| - |
Drug Abuse
A.2 Opiate Narcotics
INTRODUCTION
The term narcotic has had wide and inconsistent usage in lay, legal and scientific circles. Some use the word to characterize any drug which produces stupor, insensibility or sleep; many apply it only to derivatives of the opium plant ( `opiates'); others consider the term equivalent to 'addiction-producing'; and in legal matters, 'narcotics' may refer to almost any allegedly dangerous drugs, (for example, marijuana and cocaine are often included with opiate compounds in narcotics regulations in spite of the dissimilarity of their effects). To reduce some of this ambiguity, the specific phrase opiate narcotic is used in this report and is restricted to opium, morphine and related alkaloids obtained from the opium poppy plant (Popover somniferum), and the semi-synthetic derivatives of these alkaloids and wholly synthetic substances with similar pharmacological properties. Opium is prepared from the dried juice of the unripe seed pod (capsule) of the poppy plant, obtained soon after the flower petals begin to fall; the alkaloids are obtained from opium by various extraction processes.
In 1803, the major active constituent in opium was isolated—an alkaloid given the name morphine after the Greek god of dreams, Morpheus. Raw opium is about ten per cent morphine by weight. In the next half century, various other active alkaloids, such as codeine (methylmorphine), were discovered.113, 145, 218 Since then, hundreds of semi-synthetic and wholly synthetic morphine-like drugs have been developed. Heroin (diacetylmorphine) and hydromorphone (Dilaudid®) are semi-synthetic compounds derived from morphine. Fully synthetic drugs in this class include methadone (Dolophine® in the U.S.), piminodine (Alvodine®) and pethidine (also called meperidine or Demerol®). These various natural and synthetic compounds have the potential of producing qualitatively similar actions (at different doses), although there is considerable variability among them in the potency of their various effects. With a few exceptions they will be dealt with as a group, with morphine as the prototype.
Heroin is several times more potent on a weight basis than morphine, but is otherwise not significantly different in action from it.62, 130, 147, 228 Heroin was originally considered 'non-addictive' when first introduced at the end of the 19th century, and was even suggested as a cure for opium and morphine dependence.8, 218 Heroin is usually the choice of the chronic opiate narcotic user in North America today, although members of the medical and related professions who use these drugs non-medically, as well as others who have become dependent as a result of medical use, usually take morphine or the synthetics. Methadone, first used for its analgesic properties, has become important in the management of opiate narcotic dependence, and has recently gained some popularity among illicit users. Although methadone will be mentioned from time to time in this general opiate narcotic discussion, a separate overview of methadone and its long-acting derivatives is presented later in this section. Heroin is often referred to as 'H', 'junk', 'smack', `scag', `horse' or 'jazz'. Methadone may be called 'don' or 'dollies'.
Thebaine is an opium alkaloid, present in a number of poppy varieties, which has little morphine-like activity itself. A series of hundreds of semi-synthetic derivatives of thebaine have been developed which are referred to as the Bentley Compounds. Many of these compounds have morphine-like effects, and range in activity up to more than 1,000 times the potency of morphine and heroin. Some are equally effective opiate narcotic antagonists. One highly active drug, M-99 (Etorphine®) and a corresponding antagonist, M-5050 (Diprenorphine®) have received considerable attention and are available for veterinary use in the United States.4, 94, 137, 221 As yet, there are no indications of thebaine derivatives entering the illicit market.
Propoxyphene is a synthetic compound, chemically related to methadone, which is primarily used medically to relieve light or moderate pain, typically in combination with acetylsalicylic acid (A.S.A.) as in some Darvon® preparations. Although originally introduced as a "non-narcotic analgesic", there is growing evidence that propoxyphene is more like the narcotic analgesics than was formerly realized. Its psychological effects are similar to those of codeine in many respects. The appropriate pharmacological classification of propoxyphene is still a matter of some controversy, but it is considered with the opiate narcotics in this report. Similarly, pentazocine (TalwinC)) was once heralded as an effective non-narcotic analgesic, but it is now recognized that this drug has significant morphine-like properties and can produce dependence. Dextromethorphan is often referred to as a non-narcotic antitussive and is present in some cough medicines such as Romilar®. The drug lacks significant analgesic properties and has little dependence liability, although it is sometimes used non-medically for its mild euphoric effects.
The earliest unambiguous description of opium to which we have access was written in the third century B.C., although some scholars have cited references to the medical and non-medical use of opium or opiate-like drugs dated more than 5,000 years ago.24, 145, 218 Many believe that Homer's `Nepenthe' was opium. More modern authors, such as De Quincy in 1821, have written extensively of the perils and pleasures of opium.53, 157
Although opium eating has been known in Asia for thousands of years, common use of the drug did not occur until the development of the British East India Company's wholesale opium empire in the 18th century. The practice of smoking opium developed later in China after American tobacco was introduced to the Orient. Chinese attempts at prohibition of the British-Indian opium precipitated the Opium Wars in the 1840s and 1850s, which forced China to open its doors to British (opium) trade.24, 48, 145, 189, 218, 218 The majority of the illegal opiates on the North American market today come originally from Southeast Asia in areas of Burma, Thailand and Laos, and from parts of the Middle East. However, India remains the major legal producer of opium. (See Appendix B.2 Sources and Distribution of Opiate Narcotics.)
Prior to the 19th century, opium was taken orally in various forms or smoked, and both practices have continued in some areas. There is a decidedly lower dependence liability with these modes of use than with practices which followed, and it was not until the isolation of morphine and the invention of the hypodermic needle that opiate narcotic use became a serious problem in the Western World. Morphine was widely acclaimed among medical practitioners, and injections were used freely to treat pain during the American Civil War, sometimes producing a dependence called, in those days, the 'army disease'. Tincture of opium was employed in many patent medicines and household remedies (such as Laudanum and Paregoric), and the quasi-medical oral use of such opiate preparations was a common practice in North America during the last century. While some degree of dependence is reported to have often developed as a result of this symptomatic treatment, the associated abstinence syndrome was typically mild and often not recognized as a product of drug use. The actual extent of opiate narcotic use and associated problems at that time is difficult to ascertain, since little systematic reporting was done; however, it would appear that the use of these drugs was not a major moral or legal issue. On the West Coast, the influx of Chinese labourers, some of whom smoked opium, apparently stimulated non-medical use to some degree. In the latter part of the 19th century and early part of the 20th century, restrictions on manufacture and trade of opiate products were instituted in North America. In many cases, non-medical possession was prohibited by criminal law.24. 26, 146, 218
The first special notice of opium use in Canada was the indirect result of the anti-Asiatic riots which took place in Vancouver in 1907.49 Mr. Mackenzie King, then Deputy Minister of Labour, was sent to British Columbia to process claims from the Chinese community for financial compensation. Two claims appeared from opium merchants for losses sustained in the riots. This prompted Mr. King to inquire into the opium trade as well as the causes of the labour unrest. In his opium report, he noted that the drug was making headway, "not only among white men and boys but also among women and girls", and recommended immediate and strict legal action.
Still little public notice was given to the opiate narcotics in Canada until the 1920s. At that time, Emily Murphy, a Winnipeg police magistrate and judge, wrote a series of articles on "the drug menace" (for Macleans Magazine) which were later expanded and published in a book entitled The Black Candle. Opium smokers were described as "ashey faced, half-witted droolers" with no more blood in their bodies "than a shrimp".166
Historically, the popular conception of the 'narcotics addict dope fiend' has established an image of the non-medical drug user which persists and intrudes into almost every examination or investigation of drug use today. Furthermore, the opiate narcotics have played an important role as a model in much of the past and present drug legislation and in the general criminolegal approach to the control of socially disapproved drug use. Although many important questions about the opiate narcotics are still unanswered, it is clear that much of what has commonly passed for fact is fiction.
Until recently, many observers did not consider the opiate narcotics to be the cause of a major public health problem in Canada. In the last few years, however, increasing attention has been given to reports of growing use of these drugs by young people both here and in the United States. (See Appendix C Extent and Patterns of Drug Use.)
MEDICAL USE
Most of the current medical uses for the opiate narcotics were fairly well understood and established in Europe by the middle of the 16th century and were probably well known in certain areas long before that time. These drugs are primarily used in the relief of suffering from pain, in the treatment of diarrhea and dysentery, and to reduce cough. They were also once commonly used as tranquilizers and antidepressants.113, 145, 218 Hundreds of related compounds have been synthesized in attempts to retain the clinical benefits but reduce the dependence liability of the opiate narcotics. These efforts to develop substitute drugs which do not produce dependence have not been very successful, and morphine and related compounds are still considered by physicians to be among the most valuable drugs available to the practitioner today. Heroin is rarely used medically in Canada, and no new stocks can be produced or imported.
A recent report from a World Health Organization scientific group concluded that the natural and semi-synthetic opiate narcotics are not indispensable in the practice of modern medicine, since wholly synthetic drugs are now available which are in many respects equivalent or superior to the natural compounds.236 However, none of the synthetic alternates are free from adverse effects, and the report did not suggest that the natural and semi-synthetic opiate narcotics be replaced at this time.
CHEMICAL ANALYSIS OF ILLICIT SAMPLES IN CANADA
Opium is uncommon in Canada, and only 42 samples were identified by police analysts during a 12-month period ending in March 1973.34 Methadone, morphine, codeine and pethidine are occasionally noted in seizure reports. These latter drugs are generally of high purity and are presumed to result from the diversion of legally produced materials.
A study of police seizures of heroin in 1959-60 indicated that the illicit heroin available in Canada was of surprisingly high quality.68 Ninetyfive per cent of the 229 seizures examined contained between 24 and 68 mg of heroin per capsule, with a mean of 46 mg. The mean purity of these samples was 53%. Lactose (milk sugar) had been used to dilute the heroin in almost all cases. Nine samples (4% ) also contained quinine. There were no other indications of deliberate adulteration or any unidentifiable substances.
The Comission has investigated the chemical properties of illicit heroin available in Canada in recent years.168, 177 In one study, 90 samples from 20 different police exhibits of heroin (seized between February 1968 and May 1970) were selected from the vaults of the Bureau of Dangerous Drugs and were analysed in the Health Protection Branch laboratories.177• (a], Ib] Material packaged in unit doses (capsules or envelopes) ranged in total weight from 9 mg to 143 mg with a median of 77 mg. The actual quantities of pure heroin in these units ranged from 0.6 mg to 94 mg with a median of 25.6 mg. The purity of these samples covered a range of 0.5% to 96% heroin, with a median of 35%. Although a few large seizures showed exceptional uniformity among capsules, considerable variation in heroin content within single bulk seizures was typical. For example, the content of 10 capsules selected randomly from a total of 60 seized in a single package varied between 21 mg and 62 mg of pure heroin. In another case, the content of five seemingly identical capsules from the same source ranged from 0.6 mg to 30 mg of heroin. In this study, in only one case was another drug (procaine) identified in the heroin samples. No quinine was reported. Non-drug materials (diluents) used to dilute or cut the heroin were not positively identified.
The Health Protection Branch of the Department of National Health and Welfare provided the Commission with data on 168 police seizures of heroin quantitatively analysed during the period of June 1971—October 1972.91 The results of these analyses are generally similar to those just presented. The actual heroin content per packaged unit dose ranged from 5.4 mg to 92.5 mg with a median of 33 mg, and the purity of bulk powder samples ranged from 1.4% to 100% heroin with a median of 25.6%. Many of these samples were selected for special analysis because of previously detected impurities and consequently cannot be considered representative. The purity of randomly selected samples might be significantly higher. Products of faulty or incomplete synthesis (such as monoacetylmorphine) were often found. A few mixtures of heroin with other non-opiate drugs, such as caffeine, methaqualone and MDA were identified, but such cases did not make up a significant proportion of the total number of police seizures. Quinine was found in only three instances. Non-drug diluents were not positively identified.
In the Commission's collection of illicit drug samples and survey of `street drug' analysis facilities in Canada (1971-72), 18 samples had been presented as heroin.159. [e] Of these, only nine contained any opiate narcotics. In addition, out of almost a thousand drug analyses reported, opiates were identified in only eleven cases where the substance had been unspecified or alleged to be another drug. No case of `opiated' hashish or marijuana, alleged to be pure, has ever been chemically documented in Canada in spite of the popular impression that this is an established combination. Samples presented as `opiated hash' or 'smack grass' have invariably been found to be relatively pure cannabis.
The data now available in Canada do not provide an adequate basis for clear statements regarding regional differences in illicit heroin or changes in the quality of the drug available in the past few years. It is clear that the purity of illicit heroin and the quantity of the drug packaged for consumption in the form of single capsules or bags varies over a considerable range. Adulteration of heroin with other drugs is apparently rare. The substance most often mentioned in reports of diluted or cut heroin is lactose. Quinine, a drug which was a common diluent in the U.S.,68• 76' 97 is rarely found in Canadian samples. It would appear that opiate narcotics are very rarely disguised or misrepresented as other drugs in Canada, although some of the materials sold as opiate narcotics on the illicit market may not contain any heroin or morphine.
ADMINISTRATION, ABSORPTION, DISTRIBUTION AND PHYSIOLOGICAL FATE
Opiate narcotics are produced in a variety of tablets and capsules, elixirs, cough syrups, ampules for injection, rectal suppositories and, on the illegal market, some are also available in a gummy, solid or powdered form. Codeine and some of the synthetics are often marketed in mixtures with non-opiate analgesics (e.g., APC&C, '222'®, Darvon®). While opiate narcotics may be readily absorbed from the gastrointestinal tract, in most instances this route is less effective and often erratic and unpredictable compared to injections. Among non-medical users, subcutaneous (`skin popping') and intravenous (`mainlining') injections are commonly used with heroin and morphine, and heroin powder is sometimes sniffed ( `snorted'). Raw opium is generally ingested or smoked. Methadone is commonly given orally in medical use, although it is also available in injectable form. Smoking heroin in a cigarette or pipe is very inefficient since the high temperature of combustion (approximately 750°C) causes extensive decomposition of the drug. However, with sufficient quantities of heroin, it is possible for physical dependence to develop from smoking. Less intense (sub-combustion) heating may release a fair amount of active material in fumes (e.g., 50-75%) which is well absorbed by inhalation, and such use of heroin has been reported in the Far East.89, 188 Intravenous injection of opiate narcotics produces the most rapid and intense effects. Oral administration generally results in a slower, milder, but longer lasting effect.
Only a minute fraction of the drug absorbed actually enters the central nervous system, its most important site of action. The actual mechanisms by which these drugs exert their effects are largely unknown. There is recent evidence that the primary "opiate receptor" in the central nervous system (CNS) is associated with acetylcholine.182
The duration and intensity of the effects are dose-related and vary considerably with the different drugs in this class; the duration of major action of the natural alkaloids may vary from two to six hours or more. The effects of methadone and some of the other synthetics may last many times longer. The opiate narcotics are usually inactivated or modified in the liver and excreted in the urine. Detectable amounts may also be present in saliva and sweat.
Heroin is rapidly metabolized in the body to 6-monoacetylmorphine and morphine, and likely exerts its effects indirectly, primarily as the morphine metabolites.228 Unchanged heroin apparently has little direct effect. Codeine is chiefly metabolized and excreted in the urine in the form of inactive metabolites, but at least a small fraction is transformed into morphine."3
DETECTION OF OPIATE NARCOTICS IN BODY FLUID AND TISSUE
A wide variety of standard techniques are available for the detection of opiate narcotics and their metabolites in body tissues and fluids.15, 45, 215
There has been considerable related research activity over the past few years, and significant progress has occurred in several areas.125, 162 Much attention has focussed on developing techniques for large-scale urine monitoring programs. Important advances in the detection of opiate narcotics in blood and saliva have also been reported. There is a clear need for convenient techniques for screening for a broad spectrum of drugs in methadone maintenance programs. Several automatic and semi-automatic systems are now commercially available which facilitate the rapid analysis of large numbers of urine samples.125
The general analytic methods most commonly used for the detection of opiate narcotics include: thin-layer chromatography (TLC), gas-liquid chromatography (GLC), spectrophotometry, immunoassay, and a variety of simple chemical and colour reaction tests. Some of these methods are useful for general qualitative identification only, while others can provide precise quantitative information as well. The relative value or appropriateness of these various techniques depends on the practical applications intended. Among the factors to be considered in evaluating such methods are: cost, convenience, speed, sensitivity, and specificity. Many of the available methods, if used alone, can be expected to produce a significant number of false positive or false negative indications. The importance of such errors depends, of course, on the application involved. By a combination of methods, under optimal conditions false reports in detecting recent opiate narcotic use can virtually be
eliminated.9, 56, 209
Gas-liquid chromatography (GLC) is very sensitive and precise, but is relatively slow and requires a high degree of specialized technical training. In addition, the equipment is expensive and delicate.
At the present time thin-layer chromatography (TLC) apparently provides the most practical general method for detecting a wide variety of drugs in urine.125, 126 Many TLC methods are available, all requiring the prior extraction of drugs from biological specimens before analysis. The sensitivity of TLC systems to opiate narcotics depends in part on the volume of the sample tested, and can be enhanced by pre-treatment (hydrolysis) of the material. Methods have been developed which employ preliminary extraction of drugs from the urine onto ion-exchange paper."' 125' 127 This simple step can be easily performed with a minimum of equipment and technical skill. Identification information can be written or typed directly onto the treated paper, which may be sent to a central laboratory for subsequent chemical analysis. Storage or transportation of urine is not necessary with these techniques. Furthermore, unanalysed papers can be conveniently stored for years, if desired, for possible later analysis. Papers can also be collected over a period of time and pooled for a single general analysis, thereby providing considerable savings in time and expense. Kaistha and Jaffe have recently presented a detailed analysis of the costs involved in a large-scale urine screening system employing ion-exchange paper and TLC.'"
Radioimmunoassay, spin immunoassay and other related antibody and enzyme techniques have recently been developed which allow the rapid detection and quantification of extremely low concentrations of various opiate narcotics in very small quantities of untreated urine, blood, saliva and per-
haps sweat.1, 86, 136, 197, 210, 211, 225 The spin-label method (also called the free
radical assay technique or FRAT) requires only a tiny drop (e.g., 20 microliters) of sample fluid, and can provide analysis within seconds. Such techniques have obvious application in assisting emergency diagnosis of drug overdose cases, for example. The FRAT system has received wide usage by the United States military to determine heroin use in Vietnam.111 EMIT (enzyme multiplied immunoassay technique) is comparable to FRAT in most respects but requires less expensive equipment.135, 197 Radioimmunoassay can provide greater sensitivity than the other immunoassay techniques, but is slightly slower. With the radio-label method, false positives in the general identification of opiate narcotics are minimal. With immunoassay techniques, the administration of a single dose of heroin or morphine may be detected in body fluids for several days after use.86. 212
Methadone does not interfere significantly with the immunoassay of natural opiate alkaloids, but codeine cannot presently be efficiently distinguished from morphine or heroin using these techniques. It may be possible to specifically identify codeine by a combination of other methods, however. It is generally not practical with available urinalysis methods to determine whether morphine or heroin were used. Immunoassay techniques are much simpler, faster and more sensitive on a sample-volume basis than TLC, but are less versatile. The range of different drugs which can be identified with immunoassay methods is presently limited compared to TLC, although antibody techniques for the detection of many other drugs are anticipated in the near future.
PSYCHOLOGICAL EFFECTS
The subjective psychological effects of opiate narcotics may vary considerably among different individuals and situations. The once popular notion that morphine-like effects are intrinsically so pleasurable that most persons who experience them are promptly addicted has not been scientifically documented. In one experiment, in which injections of morphine were given to 150 healthy male volunteers, only three were willing to allow repeated administration and none indicated that he would have actively sought more." Other researchers have also reported that the majority of normal pain-free individuals found the effects of opiates quite unpleasant.130, 2" In addition, many dependent users report that their initial experiences with opiate narcotics were not very enjoyable. On the other hand, numerous individuals report that they became infatuated with heroin on their first exposure to it and immediately decided to use it in the future as often as possible.
Even after some adaptation or tolerance develops, nausea and even vomiting frequently occur early in the 'high', especially after injections. This does not necessarily indicate dysphoria, however. Regular users report feelings of warmth, euphoria or well-being, peacefulness and contentment as a result of the drug. Drowsiness, dizziness, inability to concentrate, 'mental clouding', apathy and lethargy are also commonly noted. Certain individuals, especially when fatigued, may be stimulated into feelings of energy and strength. Higher doses produce a subjective turning inward and sleep. Often a pleasant dream-like state occurs. Some users describe their drug experiences in near ecstatic, and often sexual terms—especially the 'rush' of intravenous injection. Persons with a high degree of tolerance to opiate narcotics may experience relatively little euphoric response to the drugs; some heroin-dependent individuals claim that the drug merely helps them feel 'normal', rather than `high'.
The most prominent aspect of opiate narcotics, from a medical point of view, is their considerable analgesic or pain-relieving property. The potential of these drugs to relieve suffering from pain depends upon several mechanisms. The major effect is not on the sensation directly, but on the psychological reaction to it. Often individuals can still perceive the pain sensation and rate its intensity reliably, in spite of the fact that much or all of the negative or unpleasant aspects are absent. In other words, after the drug, a person may still feel the pain, but it does not bother him to the same extent. Morphine has little effect on the other senses and, unlike non-narcotic analgesics and sedatives, it can often control severe pain at doses which do not necessarily produce marked sedation, gross intoxication or major impairment of motor coordination, intellectual functions, emotional control or judgment.113 In addition to reducing the anxiety of pain and, therefore the motivation to avoid it, the opiate narcotics also tend to decrease other primary motivation associated with sex, food, and aggression.
The psychological effects of chronic opiate narcotic use are often rather straightforward extensions of the short-term response. In regular users, much of the variability and unpredictability of the immediate response is lessened, partly because individuals who find the experience unpleasant tend to avoid additional exposure, and also because many who were initially upset by the drug's unusual physiological and psychological effects learn to tolerate and even seek some of these sensations. The commonly experienced decrease in sex drive with chronic use is often a complicating factor in marital problems. While some individuals who become dependent on the opiate narcotics withdraw from regular social activities and live what appears to be an immoral, criminal and slovenly existence, others are able to lead an otherwise normal life with little change in work habits or ability to meet responsibilities. Possible factors underlying these differences will be discussed later.
Opiate narcotics typically do not disrupt psychomotor performance to any significant degree, although with higher doses there may be some impairment, possibly related to general sedation or motivational factors. 13, 73, 85, 208
Performance is likely to be significantly impaired during the early stage of withdrawal after regular use. It has been reported that persons dependent on heroin have poorer driving records than would be expected in the general population." However, other evidence indicates that heroin users may drive more extensively, and, if driving exposure is taken into account, they may actually have fewer accidents per unit distance driven.22
There is no evidence of permanent changes in cognitive or intellectual functioning due to chronic opiate narcotic use. Nor is there any indication of psychosis or other major psychiatric complications caused by these
drugs. 28, 107, 129, 174, 183, 213 In spite of the lack of serious psychiatric compli-
cations (other than dependence) caused by opiate narcotics, users of these drugs may be hospitalized in psychiatric institutions from time to time for treatment of their dependence.
In the Commission's national survey of psychiatric hospital diagnostic records in the spring of 1971, opiate narcotics were noted as factors in the primary or secondary diagnosis of 24 (0.1% ) of the 22,885 patients in the hospitals surveyed.98. [d] In British Columbia, psychiatric wards in general hospitals were surveyed as well, and in this population opiate narcotics were mentioned in the diagnostic records of 5 (1.7% ) of 293 resident patients. According to the mental health data provided to the Commission by Statistics Canada, 139 (0.25%) of the first admissions and 100 (0.20%) of the readmissions to psychiatric institutions or wards in Canada in 1971 were attributed to dependence on natural or synthetic opiate narcotics.122• [e] In these data, males outnumbered females by approximately two to one. (See also Tables A.5, A.6 and A.7 in the Annex to this appendix.)
PHYSIOLOGICAL EFFECTS
Pure opiate narcotics may produce few significant physiological effects in low therapeutic doses, although they affect, to a minor degree, practically all systems of the body. The immediate or short-term physiological response usually includes a general reduction in breathing and cardiovascular activity, a depression of the cough reflex, a constriction of the pupil of the eye and a minor reduction in visual acuity, a small change in some hormone levels, increased biliary pressure, itching of the skin, dilation of superficial blood vessels and warming of the skin, increased perspiration, a decrease in gastrointestinal activity (which typically causes constipation), nausea and sometimes vomiting. Sleep disturbances may occur in some individuals. In higher doses, insensibility and unconsciousness result. The primary toxic overdose symptoms are coma, shock and, ultimately, respiratory arrest and death.
There appears to be little direct permanent physiological damage from chronic use of pure opiate narcotics.7, 10, 26, 112, 213 Major complaints centre around persistent constipation and reduced sexual performance during chronic use. Numerous complications are observed, however, if the overall drug use pattern involves adulterated or diluted street samples, unsterile and shared needles, unhygenic living standards, poor eating habits and inadequate general medical care—all of which are commonly part of the behaviour syndrome of criminalized users. Commonly reported disorders in illicit users are hepatitis, tetanus, numerous cardiovascular and lung abnormalities, scarred veins (`track marks'), local skin infections, ulcers and abscesses, changes in muscle tissue, and obstetrical problems in pregnant females. Serious lung damage, possibly resulting in death, may be caused by intravenous injection of colloidal or partly soluble contaminants—often substances used to dilute or 'cut' illicit heroin, or the chalk or talc commonly found in licitly manufactured drugs (such as methadone) designed for oral use rather than injection. Although users often heat, or "cook" their drugs to increase solubility, and subsequently filter the drug through a wad of cotton to remove major particles prior to injection, this procedure is only partially effective, and may, in fact, introduce other contaminating materials, such as cotton fibres.42 There is some evidence of opiate narcotic alteration in gonadal tissue and function, although gross changes in 'sex hormone' levels apparently do not occur. Tuberculosis, pneumonia and venereal disease are more common among dependent users than in the general population.42, 143, 191, 198 Since similar problems have been reported in England where pure drugs are available for intravenous self-injection, contamination or adulteration of street drugs must be considered only part of the overall problem."
In the 1930s and 40s malaria, transmitted by unsterile needles, was a frequent correlate of opiate narcotic dependence in North America.95 For several decades later, no such drug-related malaria deaths were reported.9. 9T In the past few years, however, malaria has again appeared on the scene in California. Quinine, which was once commonly used to cut or dilute illicit heroin in the United States (especially on the East Coast), has some therapeutic effects in connection with this parasitic disease and may have been, at least in part, responsible for the decline in malaria cases.9• 97 On the other hand, quinine may increase the likelihood of tetanus after subcutaneous injection.'"
ACUTE TOXIC REACTIONS AND DEATH
The mortality rate among persons dependent on opiate narcotics is considerably higher than that of individuals of similar age in the general population. Although considerable variability exists among reports, it has frequently been estimated that in the United States, over 1% of the heroin-dependent population dies each year.7, 83. 143' 176, 203 Generally similar estimates can be derived from available Canadian data,101. 158 and somewhat higher figures have been reported in England.", 129 In addition to deaths resulting directly from the use of various drugs (representing the majority of the fatalities), a disproportionately high number of heroin users die from violent causes (including murder, suicide and various accidents) and, as discussed above, from numerous infections and diseases. Henderson's101 report of heroin-related fatalities in British Columbia presents a remarkably similar picture to that described in New York by Helpern and Rho.97
There is likely significant underreporting of opiate narcotic- and other drug-related deaths for a variety of reasons.6, 97' 205 To begin with, autopsy, with full toxicological analysis, is not conducted in a large proportion of deaths, and other relevant information as to drug use habits of the deceased is frequently unavailable or not actively sought.", 758' 217 Furthermore, there is often considerable reluctance on the part of examining physicians to attribute fatalities to drug use, especially in ambiguous cases. Variations in the numbers of drug death reports from location to location, or from year to year, may represent differences in the examiners' sophistication, and in the interest in and attention paid to possible drug-related cases, as well as differences in extent and patterns of drug use. As effort and sophistication increases, we can expect a corresponding increase in the accuracy (and often the frequency) of drug-related death reports.
The Commission has investigated reports of opiate narcotic-related toxic reactions and fatalities in Canada in considerable detail.", 158 Some of the findings are presented below.
The Federal Poison Control Program has records of over one thousand "narcotics" poisonings or adverse reactions (non-fatal and fatal) for 1971.169, [b] More than three-quarters of these involved pharmaceutical preparations of codeine and acetylsalicylic acid (A.S.A.), such as `222'0. The relative importance of A.S.A. and codeine in these later cases is unclear. (A.S.A. preparations [e.g., Aspirin®] alone account for more poisonings annually than any other drugs.) The A.S.A.-codeine poisoning rate in the population was highest for children under 5 years of age. More than one-third of the cases involved persons 10-25 years of age. There were reports of 179 Darvon® (propoxyphene, typically with A.S.A. and other drugs), 162 heroin, 21 methadone and 19 Demerol® (meperidine or pethidine) toxic reactions. Almost three-quarters of the heroin and methadone cases were males; for all other drug categories, women substantially outnumbered men. A little over one-half of the heroin and methadone cases were 10-24 years of age. Thirty-two deaths were reported which involved natural or synthetic opiate narcotics; 11 of these reports noted Darvon® or propoxyphene, 8 heroin or morphine, 5 methadone, and 4 codeine with A.S.A. and/or other drugs. The persons who died ranged in age from 17-64 years with a median of 28; none of the fatalities involved children.
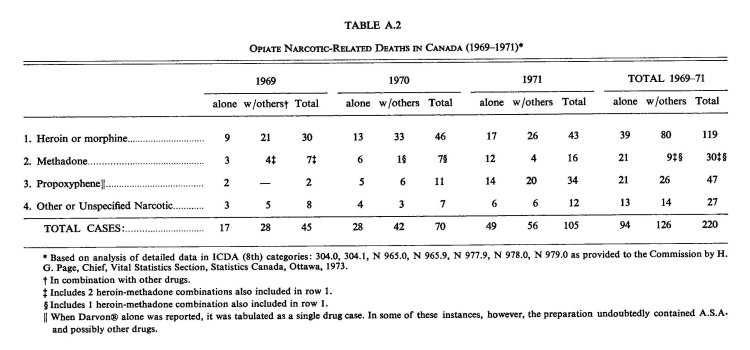
In the official Causes of death reports provided by the Federal Government, opiate narcotic deaths may be coded under a variety of categories." Since it is not possible to identify specific drugs in the published data, a detailed analysis of the federal death records was conducted for 19691971.158, 179 As shown in Table A.2, there has been a substantial increase in the opiate narcotic-related deaths reported during the three-year period. The greatest change occurred in propoxyphene-related fatalities; these cases are significantly different from the others in that the majority of the propoxyphene deaths were attributed to suicide and most involved women. Most of the other deaths were coded as accidental fatal drug reactions, primarily in men. Quite uniformly from year to year, about two-thirds of the reports included mention of more than one drug. Alcohol, barbiturates and A.S.A. were most frequently noted in combination with opiate narcotics.[ni]
The Commission has been informed by the Supervising Coroner's office of Vancouver that 37 opiate narcotic-associated deaths occurred in that city in 1971 and 65 occurred in 1972.158 Heroin (or morphine) was involved in 78% and 91% of the fatalities in those years respectively. During the two-year period, there were also 6 methadone-, 2 codeine- and 7 propoxyphenerelated deaths. Approximately three-quarters of the fatalities involved other drugs as well, with alcohol and barbiturates most frequently mentioned. Three-quarters of the deceased were males. The Coroner's Office of Ontario provided the Commission with detailed information on nine opiate narcotic-related fatalities occurring in 1972, of which seven cases also involved other drugs. Six reports noted heroin or morphine. These data are not significantly different from those reported for Ontario in 1970 and 1971.158 In the Commission's survey of coroners' records, of a series of 92 heroin-related deaths (occurring in 1969-1971) approximately three-quarters included mention of other drugs as well."' [g] In only eight cases was death ascribed to heroin or morphine overdose alone. It would appear that deaths due to heroin alone are quite infrequent in Canada; most of the fatalities involve drug combinations.
The precise mechanism of death in the majority of the acute fatal reactions to opiate narcotics in North America is uncertain. Simple pharmacological overdose of morphine is usually characterized by stupor, coma, shock and, finally with sufficient dose, death due to respiratory failure—a process which typically occurs over several hours.113, 1" Such poisoning is easily and rapidly reversed by the administration of a morphine antagonist such as nalorphine, and is rarely fatal if appropriate treatment is administered. If other drugs are also present (as is usually the case) a fatal reaction may be potentiated and effective treatment made much more difficult. (Drug interaction is discussed in more detail below.) Deaths resulting directly from the administration of opiate narcotics, on autopsy, are typically characterized by a profound pulmonary edema (swelling and fluid in the lungs), often producing a bubbly froth in the mouth and nose, with little cardiovascular change."' 61, 77' 97' 143, 205
Fatalities are frequently attributed to unpredictable variations in the strength of illicit heroin and in changes in the tolerance of users from time to time."' 97' 139' 143' 152 In several reports, death occurred soon after release from hospital or prison when the user's tolerance was low due to abstinence. Regular opiate narcotic users with high tolerance are remarkably resistant to pharmacological overdose effects,20, 138 although fatal acute reactions are reported in such individuals. While variations in tolerance and in the strength of illicit heroin likely play a role in certain fatalities, much evidence indicates that other factors are typically involved.
In most parts of North America simple opiate narcotic overdose death is apparently rare. More frequently reported is a rapid toxic reaction to the intravenous injection of an illicit heroin-containing mixture, which in some instances may result in death within minutes. In some cases, fatal reaction is so sudden that the injection needle may still be in the user's arm or hand when the death is discovered. The role of various potential factors in such unexpected and apparently unpredictable fatalities is uncertain and has recently become the subject of some controversy.26, 27, 96 It appears that such cases do not result from simple pharmacological overdose, although they are often recorded as such in official statistics.8, 43. 97 In some cases where samples of the material injected were available for analysis—either other 'caps' or 'bags', or drugs remaining in the syringe—no evidence was found of unusual heroin concentration. A sudden fatal reaction may occur to a dose which was apparently comparable to one readily tolerated the day before. As well, users often take drugs from the same batch together in groups, but very rarely does more than a single individual suffer a severe toxic reaction.97
Helpem and Rho observed in New York:
The toxicological examination of the tissues in such [sudden shock-like] fatalities, where the reaction was so rapid that the syringe and needle were still in the vein of the victim when the body was found, demonstrated only the presence of alkaloid, not overdosage.... Thus, there does not appear to be any qualitative correlation between the acute fulminating lethal effect and the amount of heroin taken .
There is some suggestion that an allergic or general hypersensitivity reaction to heroin or some contaminant might be involved in the sudden death phenomenon. Fatal allergic or other idiosyncratic reaction to intravenous injection of various materials may occur on rare occasion even under medical conditions. However, the condition seen with illicit heroin is not the same as that in fatal anaphylactic reaction to penicillin, for example.? If general non-opiate factors were typically responsible for the sudden deaths, one might expect to see a similar fatal syndrome associated with the intravenous use of other illicit drugs such as methamphetamine and barbiturates as well. As discussed in A.3 Amphetamines and Amphetamine-like Drugs and A.7 Barbiturates, comparable reactions with these other drugs are not reported. Very few fatal acute reactions to amphetamine injection have been documented, and barbiturate fatalities usually occur after prolonged coma. The edema and damage to the lungs typically reported with heroin fatalities may result in part from hypoxia due to impaired respiration;91 other drugs, such as barbiturates, which also depress breathing may produce a similar but not identical lung condition.43
It has been suggested that quinine, which is frequently found in New York heroin, might play a significant role in fatal drug reactions; overdose of quinine alone can produce rapid severe pulmonary edema and death.26 As well, it was shown in a rodent study that quinine can add to the lethal toxicity of heroin.184 However, quinine cannot provide the complete answer since the "narcotic lung" syndrome has also been reported in Canada,99 England, 18, 120 and the Far East,75 where quinine is rarely found in heroin. Furthermore, pulmonary edema as a characteristic of opiate poisoning was reported in the North American literature before the appearance of quinine in illicit market heroin. Apparently, the first report of opium-related pulmonary edema was published by Osier in 1880 in the Montreal General Hospital Reports.178
As noted earlier, the general mortality rate among heroin users in England 18, 77, 120 is reportedly as high or higher than that in North American users, although only limited comparisons of data from different reporting systems can be made. In any event, there is no evidence that the availability in England of pharmaceutical heroin preparations of known strength and purity has been associated with a reduction in the incidence of opiate narcotic-related fatalities among users. The various factors in these deaths have not been fully explored, but it would appear that other drugs are typically involved as well, and that uncomplicated fatal heroin overdose is not common in England.
Rapid fatal reaction to opiate narcotics would be difficult to study experimentally since, even though the phenomenon accounts for a large proportion of heroin deaths in North America, it is actually a rather rare occurrence. For example, Baden has estimated that death due directly to illicit heroin injection occurs only once in 100,000 administrations in New York.8
Further study of the significance of other drugs in opiate narcotic-related death is clearly indicated. While it is well known that many drugs may enhance the toxicity of opiate narcotic overdose, the role of drug interaction in the sudden heroin-death syndrome has not been adequately explored. On balance, there would appear to be some opiate-specific factor involved in the bulk of the heroin-related deaths, although the precise pharmacological mechanisms involved, and their possible interactions with other drug and non-drug variables are uncertain.
TOLERANCE AND DEPENDENCE
General tolerance to morphine and related substances develops readily; it develops more rapidly if the interval between doses is less than the duration of action, so that effective concentrations of the drug are continuously present in the tissues, and more rapidly still when large quantities are used. When tolerance has developed there is cross-tolerance to other drugs with similar pharmacological action. Tolerance does not develop with equal rapidity, nor to the same degree for all effects. The disagreeable side effects of nausea, vomiting, and dizziness usually decline early; tolerance to the analgesic and euphoric action (and the initial 'rush') may develop rapidly; and tolerance to the sedative and respiratory depressant effects usually develops most rapidly of all. In contrast, tolerance to the effect on the pupil and the gastrointestinal tract develops slowly and to a more limited degree, so that the miotic or `pin-point' pupil and constipation persist. As well, little tolerance seems to develop to the depressant effects on sexual activity. Since a great risk in opiate narcotic overdosage is respiratory depression and failure, tolerance to this effect permits the person, as a rule, to withstand many times the
amount of drug which would normally be fata1.103. 112, 113, 148,164, 200
The tendency to increase dose depends in part on which of these various effects reward or reinforce the use of the drug. Persons who are motivated by the avoidance of chronic pain or other unpleasant psychological conditions, or perhaps simply by the pleasurable, euphoric aspects of these drugs are most likely to increase dose to retain these effects after tolerance develops. Ever-increasing quantities are not inevitable, however, even in regular users, and many persons with morphine-type dependence successfully maintain use at intermediate doses for indefinite periods of time. If use is intermittent, of the 'chipping' or 'spree' variety, minimal tolerance develops and there may be little need or tendency to increase dose. Although other factors may be involved, the primary mechanism of tolerance seems to be a general reduction in the sensitivity of the nervous system to opiate narcotics.103, 118
Tolerance begins to disappear with cessation of use, but its rate of elimination, as with its acquisition, varies with the different effects, and for some it is very slow. Probably the sensitivity of the respiratory centre to the depressant action of morphine is most easily regained, and some deaths have reportedly occurred because persons have attempted to take, after withdrawal, doses to which they had been previously tolerant. Recovery of analgesic and sedative responses are slow, and some metabolic changes persist long into abstinence.103, 137, 148, 150
Opiate narcotics may produce considerable psychological and physical dependence. The relationship between tolerance and physical dependence has been the subject of much discussion, but is not yet resolved satisfactorily. For the most part, however, they seem to develop together in parallel fashion and may reflect common physiological mechanisms. There is some evidence that the mechanism may be set in operation with the very first dose. However, if the amount of drug used is small and it is taken infrequently, no significant signs of dependence normally occur.4° The degree of physical dependence, as reflected in the intensity of the withdrawal syndrome, is determined by the quantity, frequency and duration of use, as well as the specific drugs and individuals involved.
The abstinence syndrome which follows withdrawal of any one of the opiate narcotics is a specific, characteristic and self-limiting illness, the onset, peak and duration of which vary with the actual agent involved. With low dose or intermittent use, withdrawal symptoms may be negligible or perhaps resemble the symptoms of flu. This is the pattern most often seen in Canada today. Withdrawal of the drug after heavy chronic use results in a severe and painful pattern of effects which resembles in certain ways that associated with alcohol and barbiturate withdrawal. There are, however, significant differences between the morphine-like drugs and the alcohol-barbiturate type drugs in this regard.112, 200
The 'classical' severe heroin withdrawal syndrome was described several decades ago as follows:
As the time approaches for what would have been the addict's next administration of the drug, one notices that he glances frequently in the direction of the clock and manifests a certain degree of restlessness. If the administration is omitted, he begins to move about in a rather aimless way, failing to remain in one position long.... With this restlessness, yawning soon appears, which becomes more and more violent. At the end of a period of about eight hours, restlessness becomes marked. He will throw himself onto a bed, curl up and wrap the blankets tightly around his shoulders, sometimes burying his head in the pillows. For a few minutes he will toss from side to side, and then suddenly jump out of the bed and start to walk back and forth, head bowed, shoulders stooping. This lasts only a few minutes. He may then lie on the floor close to the radiator, trying to keep warm. Even here he is not contented, and he either resumes his pacing about, or again throws himself onto the bed, wrapping himself under heavy blankets. At the same time he complains bitterly of suffering with cold and then hot flashes, but mostly chills. He breathes like a person who is cold, in short, jerky, powerful respirations. His skin shows the characteristic pilomotor activity well known to those persons as "cold turkey". The similarity of the skin at this stage to that of a plucked turkey is striking.... Often at the end of this period the addict may become extremely drowsy and unable to keep his eyes open. If he falls asleep, which is often the case, he falls into a deep slumber well known as the "yen" sleep.... The sleep may last for as long as eight or twelve hours. On awakening, he is more restless than ever.... Usually as this stage, the addict complains of cramps, locating them most frequently in the abdomen, but often in the back and lower extremities.... Vomiting and diarrhea appear.... Perspiration is excessive. The underwear and pajamas may become saturated with sweat. Muscular twitchings are commonly present; they may occur anywhere, but are most violent in the lower extremities.... If he is handed a cigarette to smoke, his hands tremble so violently that he may have difficulty in placing it in his mouth. . . . It is at this stage that he may one minute beg for a "shot" and the next minute threaten physical violence (to get it)....
The readministration of the drug promptly brings about a dramatic change. The patient becomes exceedingly docile almost with the puncture of the hypodermic needle. In a few minutes he begins to feel warm, and the goose flesh and perspiration are no longer visible.... In a period ranging from thirty minutes to one hour the tremors disappear. He has become strong and well. He no longer walks with bowed head and stooped shoulders. He stands erect, is quite cheerful, and lights his cigarette like any normal person. He becomes profuse in his apologies for his conduct during the abrupt withdrawal of the drug.'
With morphine or heroin, the withdrawal syndrome usually appears 6-12 hours after the last administration, peaks at about 26-72 hours, and gross recovery usually occurs within about a week, although complete recuperation may take up to six months or longer.103, 137, 148, 150 With methadone, the symptoms are qualitatively similar, but at equivalent doses are generally less severe, develop more slowly and are more prolonged. The syndrome seen in chronic users of some of the other analgesics (e.g., codeine and propoxyphene) and in opium smokers is generally milder than with the more potent compounds.
The classical, severe opiate narcotic withdrawal syndrome described above seems to be the exception rather than the rule; much milder, flu-like symptoms are typically described by clinicians and the drug users themselves. This may be due to the relatively low purity of street heroin in some areas, and to the light and intermittent use patterns which have developed, but more likely reflects an overemphasis of extreme cases in the earlier literature.
The chronic use of heroin by pregnant women may result in a variety of obstetrical complications.20, 21, 51, 74, 80, 93, 214, 227, 240 Babies born to mothers who are dependent on heroin may also be physically dependent.
Some infants may require special medical attention for several weeks following delivery, although others show no obvious withdrawal symptoms or other difficulties. Many of these infants also have low birth weights, but it is not established if this is due to the opiate narcotic or to other factors such as poor nutrition, inadequate hygiene, or the use of other drugs such as tobacco. Babies born to mothers stabilized on methadone during pregnancy also tend to have lower birth weights and to demonstrate withdrawal symptoms, and there is currently some controversy regarding whether it is obstetrically superior for the mother to continue using heroin or to change to medically administered methadone prior to delivery. Supplying the pregnant women with methadone gives the physician a much better understanding of her drug history and also increases the opportunity for prenatal care. On the other hand, the methadone could result in a much stronger physical dependence than had been the case with heroin, and consequently the infant's withdrawal may be more severe. (This latter factor is discussed in more detail below.)
Considerable cross-dependence exists among the opiate narcotics, and an intravenous injection of any of these drugs can, in sufficient dose, substantially reduce or eliminate the withdrawal syndrome in a matter of minutes. Methadone, for example, can prevent withdrawal symptoms and reduce the craving for morphine or heroin in doses which often provide relatively few other psychological effects. In addition, large doses of methadone or other narcotics administered chronically can, by cross-tolerance, block or reduce the euphoriant effects of heroin. These qualities are commonly made use of in the treatment of severe withdrawal and in methadone maintenance programs. Although the sedatives and the opiate narcotics do not show significant cross-tolerance or cross-dependence, barbiturates and minor tranquilizers may, in some way, mask or ease the discomfort and restlessness of opiate withdrawal.
The direct injection of a specific opiate antagonist (e.g., nalorphine) will block nearly all morphine-like effects and cause the almost immediate appearance of an exaggerated form of the abstinence syndrome in dependent persons. Such drugs have been used to 'test' for dependence in suspected drug users.113 Antagonists are discussed in more detail in a separate section below.
The relative importance of physical and psychological dependence in the overall picture of chronic opiate narcotic use has been the subject of much controversy. Some investigators argue that the fear of the withdrawal syndrome is often the primary motivating factor behind continued use, while other observers emphasize the strong craving often described even after long periods of abstinence, or the drug's positive reinforcing effects or reward potential. Most dependent persons return to the drug at some time after withdrawal, and some have been known to voluntarily undergo withdrawal in order to lose tolerance and initiate chronic use again, at a lower, more manageable and less expensive level. In addition, there seems to be no relationship between the severity of the abstinence syndrome experienced and the tendency to relapse to chronic use again. These observations suggest that, with most individuals, factors other than mere avoidance of the acute abstinence syndrome are dominant in the overall drug dependence picture. Whether this motivation is related to the desire to escape or avoid a life situation which is unpleasant, emotionally painful, depressing or frustrating, or perhaps a more direct hedonistic desire for pleasure or `kicks', or a disguised attempt at self-destruction, or still other factors is not clear. No simple answer could be expected to have much generality or validity.
There is growing evidence that a significant conditioning or learning component is involved in physical dependence and the withdrawal syndrome.160, 232, 235 Stimuli which are associated with the withdrawal syndrome in dependent subjects can gain the power to produce some signs of withdrawal when presented alone. Furthermore, a stimulus which has been associated with the administration of an opiate narcotic may temporarily reduce the severity of withdrawal symptoms. Drug-dependent persons often report some feelings of relief from withdrawal as they insert a hypodermic needle, even before the drug is injected. Subjective symptoms somewhat like those experienced during acute withdrawal may be elicited by a variety of familiar stimuli in former users, even after considerable periods of abstinence. Talking about heroin, the smell of a burning match previously associated with "cooking up" an injection, or simply seeing physical surroundings and persons who were involved in one's previous drug use may elicit some craving or withdrawal-like discomfort.144, 213, 230
It has frequently been observed that some individuals develop a dependence on the hypodermic needle (or 'point') which becomes, in some respects, independent of the pharmacological properties of the drug. Persons showing such conditioning are often called 'needle freaks'.
Dole and Nyswander contend that the repeated use of opiate narcotics produce a chemically based "narcotic hunger" which may last indefinitely.59 In other words, once an individual has become accustomed to the effects of these drugs he is no longer able to function normally in their absence. Anxiety, depression and a craving for the drug may persist and interfere with previously normal behaviour. Some investigators feel that the chronic administration of an opiate narcotic is necessary for these individuals, and that such a condition is, in some respects, analogous to the dependence of a diabetic on insulin. This is one of the rationales often presented for opiate narcotic (e.g., heroin or methadone) maintenance programs.
Numerous studies have been conducted in recent years employing brain lesion, electrophysiological stimulation and recording, and pharmacological techniques in animals, to determine the areas of primary CNS action of opiate narcotics. Experimentally induced changes in opiate narcotic self-administration, tolerance, physical dependence and other effects have been reported; but much of the literature is not consistent, and con-
siderable additional research in this area is needed. 3, 71, 110, 128, 182, 187, 219, 232
Although it appears that only a fraction of the persons who have experimented with opiate narcotics actually become dependent, once a serious dependence problem develops, there is little evidence that conventional legal or medical treatment is successful in breaking the recurring relapse cycle. Many observers contend that certain social and personality factors predispose some individuals to drug dependence and that normal individuals rarely, if ever, become chronically dependent. There is considerable evidence that both the ready availability of the drug and a social milieu tolerating or encouraging drug use (either medical or non-medical) are generally more important factors. Although there are numerous individuals who have gradually worked up from occasional 'skin popping' to chronic 'mainline' dependence, there is evidence that some users are able to maintain an intermittent pattern of use.
There have been a number of popular misconceptions about the pattern of development of opiate narcotic dependence. Rumours have frequently been heard that marijuana and hashish have been 'spiked' with heroin to produce opiate addiction in the unsuspecting user. Similar rumours have been heard about 'spiked' LSD. As noted above, however, available evidence in Canada suggests that opiate narcotic adulteration of other drugs alleged to be pure is very rare or non-existent. It would be highly unlikely, if not impossible, for tolerance and dependence to develop in such a situation without the user knowing it. The majority of users, both here and in the United States, were apparently first 'turned on' by their friends and peers. Blum (in the 1967 United States Task Force Report) points out:
There is no evidence from any study, of initiation as a consequence of aggressive peddling to innocents who are 'hooked' against their will or knowledge. . . . The popular image of the fiendish peddlar seducing the innocent child is wholly false.'
Some of these topics are discussed in more detail in Appendix C Extent and Patterns of Drug Use and Appendix D Motivation and Other Factors Related to Non-Medical Drug Use.
OPIATE NARCOTICS AND CRIME
A consensus seems to exist among medical, law enforcement and research authorities, as well as drug users themselves, that few if any crimes of violence
result directly from the use of the opiate narcotics.23, 28, 40, 101, 112, 124, 183, 165, 176' 196, 213 On the other hand, there is a considerable relationship between crime and opiate narcotic dependence in North America, and many persons dependent on illicit drugs have non-drug criminal records. This apparent paradox can be explained by two important factors. To begin with, both in Canada and in the United States, the majority of the individuals studied who became dependent on illicit opiate narcotics had a prior history of behavioural problems and delinquency, and many appear to have continued these practices. The second factor is economic and is associated with the illegality of heroin and its consequent high cost on the illicit market, and the demands made by extended tolerance and dependence.
Because of the illegal nature of the drug, the cost of a heavy heroin habit may run anywhere from $15.00 to $50.00 a day and higher, in spite of the fact that the medical cost of the drugs involved would just be a few cents. There are very few legitimate ways in which most individuals can afford to meet illicit market prices. Consequently, when tolerance pushes the cost of drug use above what the user can afford legitimately, he is forced into a decision—either quit the drug and go through withdrawal, or turn to criminal methods of acquiring the necessary money. While some users refuse to become involved in criminal activities and consequently stop using the drug, at least temporarily, many turn to petty crime, small robberies, shoplifting and prostitution. These are the individuals who regularly come to the attention of the law enforcement officials. More affluent persons may be able to support the habit and continue indefinitely without running afoul of the law. Medical profession dependents, for example, apparently have less tendency to commit non-drug offences--perhaps (in addition to predisposing psychological and sociological factors) because they can often steal the drugs with little risk or purchase them at low cost.
As Jaffe has stated:
The popular notions that the morphine addict is necessarily a cunning, cringing, malicious and degenerate criminal who is shabbily dressed, physically ill, and devoid of the social amenities could not be farther from the truth. The addict who is able to obtain an adequate supply of drugs through legitimate channels and has adequate funds usually dresses properly, maintains his nutrition, and is able to discharge his social and occupational obligations with reasonable efficiency. He usually remains in good health, suffers little inconvenience, and is, in general, difficult to distinguish from other per-
OPIATE NARCOTICS AND OTHER DRUGS
Pharmacological Interaction
Although numerous psychotropic drugs are frequently used both medically and non-medically in combination with opiate narcotics, research into the possible psychological and physiological interaction involved in such combinations has been surprisingly limited. Existing evidence suggests that opiate narcotics taken together with alcohol or barbiturates can result in greater sedation and toxicity (including death) than that produced by either drug alone, but more studies are needed.52, 65, 66, 168, 226 The interaction of alcohol and methadone may be of considerable social significance. Other drugs which can produce significant sedation, such as certain non-barbiturate sedatives, minor tranquilizers, antihistamines, and belladonna alkaloids, may add to the depressant effects of opiate narcotics. There are many other questions which require attention; for example, more information is needed regarding the effects that such drug combinations have on psychomotor skills, risk taking, and other functions involved in automobile driving and accidents.
The interactions between opiate narcotics and stimulants such as caffeine, amphetamines and cocaine are also poorly understood and complex. Caffeine and amphetamines are sometimes used medically to counteract the respiratory depressant action of opiate narcotics in cases of overdose.193, Combinations of opiate narcotics and amphetamines may be antagonistic on some effects but show no interaction on others, and may have additive effects on certain subjective measures.122 It has been reported that amphetamines may enhance the pain-relieving and anti-depressant properties of opiate narcotics when the two are administered together.67, 133 Cocaine or amphetamines are sometimes mixed with heroin as a `speedball' for non-medical use. In some cases, opiate narcotics are illicitly used to reduce the severity of unpleasant symptoms following chronic, high-dose intravenous amphetamine use. Low doses of cocaine administered to mice are reported to reduce the lethality of high doses of heroin, although high doses of cocaine appear to increase the toxicity of heroin in this species. It was also shown in the same study that quinine, which is sometimes used to cut or dilute heroin, particularly in the United States, adds to the lethal toxicity of heroin.184 Further investigation of the combined toxicity of these compounds should be conducted in primates.
There has been almost no controlled research on the interaction of cannabis and opiate narcotics. There are reports that cannabinoids may ease the discomfort of heroin withdrawal or craving even though no significant cross-tolerance or cross-dependence apparently exists between these two classes of drugs.102, 154, 167, 241 There has been speculation that even though cannabis itself has exceptionally low lethal toxicity, high doses taken concomitantly with opiate narcotics might increase the likelihood of toxic overdose with the latter drugs. Cannabis has been shown to enhance the toxicity of morphine overdose in animals," but no human data is available.
Progression to Heroin from Cannabis and Other Drugs
In the past two decades, the relationship between cannabis and heroin has been the subject of heated controversy in Western literature. During this period, reports from the United States indicated that the majority of heroin users studied had previously used cannabis, although in certain sections of the country (noticeably the southeastern states) this was not the case.11 Before 1950, there was little evidence or serious discussion of a cannabisto-heroin progression in North America.
Alcoholism seems to be the most frequent form of serious drug dependence regularly associated with opiate narcotic dependence 6, 12, 176, 194, 224 although heavy use of tobacco and barbiturates is also common 50, 92, 161 Until recently, there appeared to be no relationship between the use of cannabis and heroin in Canada. Heroin users studied had generally been heavy consumers of alcohol, barbiturates, and tobacco, but had little or no cannabis experience.101, 124, 181, 213, 233 The situation has apparently changed and many young Canadian heroin users also report previous and concomitant use of marijuana, amphetamines, barbiturate and non-barbiturate sedatives and, less often, LSD.87, 123 Alcohol remains a major problem in North American heroin users, however; the incidence of alcoholism is extremely high in former heroin users, and is a common complicating factor in methadone maintenance programs.°
Several U.S. studies of persons arrested for cannabis offences, or noted for other delinquent behaviour, indicate that a significant number of these individuals were later arrested on heroin offences.32, 79,185 In some instances, however, the critical contact with heroin users and sources came from a prison experience.'" Robins reported that one-fifth of a group of blacks in St. Louis who were users of cannabis in the 1940s had admitted to subsequent heroin use.'"
Paton used a Bayesian formula employing various estimates of the incidence of cannabis and heroin use in the general population and in the sub-population of heroin users in England to predict that 7-15% of cannabis users will try heroin.'" The appropriateness and accuracy of the figures used in the formula and their applicability to the present situation are highly questionable. The proper use of Bayes' Theorem in this application requires accurate estimates of the incidence of drug use in the various populations described, at a single point in time. Good epidemiological data meeting these criteria were not available in England, and some researchers have suggested that if other, apparently equally justifiable, estimates had been employed, rather than those used by Paton, the resulting prediction of heroin use among cannabis users would have been substantially lower.88, 199 In any event, even estimates derived from the proper use of the statistical formula can be considered valid only as long as the social and epidemiological conditions associated with the use of both drugs remain constant. These requirements call into question the general value of Bayes' Theorem in those areas of science dealing with rapidly changing social phenomena.
Studies based on lower-class and/or delinquent populations do not readily generalize to the present phenomenon of middle-class cannabis consumption. It would appear that only a small minority of middle-class cannabis users have had experience with opium, morphine or heroin. However, some opiate narcotic use in certain middle-class groups in Canada has been reported.
Due to loose prescribing practices and the availability of methadone on the illicit market, a number of "primary methadone addicts" (without previous heroin experience) have developed in Canada. Some of these individuals have subsequently tried heroin as well. The extent of such occurrences is uncertain at the present time.
In North American studies, peer groups values and the establishment of contacts with illicit drug distribution networks have played a major role in concomitant and sequential illegal use of different drugs. Becoming accustomed to "breaking the barrier" of illegal drug use by the consumption of one illicit drug may reduce, in some individuals, inhibitions with respect to other such drugs. It has been proposed that cannabis often provides the initial drug in this context. Although previous heavy illicit use of alcohol during adolescence is common in adult chronic drug users, drinking by young people, even though illegal, is largely condoned and, to some extent, encouraged by our society; it does not have the legal significance that cannabis use has. Some have suggested that through the use of cannabis certain, perhaps predisposed, individuals may learn to use a drug as a mode of coping or as a simple primary source of reinforcement and satisfaction, and that this lesson might later generalize to other drugs. In some instances, heroin was first taken by intravenous amphetamine users to 'crash' or come down from a 'speed run'. Much attention has been given to the concept of a "needle barrier" in such cases. It has been suggested that learning to tolerate (or in some cases, to enjoy) the originally aversive practice of self-injection increases the likelihood that other drugs will be injected at a later time. Many argue that persons who ultimately become dependent on opiate narcotics, 'speed' or other 'hard' drugs are strongly predisposed in that direction by personal, social and economic factors, and that the use of transitional drugs is of little causal significance. Attempts to identify and establish personal predisposing factors have met with little success, however, and this interesting hypothesis has yet to be confirmed.
In summary, a positive statistical relationship exists between the use of heroin and a variety of other psychoactive drugs. Marijuana is often the first illicit drug (other than alcohol and tobacco in adolescence) taken by users of heroin and other drugs. The role of cannabis, if any, in the progression to other drugs is not yet well understood; it is unclear whether it plays a specific predisposing role, or is causally unrelated to other drug use and is typically used earlier simply because of its wider availability and social acceptance. Specific pharmacological properties of marijuana (or any other drug) which might lead to a need or craving for other drugs have not been discovered. It would appear that dynamic and changing social and personal factors play the dominant role in the multi-drug-using patterns reported, and that the specific pharmacology of the compounds involved is secondary. Other aspects of this topic are discussed in Appendix C Extent and Patterns of Drug Use.
AN OVERVIEW OF METHADONE AND LONG-ACTING METHADONE DERIVATIVES
Introduction
In light of the recent rapid expansion in the medical and non-medical use of methadone in North America, a separate overview focussing on certain pharmacological aspects of methadone and its derivatives is presented here. Some redundancy with the general opiate narcotic discussion above is unavoidable.
Methadone was first synthesized in Germany during World War 11.109 Certain derivatives of methadone, including /-alpha acetylmethadol (also called methadyl acetate or LAM) and dl.-alpha acetylmethadol, have similar but longer-lasting pharmacological effects and are currently being investigated as possible substitutes for it.104, 116, 118, 238 Since the effects of these drugs are similar, the following discussion will focus primarily on the more widely used methadone, and the specific derivatives will be referred to when distinctions are appropriate.
Methadone which appears on the illicit market is usually diverted from legal sources, primarily by opiate narcotic-dependent persons who sell a portion of their prescribed medication, or from pharmacy, hospital and other thefts. The illicit manufacture of methadone in clandestine laboratories in the United States has been reported,9° but the current magnitude of such supplies has not been established. No illicitly produced methadone has been identified in Canada. Only limited quantities of the longer-acting methadone derivatives are available through licit channels in North America, and little or none appears to have reached the illicit market.
Although the majority of persons dependent on methadone have become regular users through medical treatment of their heroin use, as noted earlier, a number of "primary methadone addicts" have been identified in Canada, who have not used heroin or other opiate narcotics.", 87
Medical Use
Methadone has clinical properties that are qualitatively similar to morphine and other opiate narcotics. It relieves all types of pain, inhibits coughing, and slows gastrointestinal contractions (thereby relieving diarrhea), and has been used medically for these purposes.13 More recently, methadone has become important in facilitating opiate narcotic withdrawal and as a substitute for heroin in the long-term medical management of opiate narcotic dependence.", 88. 83, 119 The longer-acting methadone derivatives are currently being investigated as alternatives or supplements to methadone.104, 116, 118, 239
Administration, Absorption, Distribution and Physiological Fate
Methadone is available in solution for injection or in tablets and liquid forms intended for oral use. Taken orally, it retains a considerable degree of effectiveness, including toxicity at high doses. In contrast, morphine and heroin are considerably less effective by the oral route than when injected. Consequently, methadone is commonly given orally in medical use, and may also be taken by mouth by persons who use the drug illicitly but wish to avoid injections.113 The long-acting methadone derivatives are also effective when taken orally. In fact, the psychological and physiological effects of /-alpha acetylmethadol appear more quickly by the oral route than by injection: oral administration results in a 1-11 hour delay in onset while intravenous or subcutaneous injection results in a delay of 4-6 hours or longer. The racemic mixture, dl-alpha acetylmethadol (but not 1-alpha acetylmethadol) may result in severe burning, aching and pain after subcutaneous injection.72
Metabolism occurs primarily in the liver and excretion is mainly via urine, although under certain conditions significant excretion in perspiration may occur.m° Methadone is detectable in blood, urine, and other body fluids with standard techniques, and because of its slower metabolism and excretion, it can be detected for considerably longer periods after use than is the case with morphine and heroin. Immunoassay techniques have been developed for methadone.'"
Effects, Tolerance and Dependence
The acute psychological effects of methadone depend on dose, mode of administration and the individual's past history of opiate narcotic use. When these factors are taken into account, the acute psychological effects of methadone can be very similar to the effects of other opiate narcotics, but are of somewhat longer duration.'", 1" For example, the immediate effects of intravenous injections of this drug may not be clearly discriminable from intravenous injections of morphine or heroin. All three can result in a 'rush', euphoria, drowsiness, nausea, dizziness, relief of or indifference to pain, and so forth. The long-acting methadone derivatives also result in distinct morphine-like effects; /-alpha acethylmethadol is different only in that intravenous injection of this drug does not produce an initial 'rush', and its effects have 4-6 hour delay in onset.72
With large and progressively increasing doses of methadone injected regularly over a period of several weeks in an experimental situation, individuals are reported to become less active and may spend a great deal of time in bed in a pleasant dreamy state with alternating periods of somnolence and wakefulness Con the nod' or `coasting'); personal appearance may become neglected, and performance on cognitive and psychomotor tests may be slightly impaired."9 This behaviour is reported to be strikingly similar to that observed when morphine is used under comparable conditions.
The acute physiological effects of methadone are, similarly, not substantially different from those of other opiate narcotics."9. "9 For example, there may be slowing of EEG waves, loss of appetite, slight elevation of blood sugar level, sexual impotence, constriction of the pupils, sweating and reduced respiration. The latency, intensity and duration of these effects may vary between the drugs, but for the most part the differences appear to be quantitative, not qualitative.
Although methadone has a high dependence liability of the morphine type, it is now frequently used in the medical management of chronic opiate narcotics dependence.", 93' 119 When a constant dose of methadone is given orally at daily intervals, most of the acute psychological and physiological effects of the drug gradually become minimal or absent as tolerance develops. Tolerance to methadone develops substantially slower than to morphine or heroin, but after tolerance has stabilized, clinical observers reportedly cannot distinguish individuals given such treatment from non-treated normal controls.
Many persons on methadone maintenance are able to perform well in school and at a wide variety of jobs requiring different intellectual and motor skills. Many of these individuals drive automobiles regularly, and some drive trucks and cars in the course of their employment.171, 172 So far there is no evidence of significant traffic hazards resulting from these practices. In fact, an improvement in driving records has been reported in some former heroin users after joining methadone maintenance programs.22• " However, there is relatively little systematic data available dealing with the effects of chronic methadone use on intellectual and cognitive functioning, perceptual and sensory ability, and driving and other psychomotor skills. The existing data do not provide grounds for much concern, but considerable additional research is needed in these areas.55, 58, 85, 104, 106 Of particular importance are possible interaction effects with alcohol, cannabis, and other commonly used licit and illicit drugs.
Because of cross-tolerance, when methadone tolerance is sufficiently high, subsequent injections of formerly active doses of heroin or other opiate narcotics are relatively ineffective in producing a 'high' or `rush'; this effect has been called "narcotic blockade".55, 57 In addition, daily administration of methadone is effective in forestalling the onset of the withdrawal syndrome associated with regular use of heroin. Potentially therapeutic aspects of this maintenance of cross-tolerance and cross-dependence include: the reduction of the acute pleasurable, reinforcing effects of opiate narcotics which are of importance in the development and continuation of dependence; the elimination of the need to procure illicit drugs in order to avoid the withdrawal syndrome; the reduction of the sedation and consequent behavioural impairment that may accompany the acute 'high'; the elimination of the `craving' for heroin often described by heroin users and former users; and the reduction of the secondary complications which usually follow regular intravenous injection of illicit materials.
Other opiate narcotics, including heroin, morphine or pethidine could, in principle, be given orally and in constant doses to produce a similar effect. Methadone, however, has two important properties which make its use more practical. First, it is quite effective when taken orally as compared to injections. Second, it is necessary to administer methadone only once every 24 hours in order to avoid the onset of the withdrawal syndrome. The long-acting derivatives can be administered at intervals of 48 hours or longer with the same result, and for this reason they are being investigated as possible substitutes for methadone. Heroin or morphine must be administered several times daily in order to avoid withdrawal symptoms in dependent users. Since patients may be required to go to a clinic for each drug administration, minimizing the frequency of such visits is of considerable therapeutic and economic significance. There does not appear to be any data from controlled experiments to verify the assumption that the direct effects of methadone maintenance are superior to maintenance on other opiate narcotics, however. Similarly, the relative effectiveness of oral versus intravenous administration of methadone in certain maintenance situations has not been systematically explored and is presently the subject of some controversy.
Although most acute psychological and physiological effects of methadone become minimal or absent with daily administration of constant doses, tolerance to some effects does not appear to develop in many individuals.58, 83, 108, 114, 165 Although conflicting opinions exist regarding the degree of euphoria typically produced by methadone under oral maintenance conditions, it is now generally accepted that methadone may reduce anxiety and depression, and may produce a sustained feeling of improved well-being, but not the intense peak euphoria which is characteristic of heroin and morphine. Some symptoms commonly reported to persist include constipation, excessive sweating, impotence and difficulty achieving orgasm, drowsiness and feeling `loaded'. Patients also report that methadone frequently does not prevent the appearance of withdrawal symptoms over the entire 24-hour interval between administrations. The long-acting derivatives have not been as extensively studied as methadone, but some similarities in side effects such as sweating, impotence and constipation, and some differences including less sedation and euphoria and fewer abnormal EEG's have been reported in some instances.104 A cumulative toxicity sometimes occurs with the long-acting derivatives, and it has been reported that subjective amphetamine-like effects, dysphoria, acute psychosis and other toxic reactions may develop after the drugs have been used in high doses for one or two weeks.72, 84. 118
The side effects frequently reported by patients in methadone maintenance programs are related to the magnitude of the dose administered. In one study, it was found that during the first three months of treatment, patients given a high (100 mg) or moderate (50 mg) dose reported more side effects than patients receiving only 30 mg/day.83 The differences were not pronounced, however, and might be expected to decline if tests were continued for a longer period. On the other hand, the 30 mg group showed more evidence of withdrawal effects, occurring primarily in the evening, eight or more hours after receiving the daily dose. Low maintenance doses have also been shown to be more likely to result in transient illicit heroin use; but no dose differences have been found in the number of patients remaining in treatment, their employment, arrest rate, or their use of other drugs.83, 118 So far there has been no systematic investigation of the effect that dose and duration of treatment might have on the ease and success of future methadone withdrawal and overall opiate narcotic abstinence. In Canada, methadone doses employed cover a wide range (approximately 25-150 mg), and until careful, long-range studies have been conducted, the optimal range remains unknown.
The number of medical or behavioural complications seen in individuals dependent on illicit opiate narcotics typically decreases following long-term maintenance on methadone. Changes which have been reported include: fewer infections, more regular menstrual function in females, decreased automobile driving violations, fewer physical complaints, less insomnia, an improvement in mood, reduced non-drug criminal behaviour, and increased employment.", 83. 227 Weight gain is often reported by persons on methadone maintenance. Such changes are probably the result of a number of factors, making it difficult to determine possible differences between the effects of the previously used opiate narcotics and associated illicit heroin-dependent life style, and the direct effects of methadone. Like morphine and heroin, there is little evidence of direct permanent physiological damage due to chronic use of methadone.112 Most of the complications seen in non-medical use are attributable to secondary factors such as nutrition, hygiene or the use of other drugs; other effects appear to be reversible upon cessation of methadone use. Considerably more research on the chronic physical effects of long-term use of methadone and its long-acting derivatives is necessary.
Babies born to mothers dependent on methadone frequently demonstrate withdrawal symptoms and may require hospitalization for several weeks.20, 21, 227, 240 Low birth weights have also been reported, but it is not known if this and other complications are due to the methadone or to other factors such as inadequate nutrition, poor hygiene and the heavy use of other drugs like tobacco. Babies born to mothers dependent on heroin have similar difficulties, and at present, the possible differences between the drugs in this regard are not well established. No congenital abnormalities have been linked with methadone.
At sufficiently high doses, methadone, like other opiate narcotics, produces coma, shock, respiratory arrest and death. Secondary complications, possibly leading to death, can result from the injection of insoluble materials, such as talc or chalk, which are present in preparations intended for oral use.7, 204
The nature and intensity of the abstinence syndrome which results when regular methadone administration is abruptly discontinued depends, as with other opiate narcotics, on dose and frequency of use.105 At low doses the abstinence syndrome may be minor or even absent. At high doses the abstinence syndrome is detectable in 1-3 days following cessation of use, after which the intensity and number of withdrawal symptoms build up gradually over a period of about a week and then fall even more gradually, with certain symptoms such as weakness, fatigue, aching and insomnia possibly lasting up to six weeks or longer. With the long-acting methadone derivatives the abstinence syndrome is similar but develops even more slowly, but, so far, observations in man have been continued for only two weeks following cessation of use—in this period the intensity of the withdrawal syndrome did not begin to recede.72
Because of its relatively slow metabolism and excretion, the methadone abstinence syndrome is quantitatively and in some ways qualitatively different from that associated with morphine or heroin. As noted earlier, with the latter drugs the acute effects pass more quickly, and the abstinence syndrome appears in half a day or less, reaches its peak intensity after 1-3 days of abstinence, and gross recovery occurs in 7-10 days. The maximum severity of withdrawal is considerably greater with the shorter-acting opiate narcotics than with an equivalent cross-dependent dose of methadone. As a result, methadone may be useful in withdrawing individuals heavily dependent on heroin or morphine. By substituting an equivalent dose of methadone, the subsequent withdrawal syndrome is, at its peak, considerably more bearable and manageable, although distinctly longer in duration.1°2 On the other hand, since the heroin withdrawal symptoms most often seen in Canada today are relatively mild, substituting high doses of methadone for heroin may result in a more intense and prolonged withdrawal syndrome than would otherwise have been the case. It has been noted that prolonged withdrawal, even if less severe, may be more aversive to some individuals than a more intense abstinence syndrome of shorter duration.
Some individuals who have had experience in methadone maintenance programs have complained that the withdrawal from methadone can be much worse than that experienced with illicit heroin. This apparent paradox may be partly explained if typical patterns of illicit opiate narcotic use are compared with the regular daily administration of heavy methadone doses. Even regular heroin use in North America is apparently much more of an intermittent practice than was once realized. Very few persons can afford regular daily high-dose heroin use, and many may have developed a relatively mild tolerance and physical dependence prior to beginning methadone maintenance. In fact, an individual can, in many parts of North America, enter methadone maintenance without actually having any prior physical dependence. (Note that a single "positive urine" for opiate narcotics is not adequate evidence of regular heroin use or dependence.) However, once established in a maintenance program, the patient is assured a continual daily high tissue level of methadone, designed to produce considerable tolerance and physical dependence. In other words, all individuals on methadone maintenance are solidly dependent on opiate narcotics, often to a much greater and more regular degree than they had been previously when they had to acquire an illicit drug on the street or do without. Consequently, some such individuals are liable to experience a more severe withdrawal from methadone if they quit abruptly. The methadone withdrawal syndrome is milder than that associated with heroin dependence only if equivalent doses which produce comparable tolerance and physical dependence are involved. Unfortunately it is presently difficult to accurately determine the extent of prior opiate narcotic use and dependence in individuals applying for methadone maintenance.
Although methadone is an effective analgesic in acute use, individuals on methadone maintenance experience adequate aversive response to normally painful stimuli. In spite of significant cross-tolerance, pethidine or morphine are apparently effective in relieving pain from serious injury, disease, or medical surgery in methadone-dependent persons. In addition, chronic methadone use does not seem to cause major complications to surgical anesthesia.58
OPIATE NARCOTIC ANTAGONISTS
There are a large number of drugs available which block or counteract the effects of opiate narcotics in varying degrees. Most of these compounds have some morphine-like or other activity of their own, while a few are relatively pure antagonists and lack significant direct pharmacological effect. Many of these antagonists have been derived by chemically altering some aspects of natural or synthetic opiate narcotic molecules. Among the best known antagonists are cyclazocine, naloxone, nalorphine (Nalline®), and levallorphan. Cyclazocine was the first narcotic antagonist to become important in clinical work, and is the best studied and understood of these compounds. Some promising newer antagonists which are under clinical investigation are levo-BC-2605 (synthesized by Bristol Laboratories of Canada), EN 1639A, and M-5050, a thebaine derivative.29, 35' 113' 137, 151' 153, 221 Immunization approaches to narcotic antagonism are also being explored employing antibodies originally developed for immunoassay of opiate narcotics in body tissue and fluid.17
In sufficient dose antagonists can block the psychological and physiological effects of opiate narcotics, including the development of tolerance and physical dependence, and can reverse or prevent toxic effects of opiate narcotic overdose. The antagonists produce their blocking effects without altering the metabolism or excretion of opiate narcotics. It is generally thought that they competitively block the active drug molecule at its receptor site of action. If a short-acting antagonist were used in the treatment of an overdose of a longer-acting drug, such as methadone, repeated administration of the antagonist would be necessary for the duration of time that the methadone would normally have been active. If only a single antagonist dose were given, the patient could relapse into a toxic state after initial recovery, as soon as the antagonist effects began to dissipate? As noted earlier, antagonists can precipitate an intense acute withdrawal syndrome in opiate narcotic-dependent individuals, and this property is sometimes employed for identifying physically dependent persons for medical and legal purposes.113
Cyclazocine may be administered orally, subcutaneously or intravenously. Oral administration has been preferred when the drug is to be administered regularly. Naloxone and nalorphine are 30-100 times more effective when injected and are usually given subcutaneously. This feature has led to the development of a methadone-naloxone combination which may be used in the future to discourage the injection of methadone meant for ingestion only: taken orally, as directed, the methadone is effective but the antagonist is not; taken by injection, the methadone is rendered ineffective by the antagonist and, further, an intense withdrawal syndrome is rapidly precipitated in a dependent individual. 44, 122
Variations in absorption, distribution, metabolism and excretion are responsible for many of the differences in potency and duration of action among the antagonists. While the duration of action depends to some degree on the particular effect being measured, at sufficient doses cyclazocine, levoBC-2605 and EN 1639A can be effective for 24 hours; typical doses of naloxone or nalorphine are usually effective for less than 6 hours 44, 115, 146, 151' 239 In order to obtain longer-lasting antagonism, certain salts and esters of cyclazocine and naloxone have been synthesized, resulting in an increase in their durations of action by a factor of about 10. In addition, subcutaneous injections of a lightly granular partly biodegradable plastic permeated with cyclazocine has been shown to suppress the effects of morphine in dogs for more than a week.'51 Other vehicles or antagonist carriers include surgically implanted polyethylene film and polylactate matrices.153 A relatively pure antagonist which is slowly released from implanted biodegradable material, providing effective opiate narcotic blockade for a month following administration, may be available for testing in humans in the near future.'"
Cyclazocine has been used clinically in regular, daily doses in opiate narcotic-dependent individuals in order to discourage their use of such drugs."5, 239 It is thought that ineffective attempts to use opiate narcotics diminish and possibly extinguish the individual's learned opiate narcotic-seeking behaviour and conditioned abstinence symptoms, both of which may result in relapse to opiate narcotic use. This treatment approach may be used more widely when longer-acting antagonists are refined. However, antagonists do not block the craving or hunger for narcotics often reported in persons dependent on morphine-like drugs, nor do they ease the tension or depression frequently noted in such individuals. Consequently, relatively few patients are willing to be maintained on antagonists.
One difficulty with cyclazocine maintenance is that the drug has some direct effects of its own: for example, it has mild analgesic properties, and can produce mental clouding, sensory distortions, hallucinations and a variety of physical symptoms such as constipation, headaches, muscle twitches, and difficulty focussing the eyes. However, tolerance develops to most of these effects with chronic use.113. 137 Some degree of physical dependence on cyclazocine or nalorphine can also develop. High doses of levo-BC-2605 result in some side effects, but they are considerably less significant than those produced by cyclazocine or nalorphine at comparable antagonistic doses.", 146 EN 1639A, in contrast, is a more "pure" antagonist, producing few or no discernible side effects at doses providing effective morphine blockade.'" Naloxone is also a relatively pure antagonist but its short duration of action and high cost limit its usefulness. The Bristol (BC series) antagonists have advantages in that they are synthesized entirely from petroleum products (most other antagonists require some opium material) and are very inexpensive.29. 44 Any chronically effective antagonist has the potential disadvantage of preventing the effective legitimate medical use of opiate narcotics as well as non-medical use.
There is no evidence that regular administration of opiate narcotic antagonists results in any permanent psychological or physical effects. Clinical experience with these drugs is limited, however. Human deaths due to overdose of antagonists have not been reported. Fatal levels of cyclazocine have been reached in animals, but it does not appear that lethal toxicity is a significant risk with use of antagonists.









