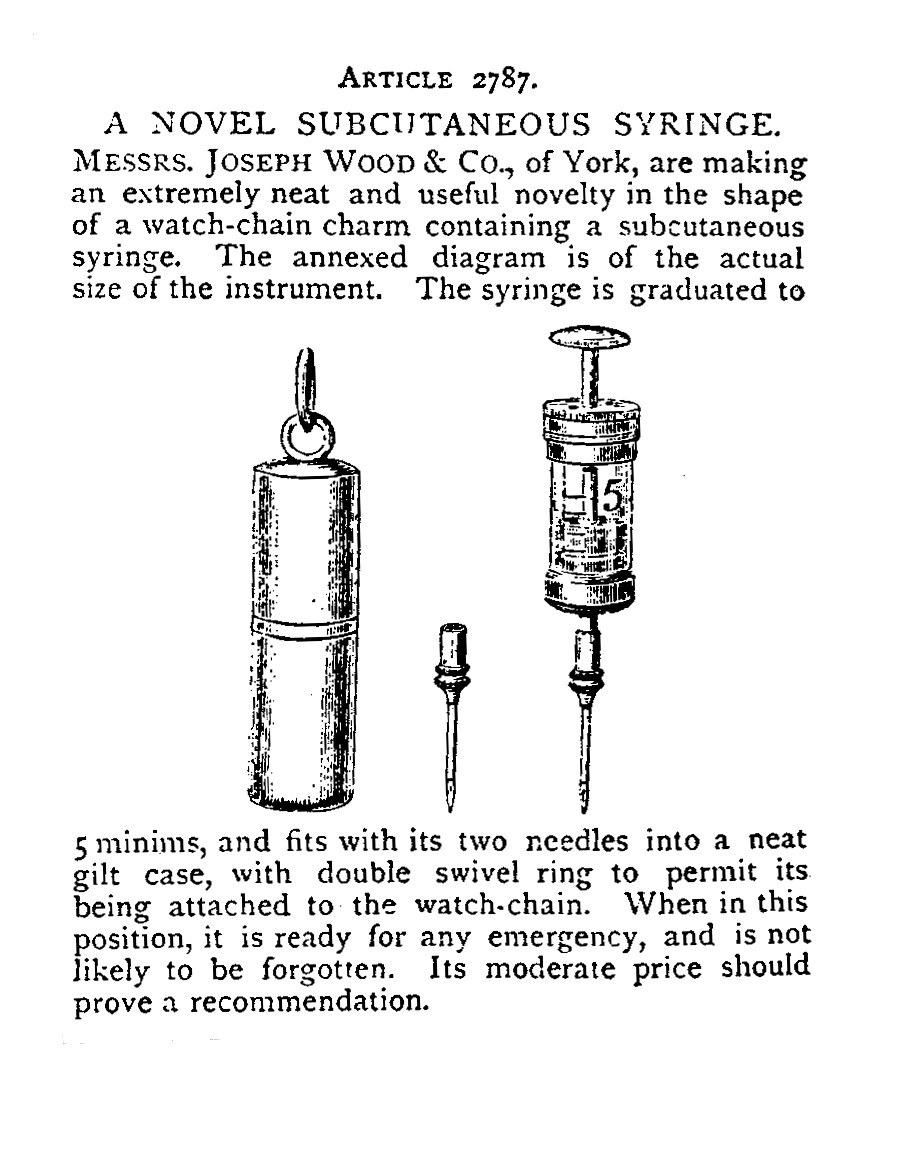
By permission of Oxford University Press6
Development of the modern syringe
The exact origins of the modern syringe are clouded in some uncertainty due to parallel developments by numerous inventors. However, the Fergusson syringe of 1853 became a forerunner of the modern syringe when Alexander Wood used it for subcutaneous injection of opiates for the relief of pain3.
Injecting and drug dependence
The development of understanding of systemic action
Systemic, means, having an effect on the entire body. Early understandings of the pain relieving effects of opiates centred on the belief that most of the drug stayed at the site at which it was injected. In fact, drugs administered by any route of injection will permeate throughout the body. Intravenous injection is the fastest route for drugs to reach the brain in concentrated form, subcutaneous injection is the slowest injected route.
Alexander Wood, although recognising some systemic action, believed that the action of opiates administered by subcutaneous injection was mainly localised. The use of the syringe over previous methods was thought to allow greater accuracy in administering the drug in close proximity to a nerve, hence it was thought, facilitating better pain relief.
The belief in localised action influenced many doctors at the time. Dr Francis Anstie, editor of The Practitioner, wrote in 1868 that there was no danger associated with the hypodermic injection of remedies, and later:
"... it is certainly the case that there is far less tendency with hypodermic than with gastric medication to rapid and large increase of the dose when morphia is used for a long time together."8
Charles Hunter, a house surgeon at St George's Hospital, made the connection that opiates administered by injection exert a systemic action when he was forced to move away from the original site of injection as a result of abscess formation and found that the patient still experienced similar relief from pain. This, as Berridge and Edwards have noted, "...led to a period of sustained and acrimonious debate between Wood and Hunter"9 about the existence or otherwise of systemic action.
Subcutaneous injecting with a syringe was initially described and popularised by Wood. It has been suggested that his fundamental misunderstanding that the effect was primarily local (and by implication that dependence could not occur), paved the way for the creation of a large number of patients dependent on morphine, described in the 19th century as 'morphinists'3 (Figure 1.4).
The growth of the medical use of opiates
A powerful influence in the development of widespread and repeated use of opiates by injection would have been the obvious and immediately beneficial effects of injected morphine, particularly to those experiencing chronic pain. Doctors at the time, with few truly effective treatments available, would have had difficulty in resisting the impulse to treat pain with something as powerful, fast and effective as injected morphine.
Courtwright, when discussing 19th-century opiate addiction in America, has said:
"The administration of opium and morphine by physicians was the leading cause of opiate addiction in the nineteenth century... case histories, clinical notes and remarks in the medical literature support the view that although opium and morphine were ultimately given for such unlikely disorders as masturbation, photophobia, nymphomania and 'violent hiccough' it was principally in those suffering from chronic ailments that the use of these drugs led to chronic addiction."10
The combination of the development and spread of injecting with the widespread availability of opiates and the easy legal availability of opiate-based patent medicines contributed to the increase in injectors of opiates in this period.
Figure 1.4: The final hours of a morphinist
By permission of Oxford University Press6
Injecting in the 20th century
Non-medical injecting of drugs grew through the 20th century. Initially the preferred route of injection by non-medical users was subcutaneous injection. In the USA, between the first and second world wars11, the preferred route gradually became intravenous injection. With a change of route of administration came a change in the medical problems commonly experienced by injectors. In the UK there were comparatively few injectors until the 1960s.
Needle sharing early research into injecting practice and infection spread
In the 19th century there was only a slow dawning of the realisation of the implications for the spread of infection by injecting. The concept of anti-sepsis was introduced by Lister in 1867. One of the earliest recorded cases of infection following injection was the report, in The Lancet in 187612, of a drug injector becoming infected with tetanus. The risk of tetanus and similar infections remains current for some subcutaneous injectors.
Needle sharing was described as being associated with infection spread in the 1920s. Malaria was first reported as a result of intravenous drug use in Egypt in 192913.
Crane14 summarises the recognition of various infections transmitted by injecting in the USA in the 1930s. At this time injectors of street drugs would probably have used a medicine dropper attached to a hypodermic needle with the aid of a cigarette paper in order to make a tight seal.
The role of needle sharing in the transmission of hepatitis A and B among injecting drug users was probably first described well, in an important American paper by Howard and Borges15 published in 1971.
Many of the infective complications of injecting drug use detailed in sections 6 and 7 of this book were recognised over the intervening years. In the early 1980s, the discovery of the
HIV virus and its routes of transmission, leant greater urgency to the study of injecting practice and infection spread. Almost a decade later, hepatitis C was identified as a risk for injectors.
The switch to disposable syringes and needles
Through the 20th century the production of precision-made glass syringes was gradually refined. The first major advance came with the manufacture of interchangeable parts, made to exact specifications, rather than as 'one-off' items.
Until the 1960s the majority of syringes and needles were re-useable and were supplied unsterilised. They had to be sterilised before each use.
Glass syringes could be re-sterilised approximately 20 times before they were in danger of breaking. Needles had to be re-sterilised and re-sharpened.
The 1950s was a period of transition, with 'hybrid' combinations of plastic and glass disposables.16
By the 1960s, glass syringes which were re-useable after sterilisation were being replaced with disposable plastic syringes and single-use needles.
However, at that time the concept of disposability was still new and manufacturers were concerned that attempts would be made to re-sterilise single-use equipment. To discourage re-use, the manufacturers experimented with materials for syringes that could not withstand the temperatures involved in heat sterilisation. The first type of plastic chosen for this use was polystyrene, but this was found to be vulnerable to chemical attack from the contents of the syringe.
Figure 1.5: Early advert for plastic disposable syringes (1961)
TO SAFEGUARD THE PATIENT TO SAVE TIME AND MONEY
PLASTIPAK
Infectious hepatitis, a growing health menace, has been traced in many instances to the re-use of syringes and needles believed to have been sterile.1-3 Other types of infections among hospitalized patients have also been attributed to the use of inadequately sterilized equipment.1-4 This indictment of hypodermic needles as a factor in the transmission of hepatitis and the growing conviction that other cross-infections may be incurred in the same manner, have cast serious doubts on the adequacy of conventional methods of sterilization1 and on the wisdom of using syringes and needles more than once.1-4
Moreover, hospitals today are confronted by mounting labor costs and a severe shortage of properly trained personnel at the very time that their facilities are most heavily taxed. Patient loads increase daily, and demands for more specialized and more exacting hospital care continue to grow.
These two vital considerations have made the use of disposable equipment almost mandatory practice. Patient safety1-4 and the inescapable dictum that 'time is money'1-5 have given rise to a par-ticular demand for sterile disposable syringes and hypodermic needles, assembled as a unit in packages that are easy to store, easy to identify, and easy to handle.
Becton, Dickinson and Company was the first manufacturer by many yearsto enter the field of disposables. Its disposable syringe program began in 1944, and for the past 17 years B-D has supplied many millions of disposables, all manufactured to conform to exacting and unremitting standards.
Yet, it is only now that the company is introducing PLASTIPAK, the sterile disposable plastic syringe for medical use. Why? Previous disposable syringes made by B-D were glass, and glass was known to be safe. But B-D was not satisfied with plastic materials available
at that time. It was not until a plastic which met every B-D safety test for injection use was developed that B-D undertook the manufacture
of plastic disposable syringes.
Polypropylene disposable syringes began to revolutionise the syringe market from 1961 onwards. Latex has been used in syringe manufacture, but there are now latex-free syringes available because some people are allergic to it.Today almost all syringes and needles are disposable and intended for 'once-only use'.
Injection and dependent drug use today
The act of using a needle and syringe to introduce drugs into the body holds a great deal of cultural symbolism both inside and outside injecting networks.
Intravenous drug use is popularly seen as an end result of a career of drug use. Injecting drug users are often characterised as being out of control or controlled by their drug use. Whilst for some injecting drug users this is true, there are many injectors who do exercise control. It seems that the majority of injectors have a level of concern about their health and are prepared, given the means and instruction, to take precautions to maintain it17.
The subjective phenomena that differentiates injecting from other routes of taking drugs is the immediacy and strength of the onset of action and the experience of a 'rush'.
A significant factor in the numbers of people using heroin by injection in the UK, was the increase in availability of cheap smokeable heroin in the 1980s. Smoking was and still is seen as a much more accessible way of taking drugs than injecting, with its attendant taboos18. Although many people who initially smoked heroin continued to use that route even after establishing dependence, many heroin smokers certainly made the transition to injecting heroin. That some drug users continue to move between the two routes, after taking up injecting, is sometimes not well appreciated19.
| Figure 1.6: 1987 UK national poster campaign |
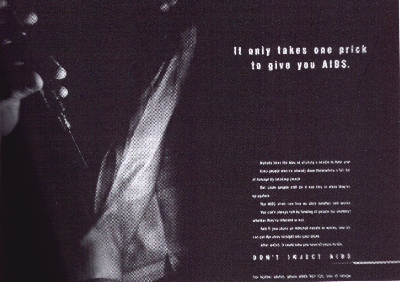 |
| Figure 1.7: 1989 national poster campaign |
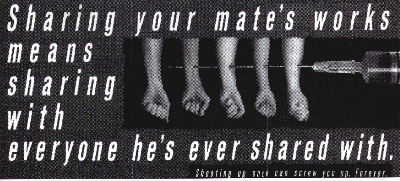 |
The 'Edinburgh experience'
In 1986 it became apparent that Edinburgh had a serious problem with a high prevalence of HIV positive injecting drug users20.
An influential paper published in the British Medical Journal in 1986 by Robertson et al.21 reported the testing for HIV of blood samples that had been systematically stored since 1982. These samples had been taken following the discovery of increasing numbers of hepatitis B positive heroin users. It later emerged that the cause of this increase was an acute shortage of injecting equipment following the closure of the main supplier and a voluntary sales ban by local community pharmacists at the request of the police.
On testing the stored blood of this group of 164 injecting drug users for HIV, it was found that 51% of the samples were HIV positive. It was possible to pinpoint the time of seroconversion for 33 of the sample to a period between the end of 1983 and the beginning of 1984.
Extrapolating from these figures, Robertson et al. suggested that the true prevalence rate of HIV positive injectors in Edinburgh in 1986 could have been as high as 85%. From interviews with 40 of the group, it was possible to establish that as clean injecting equipment became harder to obtain, the group formed an intimate equipment-sharing community21, with reports of gatherings of 1020 injectors using one syringe and needle. Comparisons were made by Robertson et al. with the similar 'shooting galleries' reported from the USA.
The development of UK service provision
Clean injecting equipment for illicit drug users was first provided in the late 1960s to those few injectors who were given a prescription of injectable heroin or methadone.
Injecting equipment had been available for sale to injecting drug users since the late 1960s. Between 1982 and 1986 the Royal Pharmaceutical Society recommended that needles and syringes should only be sold to bona fide patients for therapeutic purposes. Although this policy was not adopted by all community pharmacists, it certainly reduced the overall availability of needles and syringes. The recommendation was withdrawn in 1986 because of concern about the spread of HIV.
Needle and syringe exchange services began officially in the UK in 1987, when the DHSS commissioned a pilot study to evaluate their effectiveness.
At the time that needle exchanges came into being in the UK, there was huge anxiety amongst the general population about the perceived threat of AIDS, fuelled by the media and by government sponsored advertising campaigns. Injecting drug use was identified early on as being one of the major potential risk behaviours for HIV infection.
Injecting drug users could hardly fail to know that they were at high risk of contracting a potentially fatal condition. The prevailing view of injecting drug users in the mid-1980s was that they were deviant, self-indulgent and often out of control; the idea that injecting drug users might alter their behaviour on a widespread basis to reduce their risks was fairly novel. Needle exchanges provided the means for many to reduce their HIV risk behaviour.
The first dedicated needle exchange to begin operating in the UK was in Peterborough in early 1986. The first pharmacy scheme began operation by Boots in Sheffield in the same year.
The Kaleidoscope needle exchange in South London began operating in September 1986 as part of a wider church-based project which was also involved in methadone prescription and other, non drug-related social problems. The project was established in purpose-built accommodation and was unusual for UK schemes in that it was open seven days a week from 7am to 11pm and remained open all night on Fridays.
The Maryland Street needle exchange in Liverpool began operating in October 1986 from a modified toilet within the Mersey Drug Training and Information Centre, sited next door to the drug dependency unit. The opening hours were 9.305.30, Monday to Friday.
The DHSS initially set the following criteria for pilot schemes; they should:
![]() Provide injecting equipment on an exchange basis to drug users already injecting and unable or unwilling to stop
Provide injecting equipment on an exchange basis to drug users already injecting and unable or unwilling to stop
![]() Provide assessment of and counselling for clients' drug problems
Provide assessment of and counselling for clients' drug problems
![]() Provide advice on safer sex and offer counselling on HIV testing
Provide advice on safer sex and offer counselling on HIV testing
![]() Collect information on clients and collaborate with a monitoring and evaluation project.
Collect information on clients and collaborate with a monitoring and evaluation project.
At this time projects were largely staffed by nurses who received little specific training on the subject of safer injecting.
The DHSS simultaneously commissioned an evaluation of syringe exchange schemes nationally. Reporting on these, Stimson et al.22 concluded that needle exchanges reached:
![]() Considerable numbers of injectors
Considerable numbers of injectors
![]() Many injectors who were not in contact with any services.
Many injectors who were not in contact with any services.
They tended to attract:
![]() Opiate users primarily
Opiate users primarily
![]() Older, long-term injectors
Older, long-term injectors
![]() Fewer females than males.
Fewer females than males.
As needle exchange was seen to be effective, did not outrage public opinion or cause other anticipated potential problems, the network of needle exchange schemes expanded rapidly across the country, alongside a national expansion in the substitute prescribing of methadone.
A 'user friendly' approach
The term 'user friendly' to describe the philosophy of needle exchange was employed to make the distinction between needle exchange and the other, abstinence orientated services that were available for drug users in the mid-1980s.
This term, borrowed from the computer industry and applied to syringe exchange, encapsulated some of the fundamental principles underpinning successful exchanges, which still apply today:
![]() No waiting lists
No waiting lists
![]() Required a minimum of information from clients
Required a minimum of information from clients
![]() No entry criteria apart from injecting drug use
No entry criteria apart from injecting drug use
![]() Easy access
Easy access
![]() No requirement to change drug use i.e. stop injecting.
No requirement to change drug use i.e. stop injecting.
There was also a commitment to provide:
![]() Accurate information about the risks of injecting drug use
Accurate information about the risks of injecting drug use
![]() Encouragement to adopt safer injecting practices.
Encouragement to adopt safer injecting practices.
The balance between being user friendly and providing the information that injecting drug users need to reduce the risks that they are exposed to is one that many services have struggled with. Difficult though this balance can be, being user friendly is not a good enough reason to fail to deliver essential harm reduction information.
The public health response
In the mid-1980s UK drug treatment services had become largely focused on the achievement of abstinence. Whilst this approach may have been appropriate for those drug users wishing to stop taking drugs, the evident public health threat from HIV meant that new approaches had to be found.
The objectives of a public health based approach were to:
![]() Make contact with the whole population at risk
Make contact with the whole population at risk
![]() Maintain contact
Maintain contact
![]() Encourage behaviour change.
Encourage behaviour change.
The Advisory Council on the Misuse of Drugs presented the following hierarchy of goals in 1988:23
![]() Reduce sharing of injecting equipment
Reduce sharing of injecting equipment
![]() Reduce the incidence of injecting
Reduce the incidence of injecting
![]() Reduce the use of street drugs
Reduce the use of street drugs
![]() Reduce the use of prescribed drugs
Reduce the use of prescribed drugs
![]() Increase abstinence.
Increase abstinence.
This approach became closely identified with what became known as the 'harm reduction model'. One of the driving forces behind the development of the harm reduction model on Merseyside was Howard Seymour. In a paper given in 199724, Seymour expressed his concern that:
"the population based public health response to high risk drug use, which characterised the 'Merseyside model', has been lost or diluted in many places in the UK, into a clinical, individually oriented model."
Current UK service provision
Current UK service provision for injecting drug users represents a major expansion in the number and type of schemes. Every area in the UK, with the possible exclusion of Northern Ireland, has at least some provision for the exchange of injecting equipment.
A 1997 survey by The Centre for Research on Drugs and Health Behaviour25 suggests that there are approximately:
![]() 637 non-pharmacy exchange outlets
637 non-pharmacy exchange outlets
![]() 1695 pharmacy exchange outlets.
1695 pharmacy exchange outlets.
Non-pharmacy schemes include specialist schemes, mobile services, A&E departments and outreach projects.
The figure given for non-pharmacy schemes is an extrapolation from a 78% questionnaire return rate. The figure given for pharmacy based schemes is an extrapolation from a 62% questionnaire return rate.
This growth reflects the success of a combination of strategies in averting epidemic spread of HIV amongst injecting drug users including:
![]() Needle exchange
Needle exchange
![]() Methadone prescribing
Methadone prescribing
![]() Outreach services.26
Outreach services.26
Centre-based needle exchange schemes
The majority of 'street agencies', whether statutory or non-statutory, incorporate needle and syringe exchange as part of their service provision.
The level of service on offer varies greatly from scheme to scheme. At one extreme administration and reception staff who have little or no training in safer injecting, simply offer a facility for clients to collect and dispose of equipment. At the other end of the spectrum there are many services solely designated to provide needle exchange which have facilities for seeing clients in private and which offer a wide range of services, advice and support from trained staff.
Community pharmacy needle exchange
Since 1986 there has been a great increase in the numbers of community pharmacists prepared to provide syringes and needles. According to a study by The Centre for Research on Drugs and Health Behaviour there are now about 1700 UK community pharmacists who are paid to dispense sterile equipment free to drug users and dispose of used equipment as part of the pharmacy needle exchange scheme. A survey of more than 2000 community pharmacies, commissioned by the Task Force to Review Services for Drug Misusers in England27, found that:
![]() 19% of those who replied were involved in needle exchange
19% of those who replied were involved in needle exchange
![]() Another 36% were prepared to be involved if a pharmacy exchange scheme was set up in their area.
Another 36% were prepared to be involved if a pharmacy exchange scheme was set up in their area.
The overall percentage of those prepared to be involved had not changed over the previous eight years.
Reasons given for not becoming involved in needle exchange were:
![]() Another needle exchange nearby
Another needle exchange nearby
![]() Client behaviour
Client behaviour
![]() Lack of time and space.
Lack of time and space.
Community pharmacies are an important means whereby injectors can obtain clean injecting equipment. They are more widespread than specialist agencies, offering access to sterile equipment in rural settings. They have more flexible opening hours and can provide basic health advice. Also, they may be more attractive to some injectors not in contact with any specialist services, because they may more easily be able to maintain anonymity.
Although there is no formal recommendation to pharmacists, the limitations of working within a retail environment mean that pharmacy exchanges cannot provide specialist advice or services for those they know to be under 16 years of age. It would be impossible for them to undertake assessment procedures for under-age injectors (see page 100).
Community pharmacy sales of injecting equipment
As well as the widespread network of pharmacies offering a free exchange service, many pharmacies provide injecting equipment for sale. This has helped to plug some of the gaps in the provision of free equipment across the country.
Guidance to pharmacists, effective from April 1998, from the Royal Pharmaceutical Society, instructed them to sell equipment only in 'exceptional circumstances', if they did not have arrangements for the return of used equipment28.
Since the majority of pharmacies that sell injecting equipment do not have such facilities, early indications are that this guidance will trigger a reduction in this important, informal part of the distribution network. In some areas it may mean the loss of the only provider of sterile equipment.
In Berkshire the pharmacy needle exchange scheme has been widened to include provision of disposal facilities to many pharmacies selling injecting equipment. Customers are also informed of sites which give free needle exchange.
A&E departments
Many A&E departments in the UK provide a limited range of injecting equipment, although few advertise the fact. Drug injectors are likely to attend A&E departments more than the norm because of:
![]() Not having a GP
Not having a GP
![]() Drug-related injuries
Drug-related injuries
![]() Overdose.
Overdose.
The Task Force to Review Services for Drug Misusers27 recognised a potential for A&E departments to provide syringe exchange facilities.
General practitioners
General practitioners in the UK do not often give out injecting equipment to their patients. It is unlikely that many injectors would feel comfortable asking their GP for injecting equipment.
However, if a GP knows that a patient is injecting, it would be good practice to offer them clean injecting equipment, where appropriate, and to refer them to a pharmacy scheme or specialist syringe exchange where there are complicating factors, such as clients under 16 years of age.
Mobile exchanges
Mobile exchanges can represent a useful resource for those injectors who do not access existing services consistently. Mobile exchanges or exchanges by outreach workers can also be valuable in rural settings.
A good practice example of a successful mobile exchange service, which also provides a measure of primary health care for its users, is the MASH (Manchester Action on Street Health) trailer, which operates in the Greater Manchester area.
The main remit of the MASH trailer is to contact traditionally hard to reach groups such as:
![]() Women
Women
![]() Male and female sex workers
Male and female sex workers
![]() Young injectors
Young injectors
![]() Amphetamine injectors
Amphetamine injectors
in order to make injecting equipment, injecting advice, contraceptives and advice on safer sex and sexual health available to them. The van has a clinical examination room as well as exchange facilities and the services of a doctor, nurses and a drug liaison midwife.
Satellite schemes
Providing sterile injecting in settings such as users' houses, dealers' houses or 'shooting galleries', can help ensure that injecting equipment is not shared because of lack of immediate availability.
Dispensing machines
Dispensing machines are available commercially and may represent a useful addition to services. Although it would be desirable for all schemes to have clean equipment and secure disposal points available somehow outside normal working hours, dispensing machines are particularly useful for those services which have sporadic opening hours.
Most machines operate on a 'one for one' basis, i.e. a used syringe or a token has to be deposited for a sterile one to be dispensed. Some pilot prison needle exchange programmes operating in Europe use dispensing machines.
Current worldwide service provision
USA
Syringe and needle exchanges remain contentious in the USA, and in many states are run illegally. The US Government's antipathy to well-accepted public health measures against blood-borne disease transmission has its roots in their political and cultural response to illicit drug use.
The following list summarises the main reasons why harm reduction services are severely restricted in the USA:
![]() The absolute political dominance of a prohibitionist stance and commitment to the 'war on drugs'
The absolute political dominance of a prohibitionist stance and commitment to the 'war on drugs'
![]() A belief that accepting needle exchange would imply acceptance of drug use and thereby undermine a prohibitionist stance
A belief that accepting needle exchange would imply acceptance of drug use and thereby undermine a prohibitionist stance
![]() Lack of political will there are more votes in being seen to be hard on drugs
Lack of political will there are more votes in being seen to be hard on drugs
![]() Insistence that needle exchange has not been proven in clinical trials (despite the fact that a controlled trial would be impossible to conduct in this field)
Insistence that needle exchange has not been proven in clinical trials (despite the fact that a controlled trial would be impossible to conduct in this field)
![]() A belief (unsupported by the evidence) that the implementation of needle exchange, in removing some of the risks associated with injecting, encourages injecting
A belief (unsupported by the evidence) that the implementation of needle exchange, in removing some of the risks associated with injecting, encourages injecting
![]() A belief that the possible consequences of injecting drug use are known about by users, and they are therefore exercising informed choice.
A belief that the possible consequences of injecting drug use are known about by users, and they are therefore exercising informed choice.
In addition there has been an understandable suspicion amongst black communities that needle exchange services may be part of a racist public health policy designed to get and keep young black people on drugs. This suspicion is rooted in the historical fact that indefensible 'health' policies have previously been pursued in the USA. The most notorious example of this was the case of the 'Tuskegee experiment' which left many black syphilis sufferers untreated in order to examine the natural course of the disease despite this being well documented already and treatments being available.
In 1995 John Watters, an American epidemiologist, wrote the following powerful indictment of the continued absence of adequate harm reduction services in the USA:
"Opponents of syringe exchange... insist on unrealistic and unfeasible standards for evaluating outcomes. In dismissing existing studies, resistance to syringe exchange sets criteria for evaluation that have not been required of a dizzying array of social programmes, surgical interventions and drug based therapies. Of course what is needed is the political will to make the public health decisions which hold out the greatest likelihood of reducing continued HIV contagion. Politics is however a short sighted profession. Its collective vision rarely extends past the next election. Consequently, resistance to syringe exchange in the United States continues to hold sway."29
Numbers of exchanges and HIV prevalence statistics
The number of needle exchange programmes in the USA grew only to a meagre 87 in
1995/96, more than half of which were in California, Connecticut, New York and Washington state.
In 1995/96, around half of the needle exchanges were legal. Of the rest, half were illegal and the other half were against state law, but were locally approved.
Seroprevalence for HIV amongst injecting drug users in several large east coast cities on 1989 figures was in the 3060% range. In most areas the prevalence was 5-20%30.
Based on conservative assumptions, Lurie and Drucker estimated that there would have been between 4400 and 10000 fewer HIV infections amongst injecting drug users if the USA had embraced needle exchange in 1987. They also concluded that if current policies are maintained there will be between 5150 and 11329 preventable further infections by the year 200031.
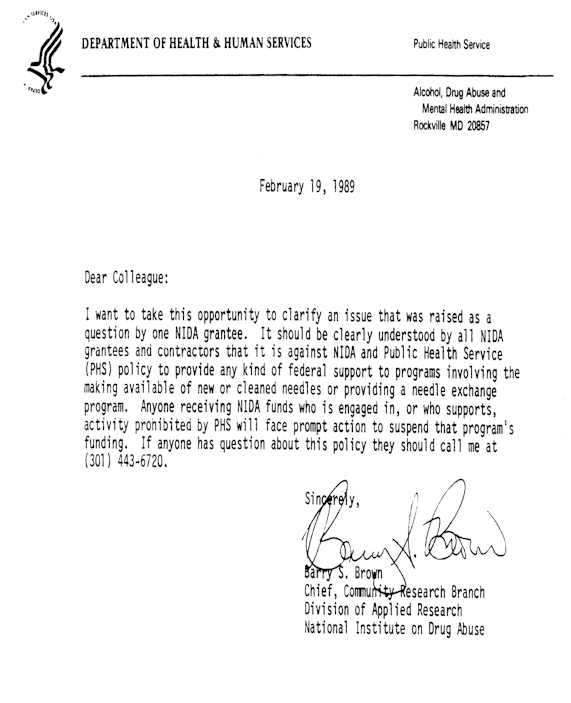
Figure 1.8: Anti-needle exchange letter
(National Institute on Drug Abuse) 1989
The Netherlands
The availability of syringes in Amsterdam became problematic at the end of 1982 before the advent of HIV when one of the few pharmacies selling sterile equipment in the inner city, stopped, probably because of increasing demand and associated problems. A market for used syringes, sometimes selling for as much as 25 Guilders (almost £10), emerged rapidly.
The immediate, obvious consequences of this were:
![]() Unhygienic use resulting in abscesses and hepatitis
Unhygienic use resulting in abscesses and hepatitis
![]() Increased dependency on the syringe retailer (often the dealer).
Increased dependency on the syringe retailer (often the dealer).
The Amsterdam 'MDHG' an interest group for drug users together with other organisations in the drug field attempted to find solutions. They held discussions with the pharmacy that had suspended sales and looked for alternative distribution points such as other pharmacies, drug stores and shops.They took part in a 'syringe working committee' and started a referral system so users could get their syringes from their own pharmacies through the social security system. However, none of these measures seemed to have a noticeable effect.
A number of organisations, including the MDHG, decided to initiate needle exchange schemes. The claim to have been the first Dutch needle exchange is disputed between MDHG of Amsterdam and 'de Junkiebond' of Rotterdam which both started in 1984.
However there is also evidence that there was needle exchange provision as early as 1981 in the cities of Groningen and Den Helder.
Between 1984 and 1986 the MDHG learned some fundamental lessons in the effective provision of injecting equipment which continue to have resonance today. One of the most important of these was that the exchange of clean equipment alone was not enough. Establishing trusting relationships so that information about safer injecting techniques or health related issues could be discussed, was vital in order to make these initiatives successful. The Netherlands now has a widespread network of needle exchanges.
Italy
Needle exchange was introduced relatively late in Italy in comparison to much of Western Europe, although sterile injecting equipment has long been available through such unlikely outlets as supermarkets. The main reasons for this late start had to do with cultural barriers that favoured therapeutic abstinence-based initiatives over preventive interventions.
The first street outreach project was initiated in 1991 in Milan. Syringes were exchanged both by outreach workers and by needle exchange machines. Soon other areas in Italy including Genoa,Turin, Florence, Rome and Palermo followed.
In Rome, in March 1992, Fondazione Villa Maraini and the Italian Red Cross opened an outreach unit at Rome central station.
In Turin, Gruppo Abele had been planning the introduction of harm reduction services since 1990, but did not receive the support of the city's public services until 1994, resulting in the funding of a project by the Regione Piemonte in 1995. This project consisted of a mobile unit with an outreach team.
In 1993, the Regione Lazio funded the Integrated Harm Reduction Programme, in which both public and private services began to work together. Apart from drop-in centres, emergency services and methadone treatment, the project consisted of three street outreach units and needle exchange. Needles were exchanged both by outreach workers and by exchange machines.
Germany
Syringe exchange has existed in Germany since 1987, although it has only been legal since 1992. While established programmes are functioning successfully in large cities such as Hamburg, Bremen and Frankfurt, the demand for sterile needles and syringes remains poorly met in smaller cities and in the conservative governed states, where pharmacies remain the primary and often only legal supply source for syringes. Although injecting drug use is common in prisons, injection equipment is not legally available for the 10000 injecting drug users imprisoned at any given time. Two of Germany's 220 prisons started experimental syringe exchanges in 199632.
Australia
Since the mid-1980s Australia has developed extensive free needle exchange provision which covers most of the urban areas of the country, although the numbers of exchanges vary from state to state. An important development was the Pharmacy Guild Fitpack Scheme which allowed injectors to buy special packs which held injecting equipment and doubled as a sharps container; once full this could then be exchanged free of charge for a new one.
A key feature of many Australian programmes has been the successful involvement of drug users many projects are staffed and run by past or current drug users.
Another feature of Australian programmes that is by no means unique but perhaps more essential because of the rural nature of large parts of the country has been the development of mobile exchanges.
As is the case in other countries, self-reports of sharing of injecting equipment the norm in the mid-1980s had become comparatively rare by the mid-1990s.
Eastern Europe
There is little published information available about the numbers of injectors or the prevalence of HIV infection amongst them in Eastern Europe. Very few formal needle exchanges exist; the first in Russia were established recently in St Petersburg and Yaroslavl, funded by Medecin du Monde (France) and Echo (Connecticut, USA).
Reports from some areas of the high prevalence of HIV among large populations of injectors, and of widespread use of opiate preparations made from poppy straw and sold in or from pre-loaded syringes are worrying. In relatively poor countries with small health care budgets there is little or no funding available for the provision of sterile equipment, and the equipment that is available is likely to be re-used many times.
Asia
Sujata Rana wrote in 1997:
"...the HIV epidemic began in Asia years after this virus had been identified and at a time when effective ways of preventing the spread of HIV among drug injectors had become known in many developed countries around the world. However, despite this knowledge, it is estimated by the year 2000, there will be more people infected with HIV in Asia than all of Africa..."33
However needle exchange is not absent from Asia. Nepal has been notable in its acceptance of the philosophies of harm reduction and effective needle exchange programmes have existed in Kathmandu and Pokhara for several years. The state of Manipur in North East India has also implemented needle exchange and other harm reduction measures following findings of overwhelming levels of HIV infection amongst injecting drug users there.
A situation assessment on drug use and HIV vulnerability in South east and East Asia prepared for the UNAIDS Asia Pacific Inter Country Team by the Asian Harm Reduction Network34 included the following conclusions:
![]() HIV infection among injecting drug users in South East and East Asia is a major problem
HIV infection among injecting drug users in South East and East Asia is a major problem
![]() Few if any countries have responded to it effectively
Few if any countries have responded to it effectively
![]() There are large gaps in information
There are large gaps in information
![]() The situation is dynamic, new drugs are constantly appearing and new populations are becoming involved with drug use
The situation is dynamic, new drugs are constantly appearing and new populations are becoming involved with drug use
![]() Explosive epidemics of HIV have occurred among injectors and will continue to happen if nothing is done.
Explosive epidemics of HIV have occurred among injectors and will continue to happen if nothing is done.
nternational harm reduction movements
Recent international developments in harm reduction have included the development of the , and the consisting of the , , and Harm Reduction Networks. These organisations exist in order to promote and develop the philosophies and principles of harm reduction worldwide.
Contact details for these organisations can be obtained through the links to their web sites above or from HIT, tel 0151 227 4012.
Key events in the development of injecting drug use
1656 Wren experiments with intravenous injecting
1850s Fergusson syringe developed
1853 Fergusson syringe adapted and used by Wood for subcutaneous injection
1858 Hunter realises systemic action of subcutaneous injection
1867 Lister develops the concept of antisepsis
1860s Subcutaneous injection of morphine 'popularised'
1874 Diacetyl morphine (heroin) synthesised
1876 Infection spread recognised as a complication of subcutaneous injecting (tetanus)
1920s First reports of 'illicit' intravenous drug use
1930s First reports of infective complications of intravenous drug use (malaria)
Needle sharing recognised as a transmission route for disease
1940s/'50s Intravenous route becomes the norm for illicit injectors
1960s Disposable plastic syringes and needles introduced
Injection of crushed tablets first reported
Hepatitis B transmission risk recognised
1980s HIV transmission risk recognised pilot needle exchange schemes began in the UK
1990s Hepatitis C identified and transmission risk recognised
Key points
![]() The first intravenous injections probably took place in the 17th century.
The first intravenous injections probably took place in the 17th century.
![]() At first it was thought that injections only acted locally and that there was therefore little risk of dependence.
At first it was thought that injections only acted locally and that there was therefore little risk of dependence.
![]() The forerunner of the modern syringe was probably the Fergusson syringe of 1853.
The forerunner of the modern syringe was probably the Fergusson syringe of 1853.
![]() The modern disposable syringe was developed in the 1960s.
The modern disposable syringe was developed in the 1960s.
![]() The provision of syringe exchange to prevent the spread of HIV has been strongly resisted in some countries including the USA.
The provision of syringe exchange to prevent the spread of HIV has been strongly resisted in some countries including the USA.
![]() Syringe exchange exists in all areas of the UK, with the probable exception of Northern Ireland.
Syringe exchange exists in all areas of the UK, with the probable exception of Northern Ireland.
Last Updated (Wednesday, 05 January 2011 23:05)
Last Updated (Thursday, 06 January 2011 11:10)









